Summary
Clofazimine is useful in the treatment of Hansen’s disease (leprosy) and some dermatological disorders, and is currently being used in drug regimens for patients with human immunodeficiency viral infections who are also infected with Mycobacterium avium complex.
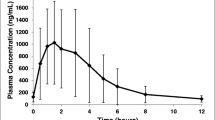
After an oral dose, absorption is variable, but when given in an oil-wax suspension is approximately 70%. Administration with food appears to increase the peak plasma drug concentration and reduce the time to peak level. Data on the volume of distribution and percentage or type of protein binding are not available; however, the drug undergoes extensive tissue distribution. Clofazimine does not cross the blood-brain barrier, but does cross the placenta, and is found in human breast milk.
To date 3 urinary metabolites have been identified in man, but their biological activity is unknown. A substantial portion of the unchanged drug is excreted in faeces. The elimination half life is variable, with values as long as 70 days being quoted in the literature.
Frequently reported side effects of clofazimine are hyperpigmentation of the skin and conjunctiva, and abdominal pain. These resolve upon cessation of therapy. Biochemical and haematological adverse effects have been reported, but are generally not clinically relevant. Pharmacokinetic drug interactions of potential clinical significance have been observed with dapsone, oestrogen, rifampicin and vitamin A.
Similar content being viewed by others
References
Acocella G. Clinical pharmacokinetics of rifampicin. Clinical Pharmacokinetics 3: 108–127, 1978
Armstrong D, Gold JWM, Dryjanski J, Whimbey E, Polsky B, et al. Treatment of infections in patients with the acquired immunodeficiency syndrome. Annals of Internal Medicine 103: 738–743, 1985
Baciewicz AM, Self TM. Rifampicin drug interactions. Southern Medical Journal 78: 714–718, 1985
Baciewicz AM, Self TM, Bekemeyer WB. Update on rifampicin drug interactions. Archives of Internal Medicine 147: 565–568, 1987
Bajaj AK, Gupta SC, Sinha SN, Govil DC, Gaur UC. Renal functional status in lepromatous leprosy. International Journal of Leprosy 49: 37–41, 1981
Banerjee DK, Ellard GA, Gammon PT, Waters MFR. Some observations on the pharmacology of clofazimine (B663). American Journal of Tropical Medicine and Hygiene 23: 1110–1119, 1974
Barry VC, Buggle K, Byrne J, Conalty ML, Winder F. Absorption, distribution and retention of amino-compounds in the experimental animal. Irish Journal of Medical Science 416: 345–352, 1960
Belaube P, Devaux J, Pizzi M, Boutboul R, Privat Y. Small bowel deposition of crystals associated with the use of clofazimine in the treatment of prurigo nodularis. International Journal of Leprosy 51: 328–330, 1983
Bharadwaj VP, Sritharan V, Venkatesan K, Girdhar A, Ramu G. Vitamin A levels of ichthyotic and non-ichthyotic skin and plasma of leprosy patients with and without clofazimine therapy. Indian Journal of Medical Research 75: 773–777, 1982
Browne SG, Harman DJ, Waudby A, McDougall AC. Clofazimine the treatment of lepromatous leprosy in the United Kingdom: a 12 year review of 31 cases, 1966–1978. International Journal of Leprosy 49: 167–176, 1981
Browne SG, Hogerzeil LM. B663 in the treatment of leprosy: preliminary report of a pilot trial. Leprosy Review 33: 6–16, 1962
Centers for Disease Control. Diagnosis and management of mycobacterial infection and disease in persons with human T-lymphotrophic virus type III/lymphadenopathy associated virus infection. Morbidity Mortality Weekly 35: 448–452, 1986
Centers for Disease Control. AIDS and HIV among health care workers. Morbidity Mortality Weekly 37: 229–234, 1988
Chuaprapcislis T, Piamphongsant T. Treatment of pustular psoriasis with clofazimine. British Journal of Dermatology 99: 303–305, 1978
deBergeyck E, Janssens PG, de Muynck A. Radiological abnormalities of the ileum associated with the use of clofazimine in the treatment of skin ulceration due to Mycobacterium ulcerans. Leprosy Review 51: 221–228, 1980
Desikan KV, Balakrishnan S. Tissue levels of clofazimine in a case of leprosy. Leprosy Reviews 47: 107–113, 1976
Dill WA, Chricot L, Glazkio AJ. A new analytical procedure for B663 (clofazimine). International Journal of Leprosy 38: 355–356, 1970
