Abstract
BD750, a novel JAK3/STAT5 inhibitor, can inhibit T cell proliferation. This study aims to evaluate whether BD750 can induce tolerogenic dendritic cells (tolDC) and their function in experimental autoimmune encephalitis (EAE) in mice. Following BD750 treatment, lipopolysaccharide (LPS)-induced maturation of DCs, allogeneic T cell proliferation, Th1 and Th17 cell functional differentiation, and STAT5 and AKT activation were determined. The effect of tolDC loaded with antigen peptide on the development and severity of EAE and splenic Th1 and Th17 cell responses was determined. In comparison with LPS-induced mature DCs (mDCs), BD750 treatment induced tolDC with lower expression levels of costimulatory molecules and proinflammatory cytokines and lower levels of STAT5 phosphorylation. TolDC inhibited allogeneic T cell proliferation and reduced Th1 and Th17 responses. Adoptive transfer of tolDC loaded with myelin oligodendrocyte glycoprotein35-55 inhibited the development and severity of EAE in mice, accompanied by reduced numbers of inflammatory infiltrates and decreased levels of demyelination in the spinal cord tissues. In addition, treatment with tolDC loaded with antigen peptide also significantly reduced the frequency of splenic Th1 and Th17 cells in EAE mice. The effects of tolDC were similar to that of JAK/STAT inhibitor CP690550-treated DCs. In conclusion, treatment with BD750 induced tolDC that inhibited proinflammatory T cell immunity in vitro and in vivo. BD750 and tolDC may be valuable for development of new therapies for EAE and other autoimmune diseases.
Similar content being viewed by others
Introduction
Multiple sclerosis (MS) is a chronic inflammatory demyelinating disease in the central nervous system (CNS), predominantly mediated by autoreactive CD4+ Th1 and Th17 cells. During the pathogenic process of MS, autoreactive CD4+ T cells pass through the blood-brain barrier and migrate into the brain and spinal cord to cause demyelination in the CNS (1,2). Together with defects in the function of regulatory T cells (Tregs) in patients with MS, this enhances pathogenic Th1 and Th17 responses within the brain (3). Therefore, reestablishing antigen-specific tolerance will be of great significance in managing patients with MS (4).
Dendritic cells (DCs) are professional antigen-presenting cells (APCs) and can induce naïve T cell activation. Mature DCs present peptide of antigens by major histocompatibility complex (MHC) molecules and express high levels of costimulatory molecules, such as CD80, CD83, CD86 and CD40, on their surface to provide two necessary signals for full T cell activation. Inflammatory DCs can secrete IL-12, IL-6, TGF-β and IL-23, which promote Th1 or Th17 polarization (5). The levels of proinflammatory cytokines produced by DCs largely depend on the maturation status, ranging from fully mature immunogenic DCs to tolerogenic immature DCs, spanning a wide variety of intermediate semi-mature states. Tolerogenic DCs (tolDC) are usually resistant to maturation, with lower levels of costimulatory molecule expression and inflammatory cytokine production, but higher levels of inhibitory molecule expression. tolDC can induce anergy and apoptosis of effector T cells, but promote Treg responses (6,7). Adoptive transfer of tolDC is a new strategy to restore immune tolerance and may be a therapeutic strategy for autoimmune diseases (8,9). Treatment with type II collagen-pulsed tolDC (dexamethasone/vitamin D3-modified) decreases the percentages of pathogenic Th17 cells in arthritic mice and reduces the severity and progression of arthritis (10). Furthermore, H471-94 peptide-loaded tolDC augments suppressive function of Tregs, suppresses Th17 cells and benefits patients with lupus (11). In addition, tolDC generated in vitro inhibit the process of experimental autoimmune encephalitis (EAE) in mice (12). More importantly, tolDC from relapsing-remitting MS patients can induce stable antigen-specific hyporesponsiveness in myelin-reactive T cells (13).
