Abstract
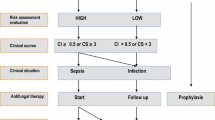
When and how to treat invasive fungal infections (IFIs) is discussed in this review, with a focus on the two most prevalent non-endemic IFIs, namely invasive aspergillosis and invasive candidiasis. Early treatment initiation in patients with IFIs has a profound impact on mortality rates, but reliable diagnostic measures are lacking. This situation has led to the parallel use of different treatment strategies, e.g. prophylaxis, empirical and pre-emptive treatment, as well as targeted treatment in response to a definite diagnosis of IFI. Identifying high-risk patients is the first step in reducing IFI-related mortality. Patients at risk of invasive aspergillosis comprise (i) those with acute myelogenous leukaemia (AML) or myelodysplastic syndrome (MDS) during remission induction chemotherapy; (ii) patients undergoing allogeneic haematopoietic stem cell transplantation (HSCT); (iii) recipients of solid organ transplants; and (iv) those with other conditions of severe and prolonged immunosuppression. Patients at high risk of invasive candidiasis are less well defined. Risk factors are diverse and include haematological malignancy, neutropenia, age <1 month or >65 years, and recent abdominal surgery. The individual risk further depends on the presence of a variety of other risk factors, including central venous catheters, use of broad spectrum antibacterials, prolonged intensive care unit (ICU) stay, total parenteral nutrition, mucosal Candida spp. colonization and renal failure.
Extensive research has been conducted to facilitate the best possible treatment strategies for these severe infections. Optimal timing and choice of antifungal agents largely remain a matter of controversy. After having reviewed the major clinical trials, we conclude that comparisons between different treatment strategies cannot be made, neither at present nor in the near future. The complexity of the clinical problem leads to an eclectic treatment approach to reduce morbidity and mortality from IFIs without compromising tolerability. We recommend prophylaxis with posaconazole for allogeneic HSCT recipients, patients receiving induction chemotherapy for AML or MDS, and those undergoing immunosuppressive therapy for graft-versus-host disease after allogeneic HSCT. For the empirical treatment of persistently febrile neutropenia, caspofungin is our first-and liposomal amphotericin B deoxycholate (LAmB) our second-line choice. Once a diagnosis of invasive aspergillosis has been established, voriconazole should be the preferred treatment option, with LAmB being an alternative. Fluconazole prophylaxis for invasive candidiasis should remain restricted to high-risk ICU patients. Once a diagnosis has been established, the drug of choice for adequate treatment depends largely on neutrophil count and haemodynamic stability. In non-neutropenic patients, an echinocandin should be considered the first-line treatment option, while patients with susceptible Candida spp. may be switched to fluconazole. In neutropenic patients, caspofungin or micafungin might be preferred to anidulafungin as first-line treatment. LAmB is a second-line treatment option in both settings.
Early diagnosis of IFIs is imperative to facilitate treatment success. In all patients at risk for IFIs, blood cultures, galactomannan antigen and diagnostic imaging should be rigorously enforced.






Similar content being viewed by others
References
Maschmeyer G, Haas A, Cornely OA. Invasive aspergillosis: epidemiology, diagnosis and management in immunocompromised patients. Drags 2007; 67(11): 1567–601
Pfaller MA, Diekema DJ. Epidemiology of invasive candidiasis: a persistent public health problem. Clin Microbiol Rev 2007 Jan; 20(1): 133–63
Morris A, Lundgren JD, Masur H, et al. Current epidemiology of Pneumocystis pneumonia: emerging infectious diseases 2004 Oct; 10(10): 1713–20
Marr KA, Carter RA, Crippa F, et al. Epidemiology and outcome of mould infections in hematopoietic stem cell transplant recipients. Clin Infect Dis 2002 Apr 1; 34(7): 909–17
