Summary
Abstract
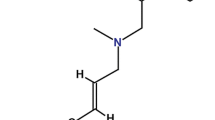
Sertaconazole (Dermofix®, Ertaczo™, Ginedermofix®, Monazol, Mykosert® or Zalain®), an imidazole antifungal agent, inhibits the synthesis of ergosterol, an essential cell wall component of fungi. It is indicated in the EU for the treatment of superficial skin mycoses such as dermatophytosis (including tinea corporis, tinea cruris, tinea manus, tinea barbae and tinea pedis), cutaneous candidiasis, pityriasis versicolor and seborrhoeic dermatitis of the scalp, and in the US for tinea pedis only.
Sertaconazole has broad-spectrum antifungal activity against dermatophytes of the Trichophyton, Epidermophyton and Microsporum genera, and yeasts of the genera Candida and Cryptococcus; additionally, it is effective against opportunistic filamentous fungi and Gram-positive bacteria. Moreover, the antifungal activity of sertaconazole is maintained in clinical isolates of dermatophytes that show reduced susceptibility to other azoles. While the drug has good dermal penetration, this is not associated with systemic absorption. In clinical trials in patients with superficial mycoses, 2% sertaconazole cream applied twice daily was effective in the eradication of a range of dermatophytoses, and a significantly greater proportion of patients were cured compared with those receiving 2% miconazole cream twice-daily treatment. In patients with vulvovaginal candidiasis, sertaconazole as a single-dose ovule or tablet was effective in the eradication of Candida spp., and achieved both a more rapid and a higher cure rate compared with a triple dose of econazole. Both as a topical cream and suppository preparation, sertaconazole was generally well tolerated. Sertaconazole is a well established antifungal agent, which is now available in a variety of formulations, and remains a useful treatment option particularly in patients with fungal infections resistant to other azoles.
Pharmacological Properties
Like other azoles, sertaconazole inhibits the synthesis of ergosterol, an essential component of fungal cell walls, resulting in disruption of mycelial growth and replication. However, at higher concentrations, sertaconazole binds directly to nonsterol lipids in the fungal cell wall, which leads to increased permeability and subsequent lysis of the mycelium. Thus, depending on the concentration, sertaconazole may exhibit both fungistatic and fungicidal activities.
Sertaconazole shows good in vitro fungistatic activity against a broad range of dermatophytes of the Trichophyton, Epidermophyton and Microsporum genera, and yeasts of the genera Candida and Cryptococcus. The geometric minimum inhibitory concentration (MIC) of sertaconazole ranged from 0.06 to 1 mg/mL against a variety of dermatophyte isolates (n = 456), which included 114 isolates with reduced susceptibility to fluconazole (MICs ≥16μg/mL). Similarly, against a variety of Candida spp., MIC values at which 90% of cultures were inhibited (MIC90) for sertaconazole were ≤0.1–4μg/mL compared with MIC90 of 0.1 to >100 μg/mL for fluconazole. Furthermore, fungicidal activity of sertaconazole was apparent against a variety of Candida spp., with minimum fungicidal concentration values of 0.5–64 μg/mL.
Additionally, sertaconazole showed antibacterial activity with a geometric MIC of 0.88μg/mL against 21 isolates of Gram-positive bacteria. When applied topically in experimental models of inflammation, sertaconazole showed some evidence of anti-inflammatory action. Only 4% of 250 clinical isolates of dermatophytes and Scopulariopsis brevicaulis from Spanish hospitals showed resistance to sertaconazole, and continuous culture of Candida spp. in sertaconazole-containing media failed to induce resistance. Following application of sertaconazole as a topical cream or vaginal suppository, plasma levels of the drug remained undetectable in healthy volunteers.
