Abstract
Objective: To describe the epidemiological, clinical and economic changes that occurred in the HIV epidemic in Italy prior to and after the introduction of highly active antiretroviral therapy (HAART).
Design: A prospective, observational, multicentre case-control study was conducted comparing data, collected over 6 months, from an AIDS cohort in 1998 with that of a cohort in 1994. Out of 77 patients with AIDS in the 1998 cohort, 74 survived. These 74 patients were matched for severity of illness with 74 patient survivors from the 1994 cohort to enable valid comparisons of mortality, disability-dependency (DD), health-related QOL (HR-QOL), and direct costs.
Results: Overall, a considerable difference was observed in mortality (33.8% in 1994 vs 3.9% in 1998) between unmatched patients of the two cohorts. As for matched patients, the number of hospital admissions was 1.7 in 1994 and 0.8 in 1998; the average length of stay was 28.1 days in 1994 and 12.6 days in 1998. The direct cost per patient per year was €15 390 and €11 465 for the 1994 and 1998 cohorts, respectively (1999 values). The 1998 patient cohort had significantly better HR-QOL at 6 months in two domains of the instrument used (emotional reaction and energy) and the percentage of totally dependent patients was significantly lower compared with the 1994 cohort (1.4% vs 6.8%).
Conclusions: This is the first study to present a comprehensive comparison of direct costs, DD and HR-QOL of patients with AIDS between two time periods. The use of a case-control design has enabled changes in costs and outcomes to be linked to the introduction of HAART in Italy in 1997.
Similar content being viewed by others
Infection with HIV is a chronic disease that results in a progressive deterioration of the immune system, secondary neoplasms or opportunistic infections and, eventually, death. During the 1990s, HIV became a major cause of death, not only in many developing countries where the effects were most dramatic, but also in developed countries.[1]
Since 1996, the introduction of new classes of antiretroviral drugs, such as protease inhibitors and non-nucleoside transcriptase inhibitors, and improved techniques for monitoring therapeutic effectiveness and disease progression have radically changed the natural history of HIV. The use of combination therapy with at least three potent antiretroviral drugs (highly active antiretroviral therapy [HAART]) has reduced morbidity and mortality.[2,3]
Several reports have documented a shift in HIV/AIDS health service utilisation from inpatient to outpatient care in developed countries after the introduction of HAART.[4–6] The use of drugs for the treatment of opportunistic infections has also reduced.[7] Reductions in hospitalisation costs in developed countries have been associated with the fall in AIDS-related morbidity and mortality.[8] Increased patient survival and reduced morbidity also increases the chance of individuals with HIV contributing to society and the economy through participation in paid or unpaid work, although in some cases the adverse effects of treatment may restrict this potential.
Allied to changes in morbidity, effective HAART regimens may deliver improvements in disability-dependency (DD) levels and health-related QOL (HR-QOL). However, quantifying such improvements is difficult and empirical studies are lacking. Ideally, an evaluation of the effectiveness and cost effectiveness of HAART used in clinical practice would involve a pragmatic controlled trial to compare the impact on healthcare costs and QOL outcomes for patients receiving HAART versus those not receiving HAART. Such a study is costly and may be problematic to design and set up, hence a practical ‘next best’ solution would be to make use of prospective observational data.
This paper reports on a multicentre observational study comparing the same patient healthcare costs and outcomes for two groups of patients with AIDS (1994 and 1998 cohorts) from centres in Northern Italy prior to and after the introduction of HAART. There are well known limitations associated with the use of observational study designs, in particular the potential for confounding factors producing bias in results.[9] However, the availability of cost and outcome data prior to HAART provided a unique opportunity for the 1994 cohort to represent a historical control group for comparison with a group after the introduction of HAART.
Methods
Study Design
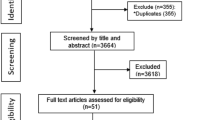
This study used data from two AIDS patient cohorts from 1994 (the historical control) and 1998. The 1994 cohort consisted of data from a multicenter, prospective, observational study conducted in ten AIDS clinics in North East Italy. This study was replicated and updated in 1998 in 34 AIDS clinics in the same region.[10] To estimate the impact of HAART on the treatment and care of patients with AIDS, a ‘before-and-after’ approach, based on a case-control study design, was adopted. The 1994 and 1998 patients were matched across the two cohorts.