Duncan ME, Oakey RE. Reduced estrogen excretion due to clofazimine. International Journal of Leprosy 51: 112–113, 1983
Farb H, West DP, Pedvis-Leftick A. Clofazimine in pregnancy complicated by leprosy. Obstetrics and Gynecology 59: 122–123, 1982
Feng PCC, Fenselau CC, Jacobson RR. Metabolism of clofazimine in leprosy patients. Drug Metabolism and Disposition 9: 521–524, 1981
Feng PCC, Fenselau CC, Jacobson RR. A new urinary metabolite of clofazimine in leprosy patients. Drug Metabolism and Disposition 10: 286–288, 1982
Fenselau CC, Pallante S, Parikh I. Solid phase synthesis of drug glucuronides by immobilized glucuronosyltransferase. Journal of Medicinal Chemistry 19: 679–683, 1976
Grabosz JAJ, Wheate HW. Effect of clofazimine on the urinary excretion of dapsone. International Journal of Leprosy 43: 61–62, 1975
Granstein RD, Sober AJ. Drug and heavy metal-induced hyper-pigmentation. Journal of the American Academy of Dermatology 5: 1–18, 1981
Greene JB, Sidhu GS, Lewin S, Levine JF, Masur H, et al. Mycobacterium avium-intracellulare: a cause of disseminated life threatening infection in homosexuals and drug abusers. Annals of Internal Medicine 97: 539–546, 1982
Gidoh M, Tsutsumi S. Determination of 3 main antileprosy drugs and their metabolites in serum by HPLC. Journal of Chromatography — Biomedical Applications 223: 379–392, 1981
Hastings RC, Jacobson RR, Trautman JR. Long term clinical toxicity studies with clofazimine in leprosy. International Journal of Leprosy 44: 287–293, 1976
Hawkins CC, Gold JWM, Whimbey E, Kiehn TE, Brannon P, et al. Mycobacterium avium complex infection in patients with the acquired immunodeficiency syndrome. Annals of Internal Medicine 105: 184–188, 1986
Holdiness MR. Clinical pharmacokinetics of the antituberculosis drugs: a review. Clinical Pharmacokinetics 9: 511–544, 1984a
Holdiness MR. Mycobacterium avium-intracellulare infection. Southern Medical Journal 77: 1614, 1984b
Holdiness MR. Adverse cutaneous reactions to antituberculosis drugs: a review. International Journal of Dermatology 24: 280–285, 1985a
Holdiness MR. Cerebrospinal fluid pharmacokinetics of the antituberculosis drugs. Clinical Pharmacokinetics 10: 532–534, 1985b
Holdiness MR. Rifampicin adverse cutaneous reactions. International Journal of Dermatology 25: 72–73, 1986a
Holdiness MR. Contact dermatitis to ethambutol. Contact Dermatitis 15: 96–97, 1986b
Holdiness MR. Contact dermatitis to the antituberculosis drugs: a review. Contact Dermatitis 15: 282–288, 1986c
Holdiness MR. Neurological manifestations and toxicities of the antituberculosis drugs: a review. Medical Toxicology 2: 33–51, 1987a
Holdiness MR. Teratology of the antituberculosis drugs: a review. Early Human Development 15: 61–74, 1987b
Holdiness MR. Transplacental pharmacokinetics of the antituberculosis drugs. Clinical Pharmacokinetics 13: 125–129, 1987c
Holdiness MR. A review of iatrogenic nutritional deficiencies induced by antituberculosis drugs. Nutrition Research 7: 891–900, 1987d
Holdiness MR. Rifampicin drug interactions. Archives of Internal Medicine 147: 1856, 1987e
Holdiness MR. Blood dyscrasias induced by the antituberculosis drugs: a review. Tubercle 68: 301–309, 1987f
Holdiness MR. Ethionamide. In Dollery C. (Ed.) Therapeutic drugs: a clinical pharmacopoeia, Churchill Livingstone, Edinburgh, 1988a
Holdiness MR. Prothionamide. In Dollery C. (Ed.) Therapeutic drugs: a clinical pharmacopoeia, Churchill Livingstone, Edinburgh, 1988b
Holdiness MR. Thiacetazone. In Dollery C. (Ed.) Therapeutic drugs: a clinical pharmacopoeia, Churchill Livingstone, Edinburgh, 1988c
Holdiness MR. Clofazimine in pregnancy. Early Human Development 16: in press, 1988d
Horsburgh CR, Mason UG, Farhi DC, Iseman MD. Disseminated infection with Mycobacterium avium-intracellulare. Medicine 64: 36–48, 1984
Jacobson RR. Treatment. In Hastings (Ed.) Leprosy, pp. 193–222, Churchill Livingstone, Edinburgh, 1985
Jopling WH. Complications of treatment of clofazimine. Leprosy Review 47: 1–3, 1976
Karat ABA. Long term follow up of clofazimine in the management of reactive phases of leprosy. Leprosy Review 46s: 105–109, 1975
Kenny MT, Strates B. Metabolism and pharmacokinetics of the antibiotic rifampicin. Drug Metabolism Review 12: 159–218, 1981
Lanyi Z, Dubois JP. Determination of clofazimine in human plasma by TLC. Journal of Chromatography — Biomedical Applications 232: 219–223, 1982