Therapeutic Efficacy
In randomized, double-blind, multicentre trials of 3–6 weeks’ duration (n= 127–383), a significantly greater number of patients with tinea of the glabrous skin and tinea pedis receiving topical 2% sertaconazole cream once or twice daily achieved a successful mycological cure compared with recipients of a placebo cream. Moreover, the clinical cure rate and the mycological cure rate of 2% sertaconazole cream twice daily was significantly higher than that of 2% miconazole cream twice daily in patients with a range of cutaneous mycoses (n = 631) in a randomized, double-blind, multicentre, phase III, comparator trial of 35 days’ duration. Furthermore, a greater proportion of patients receiving sertaconazole achieved the category of clinically cured at a significantly earlier timepoint than recipients of miconazole. An open-label, noninferiority trial of 28 days’ duration in 313 patients with tinea corporis, tinea pedis or a corresponding candidiasis showed that sertaconazole as a 2% solution was as effective as treatment with a 2% cream preparation.
Sertaconazole as a single-dose 300 mg vaginal ovule or 500 mg tablet was successful in the eradication of Candida spp. in 65–100% of patients with vaginal candidiasis in trials that evaluated clinical and mycological cure rates up to 1 year after the last treatment application (n = 37–327). Furthermore, the clinical cure rate and the mycological cure rate of single-dose sertaconazole 500 mg tablet was significantly greater than that of triple-dose econazole 150 mg in the eradication of Candida albicans and also achieved a more rapid response rate in patients with vaginal candidiasis (n=37).
Tolerability
Sertaconazole was generally well tolerated in patients with dermatological and gynaecological mycoses. Adverse events associated with topical application of sertaconazole cream were mostly cutaneous-related and included contact dermatitis, dry or burning skin, application-site reaction, eczema, itch and skin tenderness. However, the frequency of adverse events did not differ from that of the placebo vehicle treatment arm. Furthermore, sertaconazole showed no evidence of a sensitizing action in causing contact dermatitis in healthy volunteers. Sertaconazole administered as a vaginal suppository was generally associated with an absence of adverse events and, where reported, included only local irritation after insertion.





Similar content being viewed by others
References
Pfaller MA, Sutton DA. Review of in vitro activity of sertaconazole nitrate in the treatment of superficial fungal infections. Diagn Microbiol Infect Dis 2006 Oct; 56(2): 147–52
Pappas P, Rex J, Sobel J, et al. Guidelines for the treatment of candidiasis. Clin Infect Dis 2004; 38(2): 161–89
Vander Straten M, Hossain M, Ghannoum M. Cutaneous infections: dermatophytosis, onychomycosis, and tinea versicolor. Infect Dis Clin North Am 2003; 17(1): 87–112
Faergemann J. Management of seborrheic dermatitis and pityriasis versicolor. Am J Clin Dermatol 2000; 1(2): 75–80
Garber G. An overview of fungal infections. Drugs 2001; 61 (Suppl. 1): 1–12
Henzl M. Properties of sustained-release single-dose formulations for vulvovaginal candidiasis. Am J Drug Deliv 2005; 3(4): 227–37
Sobel JD. Vulvovaginal candidosis. Lancet 2007; 369(9577): 1961–71
Loo D. Cutaneous fungal infections in the elderly. Dermatol Clin 2004; 22(1): 33–50
Rios-Fabra A, Moreno A, Isturiz R. Fungal infection in Latin American countries. Infect Dis Clin North Am 1994; 8(1): 129–54