Husain S, Alexander BD, Munoz P, et al. Opportunistic mycelial fungal infections in organ transplant recipients: emerging importance of non-Aspergillus mycelial fungi. Clin Infect Dis 2003 Jul 15; 37(2): 221–9
Walsh TJ, Finberg RW, Arndt C, et al. Liposomal amphotericin B for empirical therapy in patients with persistent fever and neutropenia. National Institute of Allergy and Infectious Diseases Mycoses Study Group. N Engl J Med 1999 Mar 11; 340(10): 764–71
Walsh TJ, Pappas P, Winston DJ, et al. Voriconazole compared with liposomal amphotericin B for empirical antifungal therapy in patients with neutropenia and persistent fever. N Engl J Med 2002 Jan 24; 346(4): 225–34
Walsh TJ, Teppler H, Donowitz GR, et al. Caspofungin versus liposomal amphotericin B for empirical antifungal therapy in patients with persistent fever and neutropenia. N Engl J Med 2004 Sep 30; 351(14): 1391–402
Herbrecht R, Denning DW, Patterson TF, et al. Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. N Engl J Med 2002 Aug 8; 347(6): 408–15
Mora-Duarte J, Betts R, Rotstein C, et al. Comparison of caspofungin and amphotericin B for invasive candidiasis. N Engl J Med 2002 Dec 19; 347(25): 2020–9
Ascioglu S, Rex JH, de Pauw B, et al. Defining opportunistic invasive fungal infections in immunocompromised patients with cancer and hematopoietic stem cell transplants: an international consensus. Clin Infect Dis 2002 Jan 1; 34(1): 7–14
Cornely OA, Ullmann AJ, Karthaus M. Evidence-based assessment of primary antifungal prophylaxis in patients with hematologic malignancies. Blood 2003 May 1; 101(9): 3365–72
Ullmann AJ, Cornely OA. Antifungal prophylaxis for invasive mycoses in high risk patients. Curr Opin Infect Dis 2006 Dec; 19(6): 571–6
Pagano L, Caira M, Candoni A, et al. The epidemiology of fungal infections in patients with hematologic malignancies: the SEIFEM-2004 study. Haematologica 2006 Aug; 91(8): 1068–75
Denning DW. Invasive aspergillosis. Clin Infect Dis 1998 Apr; 26(4): 781–803; quiz 4-5
Marr KA, Carter RA, Boeckh M, et al. Invasive aspergillosis in allogeneic stem cell transplant recipients: changes in epidemiology and risk factors. Blood 2002 Dec 15; 100(13): 4358–66
Patterson TF, Kirkpatrick WR, White M, et al. Invasive aspergillosis: disease spectrum, treatment practices, and outcomes. 13 Aspergillus Study Group. Medicine (Baltimore) 2000 Jul; 79(4): 250–60
Martino R, Parody R, Fukuda T, et al. Impact of the intensity of the pretransplantation conditioning regimen in patients with prior invasive aspergillosis undergoing allogeneic hematopoietic stem cell transplantation: a retrospective survey of the Infectious Diseases Working Party of the European Group for Blood and Marrow Transplantation. Blood 2006 Nov 1; 108(9): 2928–36
Cornet M, Fleury L, Maslo C, et al. Epidemiology of invasive aspergillosis in France: a six-year multicentric survey in the Greater Paris area. J Hosp Infect 2002 Aug; 51(4): 288–96
Cornely OA, Maertens J, Bresnik M, et al. Liposomal amphotericin B as initial therapy for invasive mold infection: a randomized trial comparing a high-loading dose regimen with standard dosing (AmBiLoad trial). Clin Infect Dis 2007 May 15; 44(10): 1289–97
Cordonnier C, Ribaud P, Herbrecht R, et al. Prognostic factors for death due to invasive aspergillosis after hematopoietic stem cell transplantation: a 1-year retrospective study of consecutive patients at French transplantation centers. Clin Infect Dis 2006 Apr 1; 42(7): 955–63
Martino R, Subira M, Rovira M, et al. Invasive fungal infections after allogeneic peripheral blood stem cell transplantation: incidence and risk factors in 395 patients. Br J Haematol 2002 Feb; 116(2): 475–82
Paya CV. Fungal infections in solid-organ transplantation. Clin Infect Dis 1993 May; 16(5): 677–88
Winston DJ, Emmanouilides C, Busuttil RW. Infections in liver transplant recipients. Clin Infect Dis 1995 Nov; 21(5): 1077–89; quiz 90-1