Eligibility Criteria
Clinical eligibility criteria were the same for the two cohort groups. The studies enrolled patients with AIDS aged 18 years and older, followed for at least 6-months. Time of enrolment for both cohort groups was at the first visit in the study period at a participating inpatient or outpatient AIDS clinic. For enrolment in 1998, patients were required also to be HAART-naive (but allowed to have taken dual or monotherapy) and be starting on a HAART regimen that included the protease inhibitor indinavir. Most HAART regimes for Italian patients include a protease inhibitor.[11] We focused only on indinavir combinations to avoid the confounding effect of toxicity from other protease inhibitors on HR-QOL. The triple HAART regimen could also include the following non-nucleoside reverse transcriptase inhibitors: zidovudine, lamivudine, stavudine, didanosine and zalcitabine.
Patient Follow-up
The length of patient follow-up was the same for both groups. Data were collected at enrolment (AIDS notification [1994] or initiation of HAART [1998]) and at 3- and 6-month follow-up visits. Information collected included job status (i.e. employed, unemployed, not participating in the labour force, student), clinical information (i.e. CD4+ cell count, severity of illness and mortality), healthcare resource use (HRU), direct medical costs, dependency and HR-QOL.
Patient-Related Data
For HRU, the hospital admissions, length of inpatient stay, day care contacts, outpatient contacts, surgical interventions, consultations, diagnostic procedures and pharmaceutical use were recorded.
HR-QOL was measured by the Nottingham Health Profile (NHP). An Italian version of the NHP has been validated and the weights and standard values are available specifically for Northern Italy.[12] The NHP is a self-administered questionnaire designed to measure perceived health problems. It is a generic measure of HR-QOL that consists of 38 questions covering six aspects of HR-QOL: energy, pain, emotional reactions, sleep, social isolation and physical mobility. Its use is appropriate for people aged 16 years and older as an outcome measure for group comparison or to monitor the subjective health of chronically ill patients. The range of the global score is 0 for the best (full health) and 100 for the worst condition (or death).
Dependency was defined as “a state in which an individual is reliant upon other(s) for assistance in meeting recognised needs”.[13] Data on dependency were collected by trained medical or nursing personnel. DD measures included the following elements: ability to walk (inside/outside the home), shop, dress, eat, bath, level of incontinence and dementia. Six stages of DD were classified according to the severity of the above mentioned elements. The presence of AIDS-dementia complex (ADC) was considered as representative of the greatest level of dependency.
Severity of disease has been shown to be a relevant predictor of both healthcare costs and HR-QOL.[14] Severity of illness was classified using the Severity Classification System for AIDS Hospitalisation (SCSAH).[15] This measure includes all opportunistic and secondary neoplasms according to the Centers for Disease Control and Prevention AIDS definition with the inclusion of three specific conditions (haematologic disorders, non-opportunistic infections, organ failure, e.g. cirrhosis). The classification system grouped patients with AIDS into three main stages, each with an associated resource utilisation and inpatient mortality rate (i.e. lowest in stage 1, highest in stage 3). Stage 1 included conditions with a more favourable prognosis (e.g. Kaposi’s sarcoma, oesophageal candidiasis). Stage 2 included Pneumocystis-carinii pneumonia. Stage 3 included organ failure, cerebral opportunistic and systemic infections and ADC. The SCSAH has been used previously in different AIDS populations to describe variations in resource use and outcomes of hospital care according to severity of disease.[16]
Costing
Cost estimation was based on the actual recorded physical units of HRU (e.g. number of x-rays, packs of medicine) for each individual patient multiplied by a unit cost as follows:
-
Costs of medicine were calculated as 50% of the published market price, representing the official selling price to hospitals in Italy.
-
Costs of diagnostic examinations were based on national tariffs.
-
Average costs of a hospital day and an outpatient visit were calculated by dividing the total staff salaries for each AIDS centre by the total number of hospital days and outpatients visits. Because of the large number of AIDS clinics participating and the heterogeneity of accountability systems in these hospitals, it was not feasible to include an element for overhead costs such as capital and general services. Therefore, the costs per patient per year may be under estimations of the actual costs.
All costs were initially expressed in lira (1998 values) and then converted to euros (1€ = 1936.25 lira. Costs obtained in 1994 were actualised to 1998 using the official inflation rate reported by the Italian National Institute of Statistics. The official inflation rate was 5.4% in 1995, 3.9% in 1996, 1.7% in 1997 and 1.8% in 1998 (on average 3.2%).