Induction of tolDC has been experimentally achieved by suppressive agents, including IL-10 and TGF-β; immunomodulatory drugs, such as dexamethasone and vitamin D; and genetic modification (14). Our previous study identified that a benzothiazole derivative, BD750 [2-(2-benzothiazoleyl)-4,5,6,7-tetrahydro-2H-indazol-3-ol, C14H13N3OS, MW: 271.3], is an inhibitor of JAK3/STAT5 signaling and can inhibit T cell proliferation (15). JAK3 is crucial for the maturation of DCs, and JAK3−/− DCs fail to induce T cell proliferation (16,17). STAT5 is crucial for thymic stromal lymphopoietin-dependent DC activation and can upregulate the expression of costimulatory molecules and chemokines (18). Accordingly, we hypothesize that BD750 may induce tolDC, which may inhibit antigen-specific Th1 and Th17 responses and the pathogenic process of EAE in mice. In the current study, we tested the effect of BD750 on the maturation and function of DCs in vitro and the impact of adoptive transfer of BD750-treated DCs on Th1 and Th17 responses in EAE mice. We found that BD750 induced tolDC that impaired allogenic antigen-stimulated T cell responses in vitro. Furthermore, adoptive transfer of tolDC that had been loaded with antigen peptide inhibited Th1 and Th17 responses and the development of EAE in mice. Our findings may aid in the design of new therapies for MS.
Materials and Methods
Animals and Animal Models
C57BL/6 and BALB/c mice were purchased from Dashuo Biotechnology (Chengdu, China). The experimental protocols were approved by the Animal Care and Use Committee at Chengdu Medical College. All mice were bred and maintained in a specific pathogen-free facility in the Experimental Animal Center of Chengdu Medical College at consistent room temperatures (20–26°C) and humidity (approximately 40–70%), with a 12 h/12 h light/dark cycle.
Female C57BL/6 mice (10 wks old, 19–21 g) were used for the experiments aimed at investigating the therapeutic effect of BD750-treated DCs on the development and progression of EAE. Animals were randomized by simple randomization into seven groups (n = 8 mice per group). The mice were immunized subcutaneously at the dorsal flanks with 200 µg myelin oligodendrocyte glycoprotein (MOG)35-55 peptide (China-Peptides, Shanghai, China) emulsified 1:1 with complete Freund’s adjuvant (CFA) supplemented with 4 mg/mL heat-killed Mycobacterium tuberculosis (Chondrex, Redmond, WA, USA). Individual mice were injected intraperitoneally with 500 ng pertussis toxin (PTX) on d 0 and 2. One group of mice received adjuvant and PTX only and served as the control. The mice were monitored daily for clinical symptoms, which were scored as: 0, no clinical signs; 1, paralyzed tail; 2, loss of coordinated movement, hind limb paresis; 3, both hind limbs paralyzed; 4, forelimbs paralyzed; and 5, moribund (19).
Generation of Murine Bone Marrow-Derived Dendritic Cells
Murine bone marrow-derived dendritic cells (BMDCs) were isolated from female C57BL/6 mice (6 wks old, 16–18 g), as described previously (20). Briefly, the animals were anesthetized with intraperitoneal injection of sodium pentobarbital and euthanized by cervical disconnection. Subsequently, their femur and tibia bones were cut with scissors and the marrow was flushed out, followed by passing through a nylon mesh to remove small pieces of bone and debris. The resulting single cells (1 × 106 cells/dish) were cultured in 10% fetal calf serum RPMI 1640 (complete medium) for 4 h. The suspended cells were removed and the adherent cells were cultured in complete medium containing 20 ng/mL of recombinant granulocyte-macrophage colony-stimulating factor and 10 ng/mL of IL-4 (PeproTech) for 6 d. The cells were exposed to fresh medium every 3 d. On d 6 post-incubation, the cells were harvested and some cells were stained with fluorescent-labeled antibodies, followed by flow cytometry analysis. The CD11c+ immature DCs in the remaining cells were purified by magnetic anti-CD11c beads (Miltenyi). The purified immature DCs were pretreated with BD750 or vehicle dimethyl sulfoxide for 12 h, ensuring that the dimethyl sulfoxide was <0.025%. The cells were then stimulated with 100 ng/mL lipopolysaccharide (LPS) to induce DC maturation for 24 h.
Allogeneic Mixed Leukocyte Reaction
To test the effect of BD750-treated DCs on stimulating T cell proliferation, naïve splenic CD4+CD69− T cells were isolated from female BALB/c mice (6 wks old, 17–19 g) using a T cell isolation kit (Miltenyi) and labeled with carboxyfluorescein diacetate succinimidyl ester (1.2 µM; Invitrogen). The naïve T cells were cocultured in triplicate with allogeneic BD750 pretreated DCs (BD750-mDC) at three DC:T cell ratios (1:10, 1:30, 1:100) for 72 h. The proliferation of activated T cells was analyzed by flow cytometry.
