Abstract
Objective: The purpose of this study was to compare, from the payor perspective, the clinical and economic outcomes of olanzapine to those of haloperidol for the treatment of schizophrenia.
Design and setting: Clinical, quality-of-life and resource utilisation data were prospectively collected for US-residing patients with schizophrenia who were participating in a multicentre, randomised, double-blind clinical trial comparing olanzapine and haloperidol. Direct medical costs were estimated by assigning standardised prices (1995 values) to the resource utilisation data.
Patients and participants: 817 patients with schizophrenia who had a baseline Brief Psychiatric Rating Scale score (BPRS) ≥18 (items scored 0 to 6) and/or were no longer tolerating current antipsychotic therapy.
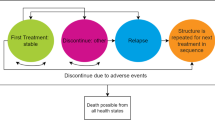
Interventions: Olanzapine 5 to 20 mg/day (n = 551) or haloperidol 5 to 20 mg/day (n = 266) for 6 weeks. Patients showing a predefined level of clinical response entered a 46-week maintenance phase.
Main outcome measures and results: After acute treatment, BPRS-based clinical improvements were seen in 38 and 27% of olanzapine and haloperidol patients, respectively (p = 0.002). Clinically important improvements on the Quality of Life Scale were achieved during acute treatment in 33% of olanzapine recipients and 25% of haloperidol recipients (p = 0.094). Olanzapine treatment in the acute phase led to significantly lower inpatient ($US5125 vs $US5795, p = 0.038) and outpatient ($US663 vs $US692, p = 0.001) costs, resulting in a significant overall reduction in mean total medical costs of $US388 (p = 0.033). This significant reduction in total costs was found despite olanzapine mean medication costs being significantly greater than haloperidol medication costs ($US326 vs $US15, p < 0.001). No significant differences in clinical improvement were observed in the maintenance phase. Maintenance phase olanzapine mean total medical costs were $US636 lower than haloperidol total costs (p = 0.128). Although olanzapine medication costs were significantly higher than haloperidol medication costs ($US3461 vs $US95, p < 0.001), this difference was offset by significantly lower inpatient ($US8322 vs $US10 662, p = 0.044) and outpatient ($US3810 vs $US5473, p = 0.038) costs.
Conclusions: In this study, olanzapine treatment was more effective than haloperidol in producing clinical response in the acute phase. In addition, olanzapine treatment led to reductions in inpatient and outpatient costs that more than offset olanzapine’s higher medication costs relative to haloperidol.
Similar content being viewed by others
References
Bland RC, Parker JH, Orn H. Prognosis in schizophrenia: a ten-year follow-up of first admissions. Arch Gen Psychiatry 1976; 33: 949–54
McGlashan TH. A selective review of recent North American long-term followup studies of schizophrenia. Schizophr Bull 1988; 14: 515–42
Tsuang MT. Suicide in schizophrenics, manics, depressives, and surgical controls: a comparison with general population suicide mortality. Arch Gen Psychiatry 1978; 35: 153–5
Tsuang MT, Woolson RF. Excess mortality in schizophrenia and affective disorders: do suicides and accidental death solely account for this excess? Arch Gen Psychiatry 1978; 35: 1181–5
Bromer EJ, Dew MA, Eaton W. Epidemiology of psychosis with special reference to schizophrenia. In: Tsuang MT, Tohen M, Zahner GEP, editors. Textbook in psychiatric epidemiology. New York (NY): John Wiley & Sons, 1996: 283–300
Keith SJ, Regier DA, Rae DS. Schizophrenic disorders. In: Robins LN, Regier DA, editors. Psychiatric disorders in America: the epidemiologic catchment area study. New York (NY): Free Press, 1991
Rice D, Miller L. The economic burden of schizophrenia. The 6th Biennial Research Conference on Economics in Mental Health; 1992 Sep 21-22; Bethesda (MD), 21–2
Rice D, Miller L. The economic burden of schizophrenia: conceptual and methodological issues, and cost estimates. In: Moscarelli M, Rupp A, Sartorius N, editors. Handbook of mental health economics and health policy. Vol. 1. New York (NY): John Wiley & Sons, 1996: 321–34
Rupp A, Keith SJ. The costs of schizophrenia: assessing the burden. Psychiatr Clin North Am 1993; 16: 413–23