Chong AH, Sinclair RD. Diagnosing superficial mycoses. Am J Clin Dermatol 2000; 1(2): 125–31
Martin G, Mannino D, Eaton S, et al. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med 2003; 348(16): 1546–54
Sobel J. Practice guidelines for the treatment of fungal infections [letter]. Clin Infect Dis 2000; 30(4): 652
Kauffmann C. Fungal infections. Proc Am Thorac Soc 2006; 3(1): 35–40
Boucher H, Groll A, Chiou C, et al. Newer systemic antifungal agents: pharmacokinetics, safety and efficacy. Drugs 2004; 64(18): 1997–2020
Singh N. Trends in the epidemiology of opportunistic fungal infections: predisposing factors and the impact of antimicrobial use practices. Clin Infect Dis 2001; 33: 1692–6
Ferrer International SA. Dermofix® Crema 2%. [online]. Available from URL: http://www.vademecum.es/medicamento/dermofix-1-0-1,1,1,1,1-1-0-4-0-1061-1/dermofix.html [Accessed 2008 Nov 12]
Bertek Pharmaceuticals Inc. Ertaczo™ (sertaconazole nitrate) cream, 2% [online]. Available from URL: http://www.fda.gov/cder/foi/label/2003/21385_Ertaczo_lbl.pdf [Accessed 2008 Nov 12]
Ferrer International SA. Dermofix® 2% solution [online]. Available from URL: http://www.vademecum.es/medicamento/sertaconazol-2-2-1,1,1,1,1-3-0-2-1643-1064-1dermofixhtml [Accessed 2009 Feb 16]
Ferrer International SA. Dermofix® 2% gel [online]. Available from URL: http://www.vademecum.es/medicamento/sertaconazol-2-2-1,1,1,1,1-3-0-2-1643-1062-1/dermofix.html [Accessed 2009 Feb 16]
Ferrer International SA. Ginedermofix® [online]. Available from URL: http://www.vademecum.es/medicamento/farmacologia/G/21203/1/ginedermofix.html [Accessed 2009 Feb 10]
EGIS Pharmaceuticals Ltd. Zalain® special product characteristics [online]. Available from URL: http://www.zdravie.sk/lieciva/doc/SPC20664.pdf [Accessed 2009 Feb 10]
Vidal. Monazol Antifongique [online]. Available from URL: http://www.automedication.fr/medicament/medicamentgf440011-MONAZOL.html [Accessed 2009 Feb 16]
Pfleger. Mykosert®, creme [online]. Available from URL: http://www.dr-pfleger.de [Accessed 2009 Feb 10]
Pfleger. Mykosert®, lösung [online]. Available from URL: http://www.dr-pfleger.de [Accessed 2009 Feb 10]
Palacin C, Sacristan A, Ortiz JA. In vitro activity of sertaconazole. Arzneimittelforschung 1992 May; 42(5A): 699–705
Drouhet E, Dupont B. In vitro antifungal activity of sertaconazole. Arzneimittelforschung 1992 May; 42(5A): 705–10
Carillo-Munoz AJ, Tur-Tur C. Comparative study of antifungal activity of sertaconazole, terbinafine, and bifonazole against clinical isolates of Candida spp., Cryptococcus neoformans and dermatophytes. Chemotherapy 1997; 43(6): 387–92
Carrillo-Munoz AJ, Fernandez-Torres B, Guarro J. In vitro antifungal activity of sertaconazole against 309 dermatophyte clinical isolates. J Chemother 2003 Dec; 15(6): 555–7
Carrillo-Munoz AJ, Quindos G, Del Valle O, et al. In vitro antifungal activity of sertaconazole nitrate against recent isolates of onychomycosis causative agents [letter]. J Chemother 2008 Aug; 20(4): 521–3
Carrillo-Munoz AJ, Fernandez-Torres B, Cardenes DC, et al. In vitro activity of sertaconazole against dermatophyte isolates with reduced fluconazole susceptibility. Chemotherapy 2003 Sep; 49(5): 248–51
Carrillo-Munoz AJ, Guglietta A, Palacin C, et al. In vitro antifungal activity of sertaconazole compared with nine other drugs against 250 clinical isolates of dermatophytes and Scopulariopsis brevicaulis. Chemotherapy 2004 Dec; 50(6): 308–13