Infectious disease community of practice, fungal infections. Am J Transplant 2004; 4 Suppl. 10: 110–34
Fishman JA. Infection in solid-organ transplant recipients. N Engl J Med 2007 Dec 20; 357(25): 2601–14
Singh N. Antifungal prophylaxis for solid organ transplant recipients: seeking clarity amidst controversy. Clin Infect Dis 2000 Aug; 31(2): 545–53
Singh N, Husain S. Aspergillus infections after lung transplantation: clinical differences in type of transplant and implications for management. J Heart Lung Transpl 2003 Mar; 22(3): 258–66
Fortun J, Martin-Davila P, Moreno S, et al. Risk factors for invasive aspergillosis in liver transplant recipients. Liver Transpl 2002 Nov; 8(11): 1065–70
Singh N, Paterson DL. Aspergillus infections in transplant recipients. Clin Microbiol Rev 2005 Jan; 18(1): 44–69
Hellinger WC, Bonatti H, Yao JD, et al. Risk stratification and targeted antifungal prophylaxis for prevention of aspergillosis and other invasive mold infections after liver transplantation. Liver Transpl 2005 Jun; 11(6): 656–62
Gavalda J, Len O, San Juan R, et al. Risk factors for invasive aspergillosis in solid-organ transplant recipients: a case-control study. Clin Infect Dis 2005 Jul 1; 41(1): 52–9
Patterson JE. Epidemiology of fungal infections in solid organ transplant patients. Transpl Infect Dis 1999 Dec; 1(4): 229–36
Singh N. Impact of current transplantation practices on the changing epidemiology of infections in transplant recipients. Lancet 2003 Mar; 3(3): 156–61
Lortholary O, Meyohas MC, Dupont B, et al. Invasive aspergillosis in patients with acquired immunodeficiency syndrome: report of 33 cases. French Cooperative Study Group on Aspergillosis in AIDS. Am J Med 1993 Aug; 95(2): 177–87
Bruck HM, Nash G, Foley D, et al. Opportunistic fungal infection of the burn wound with phycomycetes and Aspergillus: a clinical-pathologic review. Arch Surg 1971 May; 102(5): 476–82
Stone HH, Cuzzell JZ, Kolb LD, et al. Aspergillus infection of the burn wound. J Trauma 1979 Oct; 19(10): 765–7
Becker WK, Cioffi Jr WG, McManus AT, et al. Fungal burn wound infection: a 10-year experience. Arch Surg 1991 Jan; 126(1): 44–8
Labbe AC, Su SH, Laverdiere M, et al. High incidence of invasive aspergillosis associated with intestinal graft-versus-host disease following nonmyeloablative transplantation. Biol Blood Marrow Transplant 2007 Oct; 13(10): 1192–200
Narreddy S, Mellon-Reppen S, Abidi MH, et al. Non-bacterial infections in allogeneic non-myeloablative stem cell transplant recipients. Transpl Infect Dis 2007 Mar; 9(1): 3–10
Thursky KA, Worth LJ, Seymour JF, et al. Spectrum of infection, risk and recommendations for prophylaxis and screening among patients with lymphoproliferative disorders treated with alemtuzumab. Br J Haematol 2006 Jan; 132(1): 3–12
Keating MJ, Flinn I, Jain V, et al. Therapeutic role of alemtuzumab (Campath-1H) in patients who have failed fludarabine: results of a large international study. Blood 2002 May 15; 99(10): 3554–61
Meersseman W, Van Wijngaerden E. Invasive aspergillosis in the ICU: an emerging disease. Intensive Care Med 2007 Oct; 33(10): 1679–81
Meersseman W, Vandecasteele SJ, Wilmer A, et al. Invasive aspergillosis in critically ill patients without malignancy. Am J Respir Crit Care Med 2004 Sep 15; 170(6): 621–5
Wisplinghoff H, Bischoff T, Tallent SM, et al. Nosocomial bloodstream infections in US hospitals: analysis of 24,179 cases from a prospective nationwide surveillance study. Clin Infect Dis 2004 Aug 1; 39(3): 309–17
Almirante B, Rodriguez D, Park BJ, et al. Epidemiology and predictors of mortality in cases of Candida bloodstream infection: results from population-based surveillance, Barcelona, Spain, from 2002 to 2003. J Clin Microbiol 2005 Apr; 43(4): 1829–35
Asmundsdottir LR, Erlendsdottir H, Gottfredsson M. Increasing incidence of candidemia: results from a 20-year nationwide study in Iceland. J Clin Microbiol 2002 Sep; 40(9): 3489–92
Laupland KB, Gregson DB, Church DL, et al. Invasive Candida species infections: a 5 year population-based assessment. J Antimicrob Chemother 2005 Sep; 56(3): 532–7