Comparative Design
The comparative study design was based on a set of assumptions: (i) SCSAH and CD4+ cell counts are predictive of clinical progression, health resource use and costs; (ii) both groups of patients had previously received mono- or dual antiretroviral therapy; (iii) prophylaxis for opportunistic infections continued after enrollment; (iv) quality of care was assumed not to have changed between 1994 and 1998; and (v) the main difference between the two cohorts affecting clinical progression was the use of HAART in the 1998 group. However, other factors may have influenced clinical progression in the two groups. In particular, patients enrolled in the 1994 cohort demonstrated greater levels of sickness (more fever, weight loss, anemia). In order to reduce the potential differences in severity of ill-health at baseline, prior to matching we excluded all patients in the two groups who had died during the follow-up period. As mortality was much higher in the 1994 group we felt this exclusion was sufficient to counterbalance the effect of other possible factors influencing clinical progression during the 6-months follow-up.
For each surviving patient with AIDS enrolled in the case group, a match from the control group was identified. The primary matching criterion was the disease stage and CD4+ cell counts (CD4+ counts within 10 cells/mm3). If two or more patients matched on these criteria, age was then used as additional matching criterion.
Statistical Analysis
Chi-square and t-test were employed to test for associations in comparing the two populations. A paired t-test was used to evaluate the significance of the differences in the outcome variables, for which 95% confidence intervals were also computed. All statistical tests were 2-tailed; results with a p value of <0.05 were considered significant.
Results
Baseline Characteristics
A total of 251 patients with AIDS were enrolled in 1994 and 77 were enrolled in 1998. During the 6-month follow-up, 85 (33.8%) of the 251 patients with AIDS in 1994 died. From the 1998 group, 3 (3.9%) out of 77 patients died. Therefore, after the exclusion of patients who died, the remaining 74 patients in the 1998 cohort were matched to 74 patients out of the 166 patients with AIDS alive at the end of the follow-up in the 1994 cohort. Because of the study design comparing only surviving patients in the 1994 group with the overall 1998 control group, the comparison of mortality data was possible only between the two overall cohorts (unmatched patients). Table I describes the socio-demographic and clinical characteristics of the 1994- and 1998-matched patients with AIDS at enrolment.
Compared with patients in the 1994 study, the 1998 patients with AIDS were on average older, more likely to be heterosexual and less likely to be an intravenous drug user. These differences are consistent with the changes that have been reported in the epidemiology of HIV infection in Italy during the period considered.[11] In 1994, after 6-months’ follow-up, the baseline average CD4+ cell count decreased in the matched 74 patients from 143.4 to 110.1 cells/mm3. In contrast, the average CD4+ cells count among 1998 patients increased from 160.0 to 253.9 cells/mm3. After 6-months’ follow-up, we also observed a significant decrease of HIV-RNA viral load in the 1998 patients compared with baseline (from 211 739 to 35 057 copies/mL [p > 0.01]). Data on HIV-RNA viral load were not available for 1994 patients since this test was only introduced into clinical practice in 1997.
Table II describes the use of healthcare resources and the direct medical cost of care for patients with AIDS in 1998 and their matched counterparts in 1994. The numbers of hospital admissions per patient per year were 1.7 and 0.8 in the 1994 and 1998 cohorts, respectively. The numbers of hospital days were 28.1 per patient per year in 1994 and 12.6 days in 1998. The number of outpatient visits was lower in the 1998 cohort. The average direct medical cost per patient per year was estimated at €15 390 and €11 465 for the 1994 and 1998 cohorts, respectively. Drug costs accounted for 63.5% of total direct medical costs in 1998, compared with 12.8% in 1994, whilst inpatient and outpatient costs were 36.5% of the total in 1998 compared with 78.5% in 1994, reflecting a shift of healthcare resource use from inpatient and outpatient care to antiretroviral therapy.Footnote 1
Evaluation of Disabilities/Dependency Measures
Table III presents the dependency levels of surviving patients with AIDS in 1994 and 1998. Compared with the patients who survived 6 months’ of follow-up in 1994, the 1998 patients were more likely to be fully independent (90.5% vs 86.5%) at baseline. At the end of the 6-month follow-up period, 1.4% of patients in the 1998 study were in dependency stage 6 (confined to bed, mental deterioration or ADC) compared with 6.8% of the 1994 surviving patients.