Levy L. Pharmacologic studies of clofazimine. American Journal of Tropical Medicine and Hygiene 23: 1097–1109, 1974
Mackey JP. Clofazimine in dermatology. International Journal of Dermatology 15: 140–141, 1976
Mansfield RE. Tissue concentrations of clofazimine in man. American Journal of Tropical Medicine and Hygiene 23: 1116–1119, 1974
Masur H, Tuazon C, Gill V, Grimes G, Baird B, et al. Effect of combined clofazimine and ansamycin therapy on Mycobacterium avium-Mycobacterium intracellular bacteremia in patients with AIDS. Journal of Infectious Diseases 155: 127–129, 1987
Mehta J, Gandhi IS, Sane SB, Wamburkar MN. Effects of clofazimine and dapsone of rifampicin pharmacokinetics in multibacillary leprosy cases. Leprosy Review 57s: 67–76, 1986
Moore VJ. A review of side effects experienced by patients taking clofazimine. Leprosy Review 54: 327–335, 1983
Negrel AD, Chovet M, Baquillon G, Lagadec R. Clofazimine and the eye: preliminary communication. Leprosy Review 55: 349–352, 1984
Noorden SK. The epidemiology of leprosy. In Hastings R. (Ed.) Leprosy, pp. 15–30, Churchill Livingstone, Edinburgh, 1985
Parikh I, MacGlashan DW, Fenselau CC. Immobilized glucuronsyltransferase for the synthesis of conjugates. Journal of Medicinal Chemistry 19: 296–299, 1976
Pavithran K. Exfoliative dermatitis after clofazimine. International Journal of Leprosy 53: 645–646, 1985
Peters JH, Hamme KJ, Gordon GR. Determination of clofazimine in plasma by HPLC. Journal of Chromatography — Biomedical Applications 229: 503–508, 1982
Pfaltzgraff RE. The control of neuritis in leprosy with clofazimine. International Journal of Leprosy 40: 392–398, 1972
Revill WDL, Morrow RH, Pike MC, Ateng J. A controlled trial of the treatment of Mycobacterium ulcerans infection with clofazimine. Lancet 2: 873–877, 1973
Rosmusen I. Pyoderma gangrenosum treatment with clofazimine. Clinical evaluation of 7 cases. Acta Dermato-Venereologica 63: 552–553, 1983
Sansarricq H. Leprosy in the world today. Leprosy Review 54s: 7–16, 1983
Schaad-Lanyi Z, Dieterle W, Dubois JP, Theobald W, Vischer W. Pharmacokinetics of clofazimine in healthy human volunteers. International Journal of Leprosy 55: 9–15, 1987
Venencie PY, Cortez A, Orieux G, Jost JL, Chomette G, et al. Clofazimine enteropathy. Journal of the American Academy of Dermatology 15: 290–291, 1986
Venkatesan K, Bharadwaj VP, Ramu G, Desikan KV. Study on drug interactions. Leprosy in India 52: 229–236, 1980
Venkatesan K, Mathur A, Girdhan BK, Bharadwaj VP. The effect of clofazimine on the pharmacokinetics of rifampicin and dapsone in leprosy. Journal of Antimicrobial Chemotherapy 18: 715–718, 1986
Vischer WA. The experimental properties of G30,320 (B633). Leprosy Review 40: 107–111, 1969
Wallace JM, Hannah JB. Mycobacterium avium complex infection in patients with the acquired immunodeficiency syndrome. Chest 93: 926–932, 1988
Woods GL, Washington JA. Mycobacteria other than Mycobacterium tuberculosis: review of the microbiological and clinical aspects. Review of Infectious Diseases 9: 275–294, 1987
Working Party on B663: Symposium on B663 (Lamprene, Geigy) in the treatment of leprosy and leprosy reactions. International Journal of Leprosy 36: 560–561, 1968
World Health Organization. Expert committee on leprosy 1977 fifth report. World Health Organization Technical Report Series Number 607, 1977
World Health Organization. Chemotherapy of leprosy for control programs. Report of a WHO study group. World Health Organization Technical Series Number 675, 1982
Yajko DM, Nassos PS, Hadley WK. Therapeutic implications of inhibition versus killing of Mycobacterium avium complex by antimicrobial agents. Antimicrobial Agents and Chemotherapy 31: 117–120, 1987
Yawalkar SJ, Vischer W. Lamprene (clofazimine) in leprosy. Leprosy Reviews 50: 135–144, 1979
Young LS. Mycobacterium avium complex infection. Journal of Infectious Diseases 157: 863–867, 1988
Zuidema J, Hilbers-Modderman ESM, Merkus FWHM. Clinical pharmacokinetics of dapsone. Clinical Pharmacokinetics 11: 299–315, 1986
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Holdiness, M.R. Clinical Pharmacokinetics of Clofazimine. Clin-Pharmacokinet 16, 74–85 (1989). https://doi.org/10.2165/00003088-198916020-00002
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003088-198916020-00002