Carrillo-Munoz AJ, Brio S, Quindos G, et al. Sertaconazole: in-vitro antifungal activity against vaginal and other superficial yeast isolates. J Chemother 2001 Oct; 13(5): 555–62
Palacin C, Sacristan A, Ortiz JA. In vitro comparative study of the fungistatic and fungicidal activity of sertaconazole and other antifungals against Candida albicans. Arzneimittelforschung 1992 May; 42(5A): 711–4
Palacin C, Tarrago C, Agut J, et al. In vitro activity of sertaconazole, fluconazole, ketoconazole, fenticonazole, clotrimazole and itraconazole against pathogenic vaginal yeast isolates. Methods Find Exp Clin Pharmacol 2001 Mar; 23(2): 61–4
Martin-Mazuelos E, Aller AI, Morilla D, et al. Antifungal activity of sertaconazole in vitro against clinical isolates of Candida spp. Chemotherapy 1996 Mar-1996 30; 42(2): 112–7
Carrillo-Munoz AJ, Tur-Tur C, Bornay-Llinares FJ, et al. Comparative study of the in vitro antifungal activity of bifonazole, naftifine and sertaconazole against yeasts. J Chemother 1999 Jun; 11(3): 187–90
Agut J, Tarrida N, Sacristan A, et al. Antiinflammatory activity of topically applied sertaconazole nitrate. Meth Find Exp Clin Pharmacol 1996 May; 18(4): 233–4
Liebel F, Lyte P, Garay M, et al. Anti-inflammatory and anti-itch activity of sertaconazole nitrate. Arch Dermatol Res 2006 Sep; 298(4): 191–9
Clinical and Laboratory Standards Institute. Reference method for broth dilution antifungal susceptibility testing of filamentous fungi; appoved standard-second edition [online]. Available from URL: http://www.clsi.org/source/orders/free/M38-a2.pdf [Accessed 2008 Nov 11]
Clinical and Laboratory Standards Institute. Reference method for broth dilution antifungal suseptibility testing of yeasts; approved standard-third edition [online]. Available from URL: http://www.clsi.org/source/orders/free/M27-A3.pdf [Accessed 2008 Nov 11]
Ghannoum M, Arthington-Skaggs B, Chaturvedi V, et al. Interlaboratory study of quality control isolates for a broth microdilution method (modified CLSI M38-A) for testing susceptibilities of dermatophytes to antifungals. J Clin Microbiol 2006; 44(12): 4353–6
Agut J, Palacin C, Salgado J, et al. Direct membrane-damaging effect of sertaconazole on Candida albicans as a mechanism of its fungicidal activity. Arzneimittelforschung 1992 May; 42(5A): 721–4
Agut J, Palacin C, Sacristan A, et al. Inhibition of ergosterol synthesis by sertaconazole in Candida albicans. Arzneimittelforschung 1992 May; 42(5A): 718–20
Del Rosso JQ. Comprehensive management of patients with superficial fungal infections: the role of sertaconazole nitrate. Cutis 2008 Jun; 81 (Suppl. 6): 4–18
Cournia Z, Ullmann G, Smith J. Differential effects of cholesterol, ergosterol and lanosterol on a dipalmitoyl phosphatidylcholine membrane: a molecular dynamics study. J Phys Chem B 2007; 111(7): 1786–801
Sanchez JA. Sertaconazole, mechanism of action and pharmacokinetics. J Eur Acad Dermatol Venereol 1993; 2 (Suppl. 2): S71–6
Zhang A, Camp W, Elewski B. Advances in topical and systemic antifungals. Dermatol Clin 2007; 25(2): 165–83
Carrillo-Munoz A, Giusiano G, Ezkurra P, et al. Sertaconazole: updated review of a topical antifungal agent. Expert Rev Anti Infect Ther 2005; 3(3): 333–42
Guarro J, Figueras MJ, Cano J. Alterations produced by sertaconazole on the morphology and ultrastructure of Candida albicans. Mycoses 1989 Jun; 32(6): 283–95
Susilo R, Korting HC, Strauss UP, et al. Rate and extent of percutaneous absorption of sertaconazole nitrate after topical administration. Arzneimittelforschung 2005; 55(6): 338–42