Health-Related QOL Among Surviving Patients
Because of matching, the two groups had the same distribution of patients across SCSAH disease stage (stage 1: 63.5%; stage 2: 25.7%; stage 3: 10.8%), with similar CD4+ counts at enrolment (143.4 cells/mm3 [1994] vs 160.0 cells/mm3 [1998]; p > 0.05).
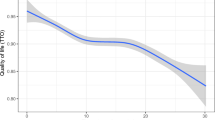
Figure 1 reports the baseline HR-QOL levels as measured by the Nottingham Health Profile in the 1994- and 1998-matched cohorts. The 1998 patients with AIDS had better HR-QOL at baseline in all domains except sleep. Figure 2 presents the changes in HR-QOL between baseline and 6 months’ follow-up for both cohorts. On average, AIDS patients surviving the 6-month follow-up in the 1998 group had significantly better HR-QOL in energy and emotional domains compared with the 1994 cohort but no differences were observed between cohorts in other domains (i.e. sleep, social isolation, mobility and pain). Patients with AIDS in the 1994 cohort had no change in any HR-QOL domain at the end of the 6-month follow-up compared with their levels at baseline.
Health-related QOL (HR-QOL) scores at enrolment; mean values and 95% confidence intervals for each Nottingham Health Profile dimension in the 1994 and 1998 samples. Mean values between 1994 and 1998 samples were statistically significant (p < 0.05) in all domains except sleep. EM = emotional reactions; ER = energy; MB = mobility; PN = pain; SC = social isolation; SL = sleep.
Mean values and 95% confidence intervals of the health-related QOL (HR-QOL) differences between baseline (AIDS notification [1994] or initiation of highly active antiretroviral therapy [1998]) and 6-months’ follow-up for each Nottingham Health Profile dimension in the 1994 and 1998 samples. EM = emotional reactions; ER = energy; MB = mobility; PN = pain; SC = social isolation; SL = sleep. * p < 0.05 vs 1994 sample for mean values.
Discussion
The scientific and epidemiological nature of the HIV epidemic and its clinical management and treatment patterns have been constantly evolving over the past two decades. Hence, estimation of the medical costs of care and evaluation of the cost effectiveness of treatment and care options has been defined as a ‘moving target’.[17] The cost effectiveness of HAART versus dual therapy has been modelled using clinical trial data for treatment effect, with the general conclusion being that HAART is cost effective.[18–20] An Italian study using observational data on 483 patients treated between 1997 and 1998 reported that 30% to over 80% of patients were prescribed HAART, according to CD4+ cell count group.[21] This study also reported lower hospital days than previous estimates for Italy, the authors claiming this indicated a shift in costs from hospitalisation to HAART.
In our study, by comparing a sample of patients treated in 1994 with a sample treated in 1998 and by adjusting for major confounders such as disease severity, CD4+ cell count and (if necessary) age, it has been possible to assess the likely impact that new antiretroviral therapy (HAART), introduced in the region in 1997, has had on medical costs and patient outcomes. We observed a number of differences in outcomes between the two cohorts. Compared with the 1994 cohort, in 1998 there was a major reduction in mortality. Allied to this there was evidence of a major shift in healthcare costs from inpatient and outpatient care to greater expenditure on antiretroviral therapy in 1998, but with a net overall decline in medical costs. Therefore, it appears from our study that despite the extra costs associated with the use of HAART there is the potential in developed healthcare systems for a large cost offset from a reduction in hospital utilisation by patients with AIDS. These results are consistent with those published by other investigators who have reported a significant decrease of non-opportunistic infections (e.g. bacterial pneumonia) and the most common opportunistic infections,[22] and a downward trend in the incidence of admissions and time spent as inpatients after the introduction of effective antiretroviral therapy.[23] A similar pattern of resource utilisation to that found in our study for 1994 was reported in an Italian national survey conducted in 1993.[24] The shift from inpatient and outpatient utilisation was also documented in another national study conducted after the introduction of HAART in 1997.[25]
Furthermore, the 1998 cohort had far fewer severe and total disability days than the 1994 cohort. The expectation is that this is likely to be associated with reduced indirect costs from fewer days off paid work and other unpaid but productive activities, although this was not specifically measured in the study. However, it is likely that combined with reduced healthcare costs, the total economic benefits of HAART therapy far outweigh the direct incremental costs of the drug treatment.