Flow Cytometry
The mature DCs were stained in duplicate with fluorescent-labeled antibodies against CD11c, CD69, CD83, CD40, CD80, CD86, MHC II or isotype-matched controls (BioLegend, San Diego, CA, USA). The maturation status of DCs was analyzed by flow cytometry. Some mature DCs were analyzed for their apoptosis by flow cytometry using the PI Annexin V Apoptosis Detection Kit I (BD Pharmingen) according to the manufacturers’ instruction.
In addition, the functional phenotypes of CD4+ T cells were analyzed by flow cytometry. Briefly, after mixed leukocyte reaction (MLR) coculture, CD4+ T cells were separated from the cell culture, then treated with anti-CD16/32 (Mouse BD Fc Block™), stained with fluorescein isothiocyanate-anti-CD4, fixed, permeabilized and intracellularly stained with PE-conjugated anti-IFN-γ and Alexa Fluor® 647-conjugated anti-IL-17, followed by flow cytometry. Moreover, Tregs were analyzed by flow cytometry using the Transcription Factor Buffer Set (BD Pharmingen), after being stained with APC-anti-CD25 and intracellularly with PE-anti-Foxp3, according to the manufacturer’s instructions. All flow cytometry was performed in the Accuri™ C6 (BD Biosciences) or Cytomics FC 500 (Beckman Coulter).
Enzyme-Linked Immunosorbent Assay
The supernatants of cultured DCs or DCs cocultured with T cells were harvested and the levels of IL-6, IL-10, IL-12, TNF-α, IL-1β, IL-23, IFN-γ and IL-17 in the supernatants were determined by enzyme-linked immunosorbent assay (ELISA) using specific kits (eBioscience), according to the manufacturer’s instructions. Briefly, the control and experimental samples were simultaneously tested in triplicate, and the plates were read at 450 nm (Powerwave XS, BioTek, Winooski, VT, USA).
Western Blotting
The purified immature DCs were pretreated with BD750 (1, 5 or 20 µM), CP690550 (1 µM), LY294002 (1 µM) or vehicle for 12 h. The cells were stimulated with 100 ng/mL LPS to induce DC maturation for 24 h. The harvested mature DCs were lysed in radioimmunoprecipitation assay buffer (Millipore), and the protein concentrations in the lysates were determined using a BCA Protein Assay Kit (BioTek). Individual cell lysate samples (20 µg/lane) were separated by electrophoresis on 10% sodium dodecyl sulfate-polyacrylamide gels and transferred onto polyvinylidene difluoride membranes (Millipore, Bedford, MA, USA). After being blocked with 5% bovine serum albumin, the membranes were incubated with specific antibodies against STAT5, phospho-STAT5, Akt, phospho-Akt or GAPDH (Cell Signaling Technology). The bound antibodies were detected with horseradish peroxidase-conjugated second antibodies (Santa Cruz Biotech, Santa Cruz, CA, USA) and visualized by enhanced chemiluminescence (Millipore). The relative levels of target proteins were normalized to the internal GAPDH and analyzed using ImageJ software.
Adoptive Transfer Experiments
Immature DCs at 6 d post-culture were pretreated with BD750 (20 µM) for 12 h. The cells were pulsed with MOG35-55 (20 µg/mL) for 24 h and subsequently treated with LPS (100 ng/mL) to induce DC maturation for 24 h. The cells were harvested and injected intravenously into mice at −2, 2 and 6 or 7, 11 and 15 d post first PTX injection (1 × 106 cells/mouse). The control mice were injected with PBS.
Histological Analysis
At 22 d post-induction, the mice were anesthetized with intraperitoneal injection of sodium pentobarbital and perfused with PBS (pH 7.4), followed by 4% (w/v) paraformaldehyde. Spinal cord samples were then fixed in 4% (w/v) paraformaldehyde overnight and paraffin-embedded. The coronal sections (5 µm) of cervicothoracic spinal cord tissues were stained with hematoxylin and eosin and examined for cellular infiltration or with Luxol fast blue/periodic acid-Schiff to determine demyelination.
Statistical Analysis
The data are expressed as mean ± standard error of the mean. The differences among the groups were evaluated using analysis of variance and post hoc least significant different t test or Kruskal-Wallis test using PRISM 6.0 software (GraphPad Software, San Diego, CA, USA). A P value < 0.05 was considered statistically significant.
All supplementary materials are available online at https://doi.org/www.molmed.org.