Palacin C, Tarrago C, Sacristan A, et al. Antifungal activity of sertaconazole in the cutaneous retention time test. J Mycol Med 1995; 5(1): 35–9
Lupetti A, Danesi R, Campa M, et al. Molecular basis of resistance to azole antifungals. Trends Mol Med 2002; 8(2): 76–81
Azcona O, Torrent J, Verges J, et al. Tolerance and kinetic behavior after single and repeated vaginal administration of sertaconazole cream and tablets in healthy volunteers. Curr Ther Res 1991; 49(6): 1046–60
Farre M, Ugena B, Badenas JM, et al. Pharmacokinetics and tolerance of sertaconazole in man after repeated percutaneous administration. Arzneimittelforschung 1992 May; 42(5A): 752–4
Guerin V, Delance V, Papalexiou P, et al. Systemic absorption of C-14-radiolabelled sertaconazole administered in 300 mg prolonged-liberation vaginal suppository form to four healthy post-menopausal women. J Mycol Med 1996 Jun; 6: 63–7
De Lunardo M, Muzard G, Guerin V, et al. Caractéristiques pharmacocinétiques d’un nouvel antifonique imidazolé: le nitrate de sertaconazole. J Mycol Med 1999; 9: 137–42
Susilo R, Korting HC, Greb W, et al. Nail penetration of sertaconazole with a sertaconazole-containing nail patch formulation. Am J Clin Dermatol 2006; 7(4): 259–62
Agut J, Moren M, Rego M, et al. Pharmacokinetic evaluation of labelled sertaconazole after dermal application. Arzneimittelforschung 1992 May; 42(5A): 748–51
Savin R, Jorizzo J. The safety and efficacy of sertaconazole nitrate cream 2% for tinea pedis. Cutis 2006 Oct; 78(4): 268–74
Susilo R, Korting HC, Strauss UP, et al. Dermatomycoses of the glabrous skin: a double-blind, randomised, comparative trial of sertaconazole 2% cream once daily versus vehicle. Clin Drug Investig 2003; 23(6): 387–94
Alomar C, Bassas S, Casas M, et al. Multi-centre double-blind trial on the efficacy and safety of sertaconazole 2% cream in comparison with miconazole 2% cream on patients suffering from cutaneous mycoses. Arzneimittelforschung 1992 May; 42(5A): 767–73
Pedragosa R, Gonzalez B, Martin M, et al. Therapeutic efficacy and safety of the new antimycotic sertaconazole in the treatment of cutaneous dermatophytosis. Arzneimittelforschung 1992 May; 42(5A): 760–3
Borelli C, Klovekorn G, Ernst TM, et al. Comparative study of 2% sertaconazole solution and cream formulations in patients with tinea corporis, tinea pedis interdigitalis, or a corresponding candidosis. Am J Clin Dermatol 2007; 8(6): 371–8
Nasarre J, Umbert P, Herrero E, et al. Therapeutic efficacy and safety of the new antimycotic sertaconazole in the treatment of Pityriasis versicolor. Arzneimittelforschung 1992 May; 42(5A): 764–7
Van Esso D, Fajo G, Losada I, et al. Sertaconazole in the treatment of pediatric patients with cutaneous dermatophyte infections. Clin Ther 1995 Mar 30; 17(2): 264–9
Crespo V, Marquez M, Torres J, et al. Ensayo clínco en fase III de sertaconazol en solución frente a placebo en el tratamiento de la pitiriasis versicolor. Piel 1993; 8: 165–9
Quereux C, Gelas B, Chevallier T, et al. Assessment of efficacy and speed of action of a treatment combining sertaconazole nitrate vaginal suppository and cream in vulvovaginal candidiasis. Gynecol Obstet Fert 2000; 28(3): 238–44
Dellenbach P, Thomas JL, Guerin V, et al. Topical treatment of vaginal candidosis with sertaconazole and econazole sustained-release suppositories. Int J Gynaecol Obstet 2000 Dec; 71 Suppl. 1: S47–52
Lopez-Olmos J, Lerma E, Parra I. Comparison of single dose fenticonazole versus sertaconazole as the treatment of vulvovaginal candidiasis: a prospective, multicentre study over one year [in Spanish]. Clinica e Investigacion En Ginecologia y Obstetricia 2003; 30(1): 10–7