Weiden PJ, Olfson M. Cost of relapse in schizophrenia. Schizophr Bull 1995; 21: 419–29
Dixon LB, Lehman AF, Levine J. Conventional antipsychotic medications for schizophrenia. Schizophr Bull 1995; 21: 567–78
Hegerty JD, Baldessarini RJ, Tohen M, et al. One hundred years of schizophrenia: a meta-analysis of the outcome literature. Am J Psychiatry 1994; 151: 1409–16
Casey DE. Motor and mental aspects of extrapyramidal syndromes. Int Clin Psychopharmacol 1995; 10 Suppl. 3: 105–14
Kane JM, Marder SR. Psychopharmacologic treatment of schizophrenia. Schizophr Bull 1993; 19: 287–302
Kane JM, McGlashan TH. Treatment of schizophrenia. Lancet 1995; 346: 820–5
Kane JM. Schizophrenia. N Engl J Med 1996; 334: 34–9
Keith SJ. Pharmacologic advances in the treatment of schizophrenia. N Engl J Med 1997; 337: 851–2
Lehman AF. Evaluating outcomes of treatments for persons with psychotic disorders. J Clin Psychiatry 1996; 57 Suppl. 11: 61–7
Borison RL. Recent advances in the pharmacotherapy of schizophrenia. Harv Rev Psychiatry 1997; 4: 255–71
Revicki DA. Methods of pharmacoeconomic evaluation of psychopharmacologic therapies for patients with schizophrenia. J Psychiatry Neurosci 1997; 22: 256–66
Revicki DA. Pharmacoeconomic evaluation of treatments for refractory schizophrenia: clozapine-related studies. J Clin Psychiatry 1999; 60 Suppl. 1: 7–11
Revicki DA, Luce BR, Weschler J, et al. Cost-effectiveness of clozapine for treatment-resistant schizophrenic patients. Hosp Community Psychiatry 1990; 41: 850–4
Meltzer H, Cola P, Way L, et al. Cost effectiveness of clozapine in neuroleptic-resistant schizophrenia. Am J Psychiatry 1993; 150: 1630–8
Frankenburg FR, Zanarini MC, Cole JO, et al. Hospitalization rates among clozapine-treated patients: a prospective cost-benefit analysis. Ann Clin Psychiatry 1992; 4: 247–50
Reid WH, Mason M, Toprac M. Savings in hospital bed-days related to treatment with clozapine. Hosp Community Psychiatry 1994; 45: 261–4
Jonsson D, Wålinder J. Cost-effectiveness of clozapine treatment in therapy-refractory schizophrenia. Acta Psychiatr Scand 1995; 92: 199–201
Addington DE, Jones B, Bloom D, et al. Reduction of hospital days in chronic schizophrenic patients treated with risperidone: a retrospective study. Clin Ther 1993; 15: 917–26
Guest JF, Hart WM, Cookson RF, et al. Pharmacoeconomic evaluation of long-term treatment with risperidone for patients with chronic schizophrenia. Br J Med Econ 1996; 10: 59–67
Frank RG. Clozapine’s cost-benefits [letter]. Hosp Community Psychiatry 1991; 42: 92
Meltzer HY, Cola PA. The pharmacoeconomics of clozapine: a review. J Clin Psychiatry 1994; 55 Suppl. B: 161–5
Hargreaves WA, Shumway M. Pharmacoeconomics of antipsychotic drug therapy. J Clin Psychiatry 1996; 57 Suppl. 9: 66–76
Essock SM, Hargreaves WA, Covell NH, et al. Clozapine’s effectiveness for patients in state hospitals: results from a randomized trial. Psychopharmacol Bull 1996; 32 (4): 683–97
Rosenheck R, Cramer J, Xu W, et al. A comparison of clozapine and haloperidol in hospitalized patients with refractory schizophrenia. N Engl J Med 1997; 337: 809–15
Mahmoud RA, Engelhart LM, Oster G, et al. Risperidone versus conventional antipsychotics: a prospective randomized naturalistic effectiveness trial of outcomes in chronic schizophrenia. 36th Annual Meeting of the American College of Neuropsychopharmacology; 1997 Dec 8-12; Kamuela (HA)
Beasley CM, Sanger T, Satterlee W, et al. Olanzapine versus placebo: results of a double-blind, fixed dose olanzapine trial. Psychopharmacology 1996; 124: 159–67
Beasley CM, Tollefson G, Tran P, et al. Olanzapine versus placebo and haloperidol: acute phase results of the North American double-blind olanzapine trial. Neuropsychopharmacology 1996; 14: 111–23
Beasley CM. Olanzapine versus placebo and haloperidol: acute phase results of the North American double-blind olanzapine trial. Response. Neuropsychopharmacology 1997; 16: 89–90
Tollefson GD, Beasley CM, Tran PV, et al. Olanzapine versus haloperidol in the treatment of schizophrenia, schizoaffective and schizophreniform disorders: results of an international collaborative trial. Am J Psychiatry 1997; 154: 457–65