Poikonen E, Lyytikainen O, Anttila VJ, et al. Candidemia in Finland, 1995–1999. Emerg Infect Dis 2003 Aug; 9(8): 985–90
Sandven P, Bevanger L, Digranes A, et al. Candidemia in Norway (1991 to 2003): results from a nationwide study. J Clin Microbiol 2006 Jun; 44(6): 1977–81
Arendrup MC, Fuursted K, Gahrn-Hansen B, et al. Seminational surveillance of fungemia in Denmark: notably high rates of fungemia and numbers of isolates with reduced azole susceptibility. J Clin Microbiol 2005 Sep; 43(9): 4434–40
Diekema DJ, Messer SA, Brueggemann AB, et al. Epidemiology of candidemia: 3-year results from the emerging infections and the epidemiology of Iowa organisms study. J Clin Microbiol 2002 Apr; 40(4): 1298–302
Kao AS, Brandt ME, Pruitt WR, et al. The epidemiology of candidemia in two United States cities: results of a population-based active surveillance. Clin Infect Dis 1999 Nov; 29(5): 1164–70
Hajjeh RA, Sofair AN, Harrison LH, et al. Incidence of bloodstream infections due to Candida species and in vitro susceptibilities of isolates collected from 1998 to 2000 in a populationbased active surveillance program. J Clin Microbiol 2004 Apr; 42(4): 1519–27
Lin MY, Carmeli Y, Zumsteg J, et al. Prior antimicrobial therapy and risk for hospital-acquired Candida glabrata and Candida knisei fungemia: a case-case-control study. Antimicrob Agents Chemother 2005 Nov; 49(11): 4555–60
Abi-Said D, Anaissie E, Uzun O, et al. The epidemiology of hematogenous candidiasis caused by different Candida species. Clin Infect Dis 1997 Jun; 24(6): 1122–8
Antoniadou A, Torres HA, Lewis RE, et al. Candidemia in a tertiary care cancer center: in vitro susceptibility and its association with outcome of initial antifungal therapy. Medicine (Baltimore) 2003 Sep; 82(5): 309–21
Blumberg HM, Jarvis WR, Soucie JM, et al. Risk factors for candidal bloodstream infections in surgical intensive care unit patients: the NEMIS prospective multicenter study. The National Epidemiology of Mycosis Survey. Clin Infect Dis 2001 Jul 15; 33(2): 177–86
Eggimann P, Garbino J, Pittet D. Epidemiology of Candida species infections in critically ill non-immunosuppressed patients. Lancet Infect Dis 2003 Nov; 3(11): 685–702
Marr KA, Scidel K, White TC, et al. Candidemia in allogeneic blood and marrow transplant recipients: evolution of risk factors after the adoption of prophylactic fluconazole. J Infect Dis 2000 Jan; 181(1): 309–16
Pappas PG, Rex JH, Lee J, et al. A prospective observational study of candidemia: epidemiology, therapy, and influences on mortality in hospitalized adult and pediatric patients. Clin Infect Dis 2003; 37: 634–43
Wey SB, Mori M, Pfaller MA, et al. Risk factors for hospital-acquired candidemia: a matched case-control study. Arch Int Med 1989; 149(10): 2349–53
Martino P, Girmenia C, Micozzi A, et al. Prospective study of Candida colonization, use of empiric amphotericin B and development of invasive mycosis in neutropenic patients. Eur J Clin Microbiol Infect Dis 1994; 13(10): 797–804
Diekema DJ, Pfaller MA. Nosocomial candidemia: an ounce of prevention is better than a pound of cure. Infect Control Hosp Epidemiol 2004 Aug; 25(8): 624–6
Ostrosky-Zeichner L. Prophylaxis and treatment of invasive candidiasis in the intensive care setting. Eur J Clin Microbiol Infect Dis 2004 Oct; 23(10): 739–44
Paphitou NI, Ostrosky-Zeichner L, Rex JH. Rules for identifying patients at increased risk for candidal infections in the surgical intensive care unit: approach to developing practical criteria for systematic use in antifungal prophylaxis trials. Med Mycol 2005 May; 43(3): 235–43
Wenzel RP, Gennings C. Bloodstream infections due to Candida species in the intensive care unit: identifying especially high-risk patients to determine prevention strategies. Clin Infect Dis 2005 Sep 15; 41 Suppl. 6: S389–93
Pelz RK, Hendrix CW, Swoboda SM, et al. Double-blind placebo-controlled trial of fluconazole to prevent candidal infections in critically ill surgical patients. Ann Surg 2001 Apr; 233(4): 542–8