Finally, HR-QOL is paramount to patients and the primary concern of the patient who seeks medical care. Compared with the 1994 cohort, in the 1998 cohort we observed a higher baseline HR-QOL score using the NHP for all NHP dimensions except sleep. In addition, compared with baseline, patients with AIDS in 1998 had significantly higher scores at the end of the 6-month follow-up in two domains: energy and emotional reactions, whereas in the 1994 group, no statistically significant changes were observed over the 6 months.
The improvement in HR-QOL occurring shortly after the start of triple antiretroviral therapy has been demonstrated in many clinical trials,[26,27] but as far as we know this is the first study using an observational design to assess the impact of HAART in real-world settings. Many factors may have contributed to the observed improvement of health outcomes and the reduction in healthcare costs. For example, better nutrition and prophylaxis for opportunistic infections and physician experience in patient care may have made an important contribution in the improved outcomes. However, it is also likely that the introduction of protease inhibitors in Italy has had the most significant contribution in the reduction of hospital resource use, costs and improvement in HR-QOL.
Study Limitations
Study Design
Compared with the use of a randomised controlled trial (RCT) design in which one group of patients receive HAART and the other receives placebo or no HAART, there are limitations with the use of an observational study design with historical controls such as the one in this study. Our observational study is subject to greater threat from bias due to the effect of differences between the cohorts in variables such as level of illness, and the potential changes in quality of care over time. Also, in addition to HAART, other health and social care interventions could be responsible for some of the differences found in resource utilisation and health outcomes. Nonetheless, whilst observational designs suffer from bias, if the intervention effect remains sufficiently large after accounting for major confounding factors, then it is likely that the intervention has had an impact on the outcomes being analysed.[28] In the study, the cost and health outcome differences between the two groups of patients with AIDS after matching were sufficiently large to provide a good level of expectation that HAART has had an impact on these outcomes.
The use of an observational study design may be preferred to an RCT if there is high importance attached to real-world relevance of the results. RCTs designed to measure efficacy are carried out under controlled circumstances and may fail to adequately reflect the treatment and care of patients in routine daily practice. It is possible to improve real-world relevance of RCTs by minimising the protocol-driven requirements, which particularly affects the accurate measurement of resource use consequences associated with an intervention. A pragmatic RCT would be most useful for addressing questions of which specific HAART regimens are most effective and cost effective to use in clinical practice (e.g. alternative quadruple or triple regimens), but these trials are costly, and take time to set up, recruit patients and to collect data. In addition, such a design may still result in some reduction in real-world applicability. In particular, clinicians do not randomise in actual practice, but show preferences in decisions of who to treat with which drugs.
Other Limitations
We were unable to measure the impact of long-term adverse events (such as lipodistrophy and diabetes) due to a limited follow-up time of 6 months. The enrolment of patients in a single HAART regimen including only indinavir combinations may be considered a further limitation, although this was felt necessary in order to reduce the confounding effect of different protease inhibitors on HR-QOL.
Finally, partly due to heterogeneity of accounting systems in the participating hospitals we could not obtain specific unit costs for an inpatient day or outpatient visit, but used total salary costs divided by number of days/visits to obtain an average cost for these resources. This approach excluded capital and other overheads/consumable costs; therefore, the costs are likely to represent a lower bound estimation of actual costs.
Conclusion
The introduction of HAART has coincided with lower costs and better clinical outcomes for the 1998 group compared with the 1994 patient cohort. Patients with AIDS in 1998 had better survival and better (or equal) HR-QOL scores. The total direct medical cost per patient per year was found to be lower in 1998 despite the increases in antiretroviral drug cost.
As far as we know, this is the first study to present a comprehensive comparison of direct costs, DD and HR-QOL for patients with AIDS using observational data and a case-control design. Although this study was conducted in a North Italian setting, the findings are generalisable to other developed healthcare systems and are consistent with results reported from other Western countries. This study can be viewed as providing useful information on the likely direction and magnitude of impact that HAART has had on AIDS care costs and patient health and HR-QOL outcome. It has relevance for future public health policies, particularly in those countries with a growing HIV epidemic who are facing decisions on the use of expensive HAART therapies in a resource-constrained healthcare environment.
