Summary
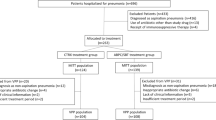
In phase I of a 2-phase study, 56 evaluable children (0.8 to 5 years) with lobar or segmental pneumonia received intravenous or intramuscular ceftriaxone 50 mg/kg/day for 2 days followed by oral cefetamet pivoxil 20 mg/kg/day in 2 divided doses to complete 7 days of treatment. All patients achieved a clinical cure.
In phase II, a randomised open multicentre study, 62 children with pneumonia received an identical regimen to phase I (arm A), and 59 children received ceftriaxone 50 mg/kg/day for 1 day followed by 6 days’ treatment with cefetamet pivoxil 20 mg/kg/day (arm B). Patients from phase I and arm A were combined giving a total of 118 evaluable patients in arm A.
At the end of treatment, 100% of patients in arm A and 96% in arm B achieved a clinical cure; cure was maintained in 99 and 98% of patients, respectively. Two (4%) patients in arm B failed therapy; in both cases, factors other than treatment failure may have accounted for the poor response.
11 and 12% of patients in treatment arms A and B, respectively, experienced adverse events; gastrointestinal events (nausea and/or vomiting) were reported in 9 and 8% of patients, respectively.
In conclusion, 1 or 2 days’ treatment with parenteral ceftriaxone before switching to oral cefetamet pivoxil was safe and effective in the treatment of childhood pneumonia. Therefore, parenteral-oral switch is a feasible treatment option in the treatment of serious paediatric community-acquired pneumonia.
Similar content being viewed by others
References
Berman S. Epidemiology of acute respiratory infections in children of developing countries. Reviews of Infectious Diseases 13 (Suppl. 6): 454–462, 1991
Chartrand SA. New concepts for antimicrobial use in respiratory infections. Seminars in Pediatric Infectious Disease 2: 18–26, 1991
Cullmann W, Edwards DJ, Kissling M, Kneer J, Stoeckel K, et al. Cefetamet pivoxil: a review of its microbiology, tox icology, pharmacokinetics and clinical efficacy. International Journal of Antimicrobial Agents 1: 175–192, 1992
Dagan R, Einhorn MS. A program of outpatient parenteral antibiotic therapy for serious pediatric bacterial infections. Reviews of Infectious Diseases 13 (Suppl. 2): 152–156, 1991
Dagan R, Phillip M, Watemberg NM, Kassis I. Outpatient treatment of serious community-acquired pediatrie infections using once daily intramuscular ceftriaxone. Pediatrie Infectious Disease Journal 6: 1080–1084, 1987
Doern GV, Jones RN. Antimicrobial susceptibility testing of Haemophilus influenzae, Branhamella catarrhalis and Neisseria gonorrhoeae. Antimicrobial Agents and Chemotherapy 32: 1747–1753, 1988
Doern GV, Jorgensen JH, Thornsberry C, Preston DA, Tubert T, et al. National collaborative study of the prevalence of antimicrobial resistance among clinical isolates of Haemophilus influenza. Antimicrobial Agents and Chemotherapy 32: 180–185, 1988
Ejlertsen T, Schonheyder HC, Thisted E. β-Lactamase production in Branhamella catarrhalis isolated from lower respiratory tract infections in Danish children: an increasing problem. Infection 19: 329–330, 1991
Fass RJ, Helsel VL. In vitro activities of Ro 19-5247 and Ro 15-8074, new oral cephalosporins. Antimicrobial Agents and Chemotherapy 30: 429–434, 1986
Forgie IM, o’Neill KP, Lloyd-Evans N, Leinonen M, Campbell H, et al. Etiology of acute lower respiratory tract infections in Gambian children. I. Acute lower respiratory tract infections in infants presenting at the hospital. Pediatrie Infectious Disease Journal 10: 33–41, 1991a
Forgie IM, o’Neill KP, Lloyd-Evans N, Leinonen M, Campbell H, et al. Etiology of acute lower respiratory tract infections in Gambian children. II. Acute lower respiratory tract infection in children aged one to nine years presenting at the hospital. Pediatrie Infectious Disease Journal 10: 42–47, 1991b
Greenwood BM, Greenwood AM, Bradley AK, Tulloch S, Hayes R, et al. Deaths in infancy and early childhood in a well vaccinated, rural, West African population. Annals of Tropical Paediatrics 7: 91–99, 1987
Gwatkin DR. How many die? A set of demographic estimates of the annual number of infants and child deaths in the world. American Journal of Public Health 70: 1286–1289, 1980
Jacobs MR, Koornhof HJ, Robins-Browne RM, Stevenson CM, Vermaak ZA, et al. Emergence of multiply resistant pneumococci. New England Journal of Medicine 299: 735–740, 1978
Keeley DJ, Nkrumah FK, Kapuyaniyika C. Randomized trial of sulfamethoxazole + trimethoprim versus procaine penicillin for the outpatient treatment of childhood pneumonia in Zimbabwe. Bulletin of the World Health Organization 68: 185–192, 1990
Klugman KP, Koornhof HJ. Drug resistance patterns and serogroups or serotypes of pneumococcal isolates from cerebrospinal fluid or blood, 1979–1986. Journal of Infectious Diseases 158: 956–964, 1988
Leibovitz E, Tabachnik E, Fliedel O, Steinberg S, Miskin A, et al. Once daily intramuscular ceftriaxone in the outpatient treatment of severe community-acquired pneumonia in children. Clinical Pediatrics 29: 634–639, 1990
Neu HC, Chin NX, Labthavikul P. In vitro activity and β-lactamase stability of two oral cephalosporins, ceftetrame (Ro 19-5247) and cefetamet (Ro 15-8074). Antimicrobial Agents and Chemotherapy 30: 423–428, 1986
Nohlynek H, Eskola J, Laine E, Halonen P, Ruutu P, et al. The causes of hospital-treated acute lower respiratory tract infection in children. American Journal of Diseases of Children 145: 618–622, 1991
Schutze GE, Jacobs RF. Management of community-acquired bacterial pneumonia in hospitalized children. Pediatric Infectious Disease Journal 11: 160–164, 1992
Shawn F. Etiology of severe pneumonia in children in developing countries. Pediatric Infectious Disease Journal 5: 247–252, 1986
Turner RB, Lande AE, Chase P, Hilton N, Weinberg D. Pneumonia in pediatrie outpatients: cause and clinical manifestations. Journal of Pediatrics 111: 194–200, 1987
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Dagan, R., Syrogiannopoulos, G., Ashkenazi, S. et al. Parenteral-Oral Switch in the Management of Paediatric Pneumonia. Drugs 47 (Suppl 3), 43–51 (1994). https://doi.org/10.2165/00003495-199400473-00008
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-199400473-00008