Leon C, Ruiz-Santana S, Saavedra P, et al. A bedside scoring system (“Candida score”) for early antifungal treatment in nonneutropenic critically ill patients with Candida colonization. Crit Care Med 2006 Mar; 34(3): 730–7
Ostrosky-Zeichner L, Sable C, Sobel J, et al. Multicenter retrospective development and validation of a clinical prediction rule for nosocomial invasive candidiasis in the intensive care setting. Eur J Clin Microbiol Infect Dis 2007 Apr; 26(4): 271–6
Pittet D, Monod M, Suter PM, et al. Candida colonization and subsequent infections in critically ill surgical patients. Ann Surg 1994 Dec; 220(6): 751–8
Dupont H, Bourichon A, Paugam-Burtz C, et al. Can yeast isolation in peritoneal fluid be predicted in intensive care unit patients with peritonitis? Crit Care Med 2003 Mar; 31(3): 752–7
Richet H, Roux P, Des Champs C, et al. Candidemia in French hospitals: incidence rates and characteristics. Clin Microbiol Infect 2002; 8: 405–12
Tortorano AM, Biraghi E, Astofi A, et al. European Confederation of Medical Mycology (ECMM) prospective survey of candidaemia: report from one Italian region. J Hosp Infect 2002; 51: 297–304
Marchetti O, Bille J, Fluckinger U, et al. Epidemiology of candidemia in Swiss tertiary care hospitals: secular trends, 1991–2000. Clin Infect Dis 2004; 38: 311–20
Chen YC, Chang SC, Luh KT, et al. Stable susceptibility of Candida blood isolates to fluconazole despite increasing use during the past 10 years. J Antimicrob Chemother 2003; 52: 71–7
Hsueh PR, Lau YJ, Chuang YC, et al. Antifungal susceptibilities of clinical isolates of Candida species, Cryptococcus neoformans, and Aspergillus species from Taiwan: surveillance of multicenter antimicrobial resistance in Taiwan program data from 2003. Antimicrob Agents Chemother 2005 Feb; 49(2): 512–7
Pfaller MA, Boyken L, Hollis RJ, et al. In vitro susceptibilities of Candida spp. to caspofungin: four years of global surveillance. J Clin Microbiol 2006 Mar; 44(3): 760–3
Colombo AL, Nucci M, Salomao R, et al. High rate of non-albicans candidemia in Brazilian tertiary care hospitals. Diagn Microbiol Infect Dis 1999 Aug; 34(4): 281–6
Pfaller MA, Messer SA, Boyken L, et al. Geographic variation in the susceptibilities of invasive isolates of Candida glabrata to seven systemically active antifungal agents: a global assessment from the ARTEMIS Antifungal Surveillance Program conducted in 2001 and 2002. J Clin Microbiol 2004; 42: 3142–6
Klevay MJ, Ernst EJ, Hollanbaugh JL, et al. Therapy and outcome of Candida glabrata versus Candida albicans bloodstream infection. Diagn Microbiol Infect Dis 2008 Mar; 60(3): 273–7
Gudlaugsson O, Gillespie S, Lee K, et al. Attributable mortality of nosocomial candidemia, revisited. Clin Infect Dis 2003 Nov 1;37(9): 1172–7
Pfaller MA, Diekema DJ, Gibbs DL, et al. Results from the ARTEMIS DISK Global Antifungal Surveillance study, 1997 to 2005: an 8.5-year analysis of susceptibilities of Candida species and other yeast species to fluconazole and voriconazole determined by CLSI standardized disk diffusion testing. J Clin Microbiol 2007 Jun; 45(6): 1735–45
Scifert H, Aurbach U, Stefanik D, et al. In vitro activities of isavuconazole and other antifungal agents against Candida bloodstream isolates. Antimicrob Agents Chemother 2007 May; 51(5): 1818–21
National Center for Biotechnology Information. The NCBI taxonomy homepage [online]. Available from URL: http://www.ncbi.nlm.nih.gov/Taxonomy/Browser/wwwtax.cgi?.id=475 [Accessed 2008 Jul 16]
De Pauw B, Walsh TJ, Donnelly JP, et al. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis 2008 Jun 15; 46(12): 1813–21
Kuhlman JE, Fishman EK, Siegelman SS. Invasive pulmonary aspergillosis in acute leukemia: characteristic findings on CT, the CT halo sign, and the role of CT in early diagnosis. Radiology 1985 Dec; 157(3): 611–4
Vandewoude KH, Blot SI, Depuydt P, et al. Clinical relevance of Aspergillus isolation from respiratory tract samples in critically ill patients. Crit Care 2006 Feb; 10(1): R31