Wang PH, Chao HT, Chen CL, et al. Single-dose sertaconazole vaginal tablet treatment of vulvovaginal candidiasis. J Chin Med Assoc 2006 Jun; 69(6): 259–63
Romaguera C, Herrero E, Marquez M, et al. Study on the sensitizing capacity of the new antimycotic sertaconazole in the treatment of cutaneous mycoses. Arzneimittelforschung 1992 May; 42(5A): 754–6
Drake L, Dinehart S, Farmer E, et al. Guidelines of care for superficial mycotic infections of the skin: tinea corporis, tinea cruris, tinea faciei, tinea manuum and tinea pedis. J Am Acad Dermatol 1996; 34 (2 Pt. 1): 282–6
Higgins E, Fuller L, Smith C. Guidelines for the management of tinea capitis. Br J Dermatol 2000; 143(1): 53–8
Roberts D, Taylor W, Boyle J. Guidelines for the treatment of onychomycosis. Br J Dermatol 2003; 148(3): 402–10
Erbagci Z. Topical therapy for dermatophytosis: should corticosteroids be included? Am J Clin Dermatol 2004; 5(6): 375–84
British Association of Dermatologists. Pityriasis versicolor [online]. Available from URL: http://www.bad.org.uk/public/leaflets/Pityriasis_versicolor_Ed_DM_17.4.2008.pdf [Accessed 2008 Dec 4]
Kyle AA, Dahl MV. Topical therapy for fungal infections. Am J Clin Dermatol 2004; 5(6): 443–51
Author information
Authors and Affiliations
Corresponding author
Additional information
Various sections of the manuscript reviewed by: M. Bassetti, Infectious Diseases Division, San Martino University and University of Genoa, Genoa, Italy; A.J. Carrillo-Munoz, Department of Microbiology, Asesoria Cientifica y de la Investigacion Aplicada Hospital Vall d’Hebron, Barcelona, Spain; J. das Neves, Department of Pharmaceutical Technology, Faculty of Pharmacy, University of Porto, Porto, Portugal; H.C. Korting, Klinik und Poliklinik für Dermatologie und Allergologie, Klinikum der Universität München, Munich, Germany; M.A. Pfaller, Department of Pathology, College of Medicine, University of Iowa, Iowa City, Iowa, USA; S. Veraldi, Institute of Dermatological Sciences, University of Milan, I.R.C.C.S. Foundation, Ospedale Maggiore Policlinico, Mangiagalli and Regina Elena, Milan, Italy.
Data Selection
Sources: Medical literature published in any language since 1980 on ‘sertaconazole’, identified using MEDLINE and EMBASE, supplemented by AdisBase (a proprietary database of Wolters Kluwer Health | Adis). Additional references were identified from the reference lists of published articles. Bibliographical information, including contributory unpublished data, was also requested from the company developing the drug.
Search strategy: MEDLINE, EMBASE and AdisBase search terms were ‘sertaconazole’ and ‘mycoses’. Searches were last updated 16 February 2009.
Selection: Studies in patients with superficial mycoses who received sertaconazole. Inclusion of studies was based mainly on the methods section of the trials. When available, large, well controlled trials with appropriate statistical methodology were preferred. Relevant pharmacodynamic and pharmacokinetic data are also included.
Index terms: Sertaconazole, mycoses, dermatology, gynaecology, pharmacodynamics, pharmacokinetics, therapeutic use, tolerability.
Rights and permissions
About this article
Cite this article
Croxtall, J.D., Plosker, G.L. Sertaconazole. Drugs 69, 339–359 (2009). https://doi.org/10.2165/00003495-200969030-00009
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-200969030-00009