Further research is needed to investigate whether since 1998 a steady state has been reached in healthcare costs and patient outcomes and if HIV can still be regarded as a ‘moving target’ in this context. In addition, although this study has employed a case-control approach to investigate the potential impact of HAART it has not been possible to conclusively assess whether HAART is cost effective. Formal economic evaluation is required, potentially alongside a pragmatic RCT, to investigate further hypotheses of the cost effectiveness of specific HAART regimens. Interestingly, the changing impact of HIV at the individual patient level could have implications at the population level. For example, an epidemiological implication of lengthened survival and better HR-QOL could be an increased prevalence of at-risk behaviour (and related increases in epidemics). Further research is required to address issues such as these.
Notes
Data on therapy history (monotherapy or dual therapy) were not available for 1994 patients.
References
Hanvelt RA, Ruedy NS, Hogg RS, et al. Indirect costs of HIV/AIDS mortality in Canada. AIDS 1994; 8: 7–11
Mouton Y, Alfandari S, Valette M, et al. Impact of protease inhibitors on AIDS-defining events and hospitalisations in 10 French AIDS reference centres. AIDS 1997; 11: 101–5
Patella FJ, Delanee KM, Moorman AC, et al. Declining mor-bidity and mortality among patients with advanced human immunodeficiency virus infection. N Engl J Med 1998; 338: 853–60
Gebo KA, Chaisson RE, Folkemer JG, et al. Costs of HIV medical care in the era of highly active antiretroviral therapy. AIDS 1999; 13: 963–9
Keiser P, Kvanli MB, Turner D, et al. Protease inhibitors therapy is associated with decreased with HIV related health care costs in men treated at a Veteran Administration Hospital. J Acquir Immune Defic Syndr Hum Retrovirol 1999; 20: 28–33
Perdue BE, Weidle PJ, Everson-Mays, et al. Evaluating the cost of medications for ambulatory HIV-infected persons associated with landmark changes in antiretroviral therapy. J Acquir Immune Defic Syndr Hum Retrovirol 1998; 4: 354–60
Lapins D, Hamel E, Barret J, et al. Cost of HIV care in the era of combination therapy [abstract PO 460–737]. 39th ICAAC; 1999 Sep 26–29; San Francisco
Moore RD. Cost-effectiveness of combination HIV therapy: 3 year later. Pharmacoeconomics 2000; 17 (4): 325–30
Grimes DA, Schultz KF. Bias and causal associations in obser-vational research. Lancet 2002; 359: 248–52
Tramarin A, Tolley K, Campostrini S, et al. Efficiency and rationality in the planning of health care for people with AIDS: an application of the balance of care approach. AIDS 1997; 11: 809–16
Aggiornamento dei casi di AIDS notificati in Italia al 30 Giugno 2000. Notiziario dell’Istituto Superiore di SanitA 2000; 13 (11): 1–12
Alonso J, Hunt S, Niero M, and the European Group for Quality of Life and Health Measurement. European guide to the Nottingham health profile. D Bucquet, editor. France: Montpellier, 1992
Wilking D, Thompson C. User’s guide to dependency measures for elderly people: social service monograph 1989. Sheffield: Joint Unit for Social Services Research, University of Sheffield, 1989
Postma MJ, Jager JC, Ruwaard D, et al. Disease-staging for modelling current and future health-care impact of disease; illustrations for diabetes mellitus and AIDS. Health Policy 1998; 43: 45–54
Turner BJ, Kelly JV, Ball JK. A severity classification system for AIDS hospitalisations. Med Care 1989; 27: 423–36
Kelly JV, Ball JK, Turner BJ. Duration and costs of AIDS hospitalisation in new york: variations by patients severity illness and hospital type. Med Care 1989; 27: 1085–98
Scitovsky AA. Studying the cost of HIV-related illnesses: reflection on the moving target. Milbank Q 1989; 673: 18–44
Miners AH, Sabin CA, Trueman P, et al. Assessing the costeffectiveness of HAART for adults with HIV in England. HIV Med 2001; 2 (1): 52–8