Garnacho-Montero J, Amaya-Villar R. A validated clinical approach for the management of aspergillosis in critically ill patients: ready, steady, go! [letter]. Crit Care 2006; 10(2): 132
Hope WW, Walsh TJ, Denning DW. Laboratory diagnosis of invasive aspergillosis. Lancet Infect Dis 2005 Oct; 5(10): 609–22
Uffredi ML, Mangiapan G, Cadranel J, et al. Significance of Aspergillus fumigatus isolation from respiratory specimens of nongranulocytopenic patients. Eur J Clin Microbiol Infect Dis 2003 Aug; 22(8): 457–62
Husain S, Kwak EJ, Obman A, et al. Prospective assessment of Platelia Aspergillus galactomannan antigen for the diagnosis of invasive aspergillosis in lung transplant recipients. Am J Transplant 2004 May; 4(5): 796–802
Kwak EJ, Husain S, Obman A, et al. Efficacy of galactomannan antigen in the Platelia Aspergillus enzyme immunoassay for diagnosis of invasive aspergillosis in liver transplant recipients. J Clin Microbiol 2004 Jan; 42(1): 435–8
Digby J, Kalbfleisch J, Glenn A, et al. Serum glucan levels are not specific for presence of fungal infections in intensive care unit patients. Clin Diagn Lab Immunol 2003 Sep; 10(5): 882–5
Vardakas KZ, Michalopoulos A, Falagas ME. Fluconazole versus itraconazole for antifungal prophylaxis in neutropenic patients with haematological malignancies: a meta-analysis of randomised-controlled trials. Br J Haematol 2005 Oct; 131(1): 22–8
Glasmacher A, Cornely O, Ullmann AJ, et al. An open-label randomized trial comparing itraconazole oral solution with fluconazole oral solution for primary prophylaxis of fungal infections in patients with haematological malignancy and profound neutropenia. J Antimicrob Chemother 2006 Feb; 57(2): 317–25
Cornely OA, Maertens J, Winston DJ, et al. Posaconazole vs fluconazole or itraconazole prophylaxis in patients with neutropenia. N Engl J Med 2007 Jan 25; 356(4): 348–59
Vehreschild JJ, Böhme A, Buchheidt D, et al. A double-blind trial on prophylactic voriconazole (VRC) or placebo during induction chemotherapy for acute myelogenous leukaemia (AML). J Infect 2007 Nov; 55(5): 445–9
Cornely OA, Stollorz A, Beisel C, et al. Impact of posaconazole prophylaxis on the epidemiology of invasive aspergillosis. 47th Interscience Conference on Antimicrobial Agents and Chemotherapy; 2007 Sep 17–20; Chicago (IL)
Goodman JL, Winston DJ, Greenfield RA, et al. A controlled trial of fluconazole to prevent fungal infections in patients undergoing bone marrow transplantation. N Engl J Med 1992 Mar 26; 326(13): 845–51
Slavin MA, Osbome B, Adams R, et al. Efficacy and safety of fluconazole prophylaxis for fungal infections after marrow transplantation: a prospective, randomized, double-blind study. J Infect Dis 1995; 171(6): 1545–52
Wingard JR, Carter SL, Walsh TJ, et al. Results of a randomized, double-blind trial of fluconazole (FLU) vs voriconazole (VORI) for the prevention of invasive fungal infections (IFI) in 600 allogeneic blood and marrow transplant (BMT) Patients. ASH Annual Meeting; 2007 Dec 8–11; Atlanta (GA)
Ullmann AJ, Lipton JH, Vesole DH, et al. Posaconazole or fluconazole for prophylaxis in severe graft-versus-host disease. N Engl J Med 2007 Jan 25; 356(4): 335–47
Ullmann AJ, Heussel CP, Cornely OA. Voriconazole versus liposomal amphotericin B for empirical antifungal therapy. N Engl J Med 2002 May 30; 346(22): 1745–7; discussion 1747
Marr KA. Empirical antifungal therapy: new options, new tradeoffs. N Engl J Med 2002 Jan 24; 346(4): 278–80
Boogaerts M, Winston DJ, Bow EJ, et al. Intravenous and oral itraconazole versus intravenous amphotericin B deoxycholate as empirical antifungal therapy for persistent fever in neutropenic patients with cancer who are receiving broad-spectrum antibacterial therapy: a randomized, controlled trial. Ann Intern Med 2001 Sep 18; 135(6): 412–22
Link H, Böhme A, Cornely OA, et al. Antimicrobial therapy of unexplained fever in neutropenic patient: guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO). Ann Hematol 2003 Oct; 82 Suppl. 2: S105–17