Results
BD750 Treatment Induces tolDC
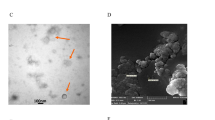
Mature dendritic cells (mDCs) possess numerous dendrites that may be of great advantage to interaction with T cells (21). In this study, we first examined the effect of BD750 treatment on the maturation and survival of DCs in vitro. Treatment with a low dose of BD750 (1 µM) did not change the morphology of mDCs, and both mDCs that had been treated with low-dose BD750 and vehicle displayed large clusters of adherent cells with sharp cytoplasmic projections. In contrast, most mDCs that had been treated with BD750 (5 or 20 µM) or CP690550, a JAK inhibitor, had fewer small dendrites and smaller clusters than typical mDCs (Figure 1A). However, treatment with BD750 did not change the frequency of spontaneous mDC apoptosis (Figures 1B, C). Hence, treatment with a higher dose of BD750 altered the morphology of mDC, but did not change the frequency of spontaneous mDC apoptosis in vitro.
Morphological characteristics and survival of typical mDCs and BD750-treated DCs. BMDCs were stimulated with cytokines and treated with or without BD750 at the indicated dose or CP690550 for 12 h and then further stimulated with LPS for 24 h. The imDCs, mDCs and BD750-treated DCs were observed by a light microscope, and the percentages of apoptotic DCs in different groups of cells were determined by flow cytometry analysis. Data are representative images or expressed as the mean ± SEM of three independent experiments. (A) Light microscopic analysis of different groups of DCs. (B) Flow cytometry analysis of apoptotic cells. (C) Quantitative analysis of apoptotic cells. *P < 0.05, **P < 0.01 versus the mDC group.
Next, we analyzed whether BD750 could change the maturation of DCs. DCs were stimulated and generated at d 6 post stimulation as immature DCs (imDCs), and further stimulated with LPS for maturation as mDCs. Some imDCs were treated with or without BD750 or CP690550 alone. Subsequently, the supernatants of cultured DCs were harvested and the cells were stained with fluorescent-labeled antibodies to analyze the levels of CD69, CD40, CD80, CD83, CD86 and I-Ab expression by flow cytometry. ImDCs expressed very low levels of each molecule tested relative to mDCs (Figure 2). Furthermore, DCs that had been treated with BD750 at concentrations of 5 and 20 µM but not 1 µM displayed significantly reduced levels of each molecule relative to mDC. Similarly, treatment with CP690550 further significantly reduced the levels of each molecule in DCs.
Analysis of maturation status of BD750-treated DCs by flow cytometry. After different treatments, the different groups of DCs were stained with the indicated antibodies and the levels of surface molecule expression were determined by flow cytometry. Data are representative histograms or expressed as the mean ± SEM of three independent experiments. (A) Flow cytometry analysis. (B) Quantitative analysis. *P < 0.05, **P < 0.01 versus the mDC group.
Analysis of cytokines indicated that treatment with BD750 at a higher dose or with CP690550 significantly reduced the levels of LPS-stimulated IL-6, IL-12, TNF-α, IL-1β and IL-23 production by DCs (Figures 3A, C-F). BD750 did not modulate cytokine secretion of IL-10, even at a high concentration of 20 µM (Figure 3B). Western blot analysis revealed that while treatment with LPS significantly induced STAT5 and AKT phosphorylation in DCs, treatment with BD750 or CP690550 significantly inhibited STAT5 but not AKT phosphorylation in cultured DCs (Figures 3G, H). Hence, treatment with BD750 at a higher dose induced tolDC in vitro, which was associated with inhibiting the LPS-induced JAK-STAT5 signaling in DC.
BD750 inhibits proinflammatory cytokine secretion and STAT5 phosphorylation in DCs. BMDCs were stimulated with cytokines for expansion in the presence or absence of BD750 for 12 h and then stimulated with LPS for 24 h. The supernatants of cultured cells were harvested and the levels of IL-6, IL-10, IL-12, TNF-α, IL-1β and IL-23 in the supernatants were determined by ELISA (A-F). In addition, the relative levels of STAT5 and AKT expression and phosphorylation in the different groups of DCs were determined by Western blot assays (G-H). The relative levels of STAT5 and AKT phosphorylation to total STAT5 and AKT were determined. The relative density for bands of p-STAT5 or p-AKT activity was normalized to the total STAT5 or AKT, respectively. Data are representative images or expressed as the mean ± SEM of three independent experiments. *P < 0.05, **P < 0.01 versus the mDC group.