Cook J, Dasbach E, Coplan P, et al. Modelling the long term outcomes and costs of HIV antiretroviral therapy using HIV RNA levels: application to a clinical trial. AIDS Res Hum Retroviruses 1999; 15 (6): 499–508
Paul S, Gilbert HM, Ziecheck W, et al. The impact of potent antiretroviral therapy on the characteristics of hospitalized patients with HIV infection. AIDS 1999 Feb 25; 13 (3): 415–8
Garanttini L, Tediosis F, Di Cintio E, et al. Resource utilisation and hospital costs of HIV/AIDS care in Italy in the era of highly active antiretroviral therapy. AIDS Care 2001; 13 (6): 733–41
Johnson AM, Shergold C, Haekins A, et al. Patterns of hospital care for patients with HIV infection and AIDS. J Epidemiol Community Health 1993; 47: 232–7
Beck EJ, Kennelly J, McKevitt J, et al. Changing use of hospital services and costs at a London AIDS referral centre. AIDS 1994; 8: 367–77
Taroni F, Anemona A per it gruppo di Studio AN. CO. L’assistenza ospedaliera per i pazienti con AIDS in Italia. GIAIDS 1993; 1: 2–15
Torti C, Casari S, Palvarini L, et al. Modifications of health resource-use in Italy after the introduction of highly active antiretroviral therapy (HAART) for human immunodeficiency virus (HIV) infection. Pharmacoeconomic implications in a population-based setting. Health Policy 2003 Sep; 65 (3): 261–7
Nieuwkerk PT, Gisolf EH, Colebunders R, et al. Quality of life in asymptomatic HIV infected patients in a trial of ritonavir/saquinavir therapy. AIDS 2000; 14: 181–2
Revicky DA, Moyle G, Stellbrink HJ, et al. Quality of life outcomes of combination zalcitabine-zidovudine, saquinavir-zidovudine and saquinavir-zalcitabine-zidovudinetherapy for HIV-infected adults with CD4 cell count between 50 and 350 per cubic millimeter. AIDS 1999; 13: 851–8
Black N. Why we need observational studies to evaluate the effectiveness of health care. BMJ 1996; 312: 1215–8
Acknowledgements
The 1998 study (The Palladio study) has been partly supported by Merck Sharp & Dohme S. p. A., Italy. The authors have no conflicts of interest that are directly or indirectly relevant to the content of this manuscript.
The authors gratefully acknowledge the contributions of Dr Dongping Yin (MSD S.p.A.) for his assistance and JM Bos (GUIDE/GRIP) for the critical review of the paper.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
The members of the Palladio Study group are: Alessandria: Azzini M, Mantia E; Asti: Biglino A, Degioanni M; Aviano: Tirelli U, Schioppa O; Belluno: Caruso G, Mondardini V; Bologna: Chiodo F, Borderi M, Donzelli C; Bologna2: Gritti F, Coronado O; Bolzano: Mian P, Paternoster C; Brescia: Carosi G, Torti C; Como: Vigevani GM, Pusterla L; Cremona: Carnevale G; Ferrara: Ghinelli F, Carradori S; Forlě: Cancellieri C, Mastroianni A; Genova1: Piersantelli N, Lorusso C; Genova2: Bassetti D; Genova3: Pagano G, Camera M; Fondi (LT): Di Toro MT; Legnago (VR): Parrinello A, Rovere P; Mantova: Scalzini A, Alessi F; Mestre: Borri A, Panese S; Milano1: Milazzo F, Rizzardini G; Milano2: Cargnel A, Grisetti R; Modena: Esposito R, Pignattari E, Del Borgo C; Rovigo: Carretta M, Masiero G; Padova: Meneghetti F, Scanio F; Pavia: Filice G, Patruno S; Schio (VI): Marranconi F, Merighi M; Torino1: Soranzo ML, Macor A; Torino2: Di Perri G; Trieste: Mascioli M, Errera G; Treviso: Vaglia A, Zanatta A; Trento: Mian P, Paternoster C, Dorigoni N; Udine: Ciccone L, Panzolli L; Venezia: Raise E, Rosini G; Verona: Concia E, Dal Bravo P.
Rights and permissions
About this article
Cite this article
Tramarin, A., Campostrini, S., Postma, M.J. et al. A multicentre study of patient survival, disability, quality of life and cost of care. Pharmacoeconomic 22, 43–53 (2004). https://doi.org/10.2165/00019053-200422010-00004
Published:
Issue Date:
DOI: https://doi.org/10.2165/00019053-200422010-00004