Maertens J, Theunissen K, Verhoef G, et al. Galactomannan and computed tomography-based preemptive antifungal therapy in neutropenic patients at high risk for invasive fungal infection: a prospective feasibility study. Clin Infect Dis 2005 Nov 1; 41(9): 1242–50
Viscoli C, Herbrecht R, Akan H, et al. Caspofungin as first-line therapy of invasive aspergillosis in haematological patients: a study of the EORTC Infectious Diseases Group. Trends in Medical Mycology Congress 2007; 2007 Oct 28–31; Turin
van’t Wout JW, Novakova I, Verhagen CA, et al. The efficacy of itraconazole against systemic fungal infections in neutropenic patients: a randomised comparative study with amphotericin B. J Infect 1991 Jan; 22(1): 45–52
Caillot D, Bassaris H, McGeer A, et al. Intravenous itraconazole followed by oral itraconazole in the treatment of invasive pulmonary aspergillosis in patients with hematologic malignancies, chronic granulomatous disease, or AIDS. Clin Infect Dis 2001 Oct 15; 33(8): e83–90
Denning DW, Lee JY, Hostetler JS, et al. NIAID Mycoses Study Group multicenter trial of oral itraconazole therapy for invasive aspergillosis. Am J Med 1994 Aug; 97(2): 135–44
Ostrosky-Zeichner L. Combination antifungal therapy: a critical review of the evidence. Clin Microbiol Infect 2008 May; 14 Suppl. 4: 65–70
Eggimann P, Francioli P, Bille J, et al. Fluconazole prophylaxis prevents intra-abdominal candidiasis in high-risk surgical patients. Crit Care Med 1999 Jun; 27(6): 1066–72
Garbino J, Lew DP, Romand JA, et al. Prevention of severe Candida infections in nonneutropenic, high-risk, critically ill patients: a randomized, double-blind, placebo-controlled trial in patients treated by selective digestive decontamination. Intensive Care Med 2002 Dec; 28(12): 1708–17
Swoboda SM, Merz WG, Lipsetta PA. Candidemia: the impact of antifungal prophylaxis in a surgical intensive care unit. Surg Infect 2003 Winter; 4(4): 345–54
Cruciani M, de Lalla F, Mengoli C. Prophylaxis of Candida infections in adult trauma and surgical intensive care patients: a systematic review and meta-analysis. Intensive Care Med 2005 Nov; 31(11): 1479–87
Playford EG, Webster AC, Sorrell TC, et al. Antifungal agents for preventing fungal infections in non-neutropenic critically ill and surgical patients: systematic review and meta-analysis of randomized clinical trials. J Antimicrob Chemother 2006 Apr; 57(4): 628–38
Rex JH, Sobel JD. Prophylactic antifungal therapy in the intensive care unit. Clin Infect Dis 2001 Apr 15; 32(8): 1191–200
Ostrosky-Zeichner L, Sobel J, Pappas P, et al. Lessons from a multicenter, randomized, double-blind trial and insights into diagnostic performance of surrogate markers; M-1158. Interscience Conference on Antimicrobial Agents and Chemotherapy 2007; 2007 Sep 17–20; Chicago (IL)
Cruciani M, Mengoli C, Malena M, et al. Antifungal prophylaxis in liver transplant patients: a systematic review and meta-analysis. Liver Transpl 2006 May; 12(5): 850–8
Cruciani M, Serpelloni G. Management of Candida infections in the adult intensive care unit. Expert Opin Pharmacother 2008 Feb; 9(2): 175–91
Piarroux R, Grenouillet F, Balvay P, et al. Assessment of preemptive treatment to prevent severe candidiasis in critically ill surgical patients. Crit Care Med 2004 Dec; 32(12): 2443–9
Rex JH, Bennett JE, Sugar AM, et al. A randomized trial comparing fluconazole with amphotericin B for the treatment of candidemia in patients without neutropenia. Candidemia Study Group and the National Institute. N Engl J Med 1994 Nov 17; 331(20): 1325–30
Kullberg BJ, Sobel JD, Ruhnke M, et al. Voriconazole versus a regimen of amphotericin B followed by fluconazole for candidaemia in non-neutropenic patients: a randomised noninferiority trial. Lancet 2005 Oct 22–28; 366(9495): 1435–42
Kuse ER, Chetchotisakd P, da Cunha CA, et al. Micafungin versus liposomal amphotericin B for candidaemia and invasive candidosis: a phase III randomised double-blind trial. Lancet 2007 May 5; 369(9572): 1519–27