BD750-Treated DC Functionally Impairs Allogenic T Cell Responses In Vitro
To investigate the immunoregulatory capacity of BD750-treated DCs, imDCs, mDCs and BD750-treated DCs were cocultured with allogeneic naïve CD4+CD69− T cells for 3 d. The T cell proliferation induced by allogenic antigens was analyzed by flow cytometry. While mDC stimulated strong allogenic T cell proliferation, BD750-treated DC impaired allogenic antigen-stimulated T cell proliferation in vitro in a dose-dependent manner (Figure 4). A stronger inhibition of allogenic antigen-stimulated T cell proliferation was observed when mDC was treated with CP690550.
BD750-treated DC impairs allogeneic antigen-stimulated T cell proliferation in vitro. ImDCs, mDCs and BD750-pretreated DCs (12 h) were mixed in triplicate with carboxyfluo-resceinsuccinimidyl ester-labeled allogeneic naive CD4+CD25− T cells for 72 h at different ratios (DC:CD4 + T, 1:10, 1:30 and 1:100), and the proliferation of T cells was determined by flow cytometry. Data are representative histograms or expressed as the mean ± SEM of three independent experiments. (A) Flow cytometry analysis. (B-D) Quantitative analysis. *P < 0.05, **P < 0.01 versus the mDC group.
Flow cytometry characterization indicated that while mDC induced high frequency of Th1 and Th17 cells, DCs that had been treated with BD750 or CP690550 induced significantly lower frequency of Th1 and Th17 cells and slightly higher frequency of Tregs relative to mDC (Figures 5A-D). Further analysis revealed that high levels of IL-17A and IFN-γ were secreted by activated T cells cocultured with mDC and significantly lower levels of IL-17A and IFN-γ were detected in the supernatants of cocultured T cells with DC treated with a high dose of BD750 or with CP690550 (Figure 5E, F). The BD750-treated and CP690550-treated DCs also significantly increased the level of IL-10 in the supernatants cocultured with T cells, compared with mDCs. Together, BD750-treated DCs impaired allogenic antigen-stimulated T cell proliferation and functional differentiation in vitro.
BD750-treated DC impairs allogeneic antigen-stimulated Th1 and Th17 responses in vitro. Following MLR in vitro, the frequency of Th1 and Th17 cells and Tregs was determined by flow cytometry. The levels of IL-17A and IFN-γ in the supernatants of cocultured T and DC cells were determined by ELISA. Data are representative FACS charts or expressed as the mean ± SEM of three independent experiments. (A) Flow cytometry analysis of Th1 and Th17 cells and Tregs. (B-D) Quantitative analysis of Th1 and Th17 cells and Tregs. (E-G) ELISA analysis of the levels of IL-17A, IFN-γ and IL-10. *P < 0.05, **P < 0.01 versus the mDC group.
Adoptive Transfer of BD750-Treated DC Inhibits the Development and Reduces the Severity of EAE in Mice
To examine the potent immunosuppressive ability of BD750-treated DC, C57BL/6 mice were immunized subcutaneously with MOG35-55 in CFA (4 mg/mL Mycobacterium tuberculosis) and injected with PTX. One week after induction, the mice were randomized and injected intravenously with PBS as the control, MOG35-55-pulsed and BD750 (20 µM)-treated DC on d 7, 11 and 15 post the first PTX injection (dpi 7, 11 and 15) (Figure 6A). The development and severity of EAE in individual groups of mice were monitored daily. In comparison with the mice receiving PBS, the mice receiving DC treated with 20 µM BD750 and loaded with antigen peptide displayed delayed EAE development and reduced severity of EAE (Figure 6A). In addition, we found that adoptive transfer of tolDC without MOG35-55 did not improve EAE (Figure 6B). Moreover, delayed adoptive transfer of tolDC loaded with antigen peptide at dpi 19, 23 and 27 or adoptive transfer of tolDC loaded with antigen peptide for 1–2 times failed to effectively inhibit EAE development in mice (Figures 6C, D). More interestingly, adoptive transfer with BD750-treated DC at dpi −2, 2 and 6 greatly inhibited development of EAE in mice (Figure 6C). Histological analysis of the spinal cord sections at peak disease (dpi 22) also indicated that treatment with BD750-treated and antigen-loaded tolDC, but not tolDC without antigen, reduced inflammatory infiltrates and demyelination intensity in mice (Figure 6E). Further analysis of splenic T cells indicated that adoptive transfer with tolDC that had been treated with 20 µM BD750 significantly reduced the frequency of Th1 and Th17 cells and increased the percentage of Tregs compared with mice receiving PBS (Figure 7). Thus, adoptive transfer with BD750-treated DC significantly inhibited T cell autoimmunity and EAE development in mice.