Revicki DA, Genduso L, Hamilton S, et al. Olanzapine versus haloperidol in the treatment of schizophrenia and other related psychotic disorders: quality of life and clinical outcomes of a randomised clinical trial. Qual Life Res. In press
Tollefson G. Long-term continuation therapy with olanzapine: New Clinical Drug Evaluation Unit (NCDEU) Program. NCDEU Meeting; 1997 May 27-30; Boca Raton (FL)
Dellva MA, Tran P, Tollefson GD, et al. Standard olanzapine versus placebo and ineffective-dose olanzapine in the maintenance treatment of schizophrenia. Psychiatr Serv 1997; 46: 1571–7
Diagnostic and statistical manual of mental disorders. 3rd ed. Washington, DC: American Psychiatric Association, 1987
Woerner MG, Mannuza S, Kane JM. Anchoring the BPRS: an aid to improved reliability. Psychopharmacol Bull 1988; 24: 112–7
Guy W, editor. ECDEU Assessment manual for psychopharmacology. Rockville (MD): US Department of Health, Education, and Welfare (DHEW), 1976. DHEW publication no. (ADM): 76–338
Kay SR, Opler LA, Fiszbein A. Positive and negative syndrome scale (PANSS) manual. North Tonawanda (NY): Multi- Health Systems, Inc., 1986
Heinrichs DW, Hanlon TE, Carpenter WT. The quality of life scale: an instrument for rating the schizophrenic deficit syndrome. Schizophr Bull 1984; 10: 388–98
International Classification of Diseases, 9th revision, Clinical Modification. 4th ed. Los Angeles (CA): Practice Management Information Corporation (PMIC), 1993
Finkler S. The distinction between costs and charges. Ann Intern Med 1982; 96: 102–9
Luce BR, Elixhauser A. Estimating costs in the economic evaluation of medical technologies. Int J Technol Assess Health Care 1990; 6: 57–75
Gold MR, Siegel JE, Russell LB, et al., editors. Cost-effectiveness in health and medicine. New York (NY): Oxford University Press, 1996
Payment for part B medical and other health services. Fed Regist 1994; 59: 235
Reed SK, Hennessy KD, Mitchell OS, et al. A mental health capitation program. II: cost-benefit analysis. Hosp Community Psychiatry 1994; 45: 1097–103
Dwyer DS, Mitchell OS, Cole R, et al. Evaluating mental health capitation treatment: lessons from panel data. Cambridge (MA): National Bureau of Economic Research, 1995
US Bureau of Labor Statistics. CPI detailed report. Washington, DC: US Bureau of Labor Statistics, Department of Labor, 1995
Palmer CS, Revicki DA, Halpern MT, et al. The cost of suicide and suicide attempts in the United States. Clin Neuropharmacol 1995; 18 Suppl. 3: S25–33
National Association of Psychiatric Health Systems. Trends in psychiatric health systems: 1995 annual survey, final report. Washington, DC: National Association of Psychiatric Health Systems, 1995
Physicians GenRx. 5th ed. St. Louis (MO): Mosby-Year Book, 1995
Red Book pharmacy’s fundamental reference. Montville (NJ): Medical Economics Data Production Company, 1995
Glazer W, Ershefsky L. A pharmacoeconomic model of outpatient neuroleptic therapy in ‘revolving door’ schizophrenic patients. J Clin Psychiatry 1996; 57 (8): 337–45
Rutten-Van Molken MPMH, Van Doorslaer EKA, Van Vliet RCJA. Statistical analysis of cost outcomes in a randomized controlled clinical trial. Health Econ 1994; 3: 333–45
Anderson KH, Mitchell JM. Expenditures on services for persons with acquired immunodeficiency syndrome under a Medicaid home and community-based waiver program: are selection effects important? Med Care 1997; 35 (5): 425–39
Manning WG, Newhouse JP, Duan N, et al. Health insurance and the demand for medical care. Am Econ Rev 1987; 77: 251–77
SAS Institute, Inc. SAS/STAT user’s guide. Vols. 1 & 2. 4th ed. Version 6. Cary (NC): SAS Institute, Inc., 1990
Drummond MF, Stoddart GL. Economic analysis and clinical trials. Control Clin Trials 1984; 5: 115–28
Obenchain RL, Johnstone BM. Mixed-model imputation of cost data for early discontinuers from a randomized clinical trial. Drug Inf J 1999; 33: 191–209
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hamilton, S.H., Revicki, D.A., Edgell, E.T. et al. Clinical and Economic Outcomes of Olanzapine Compared With Haloperidol for Schizophrenia. Pharmacoeconomics 15, 469–480 (1999). https://doi.org/10.2165/00019053-199915050-00005
Published:
Issue Date:
DOI: https://doi.org/10.2165/00019053-199915050-00005