Pappas PG, Rotstein CM, Betts RF, et al. Micafungin versus caspofungin for treatment of candidemia and other forms of invasive candidiasis. Clin Infect Dis 2007 Oct 1; 45(7): 883–93
Reboli AC, Rotstein C, Pappas PG, et al. Anidulafungin versus fluconazole for invasive candidiasis. N Engl J Med 2007 Jun 14; 356(24): 2472–82
Greene RE, Schlamm HT, Oestmann JW, et al. Imaging findings in acute invasive pulmonary aspergillosis: clinical significance of the halo sign. Clin Infect Dis 2007 Feb 1; 44(3): 373–9
Walsh TJ, Anaissie EJ, Denning DW, et al. Treatment of aspergillosis: clinical practice guidelines of the Infectious Diseases Society of America. Clin Infect Dis 2008 Feb 1; 46(3): 327–60
Karthaus M. Treatment of aspergillosis. Clin Infect Dis 2008; 47(3): 427
Maertens J, Verhaegen J, Lagrou K, et al. Screening for circulating galactomannan as a noninvasive diagnostic tool for invasive aspergillosis in prolonged neutropenic patients and stem cell transplantation recipients: a prospective validation. Blood 2001 Mar 15; 97(6): 1604–10
Rovira M, Jimenez M, De La Bellacasa JP, et al. Detection of Aspergillus galactomannan by enzyme immunoabsorbent assay in recipients of allogeneic hematopoietic stem cell transplantation: a prospective study. Transplantation 2004 Apr 27; 77(8): 1260–4
Maertens J, Van Eldere J, Verhaegen J, et al. Use of circulating galactomannan screening for early diagnosis of invasive aspergillosis in allogeneic stem cell transplant recipients. J Infect Dis 2002 Nov 1; 186(9): 1297–306
Maschmeyer G, Beinert T, Buchheidt D, et al. Diagnosis and antimicrobial therapy of pulmonary infiltrates in febrile neutropenic patients: guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO). Ann Hematol 2003 Oct; 82 Suppl. 2: S118–26
Morrell M, Fraser VJ, Kollef MH. Delaying the empiric treatment of Candida bloodstream infection until positive blood culture results are obtained: a potential risk factor for hospital mortality. Antimicrob Agents Chemother 2005 Sep; 49(9): 3640–5
Garey KW, Rege M, Pai MP, et al. Time to initiation of fluconazole therapy impacts mortality in patients with candidemia: a multi-institutional study. Clin Infect Dis 2006 Jul 1; 43(1): 25–31
Magill SS, Shields C, Sears CL, et al. Triazole cross-resistance among Candida spp.: occurrence among bloodstream isolates, and implications for antifungal therapy [case report]. J Clin Microbiol 2006 Feb; 44(2): 529–35
Perlin DS. Resistance to echinocandin-class antifungal drugs. Drug Resist Updat 2007 Jun; 10(3): 121–30
Pfaller MA, Diekema DJ, Gibbs DL, et al. Geographic and temporal trends in isolation and antifungal susceptibility of Candida parapsilosis: a global assessment from the ARTEMIS DISK Antifungal Surveillance Program, 2001 to 2005. J Clin Microbiol 2008 Mar; 46(3): 842–9
van Burik JA, Ratanatharathorn V, Stepan DE, et al. Micafungin versus fluconazole for prophylaxis against invasive fungal infections during neutropenia in patients undergoing hematopoietic stem cell transplantation. Clin Infect Dis 2004 Nov 15; 39(10): 1407–16
Acknowledgements
The authors did not receive any funding or external help for the completion of this article. Dr Rüping has received travel grants from Schering-Plough/Essex and Gilead. Dr Vehreschild has received travel grants from Merck Sharp & Dohme/Merck, Pfizer, Schering-Plough and Viropharma. Dr Cornely is supported by the German Federal Ministry of Research and Education (BMBF grant 01KN0706) and has received research grants from, is an advisor to, or served at the speakers’ bureau of Astellas, Basilea, Bayer, F2G, Genzyme, Gilead, Pfizer, Merck, Mölnlycke, Nektar, Optimer, Schering-Plough, SpePharm, United Medical, Vicuron and Zeneus.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rüping, M.J.G.T., Vehreschild, J.J. & Cornely, O.A. Patients at High Risk of Invasive Fungal Infections. Drugs 68, 1941–1962 (2008). https://doi.org/10.2165/00003495-200868140-00002
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-200868140-00002