Treatment with BD750-treated DC ameliorates EAE. C57BL/6 mice were immunized with MOG35-55 peptide in CFA and PTX. (A) The mice were randomized and treated intravenously with 20 µM BD750 pretreated DC (12 h) loaded with MOG35_55 on d 7, 11 and 15 post the first PTX injection. Data are shown as the mean ± SEM of each group (n = 8 per group), *P < 0.05 versus the PBS group. (B) The EAE mice were treated intravenously with 20 µM BD750-treated DCs loaded with or without MOG35-55 on d 7, 11 and 15 post the first PTX injection. Data are shown as the mean ± SEM of each group (n = 8 per group). *P < 0.05 versus the DC (20 µM BD750) without MOG35-55 loading group. (C) The EAE mice were treated intravenously with 20 µM BD750-treated DCs loaded with MOG35-55 on d 7, 11 and 15 or delayed on 19, 23 and 27 d or earlier on d −2, 2 and 6 post the first PTX injection. Data are shown as the mean ± SEM of each group (n = 8 per group). *P < 0.05 versus the tolDC intravenous (dpi 19, 23 and 27) group. (D) The EAE mice were treated intravenously with 20µM BD750-treated DC loaded with MOG35-55 on d 7, 11 and 15 post induction only for 1–2 times. Data are shown as the mean ± SEM of each group (n = 8 per group). *P < 0.05 versus the tolDC intravenous (dpi 7) group. The dynamic progression of EAE in individual groups of mice was monitored daily by two researchers without knowing the groups in a Plinded manner, and some mice from some groups of mice were euthanized at 22 d post induction for analysis of inflammation and demyelination in the spinal cord tissues. (E) Histological examinations, Arrows indicate inflammatory infiltrates. Scale Par, 100µm (magnification 100 ×).
Adoptive transfer of BD750-treated DC decreases the proportion of splenic Th1 and Th17 cells and Tregs in EAE mice. On d 22 post the first PTX injection, some mice from each group were euthanized and their splenic T cells were stained with anti-CD4/anti-CD25, intracellularly stained with anti-IL-17A, anti-IFN-γ or anti-Foxp3. The percentages of splenic Th1 and Th17 cells and Tregs were determined by flow cytometry. Data are representative FACS charts or expressed as the mean ± SEM of each group of mice (n = 8 per group). (A) Flow cytometry analysis. (B) Quantitative analysis of the percentages of Th1 and Th17 cells and Tregs. *P < 0.05, **P < 0.01 versus the PBS group.
Discussion
DCs are the most powerful APCs and induce antigen-specific T cell responses (22,23). Mature DCs are powerful for inducing T cell activation, and immature DCs usually promote T cell tolerance. Previous studies have shown that tolDC can inhibit autoimmune diseases, such as rheumatoid arthritis and EAE, in rodents (24,25). Indeed, pharmacological modification is a new strategy to induce tolDC (10,26). It is well known that the JAK/STAT pathway is crucial for the maturation and tolerance of DCs (16). Inhibition of STAT5 can impair the maturation of monocyte-derived DCs with downregulated expression of costimulatory molecules and reduced secretion of IL-12 (27,28). Our previous study identified that BD750 is an inhibitor of JAK3/STAT5 and can inhibit T cell proliferation (15). In this study, we found that BD750 induced tolDC. Evidentially, BD750-treated DCs displayed typically immature morphology. Second, BD750-treated DCs had lower levels of costimulatory molecule and MHC II expression and secreted lower levels of proinflammatory cytokines following LPS activation in vitro. Furthermore, BD750-treaed DCs impaired allogeneic antigen-stimulated T cell proliferation, accompanied by lower frequency of proinflammatory Th1 and Th17 cells and STAT5 phosphorylation. Its inhibitory effect was similar to that of CP690550. Given that tolDC are important to induce T cell tolerance, BD750 may be a valuable agent for inducing T cell tolerance. Notably, BD750 inhibited STAT5 activation but not AKT phosphorylation, consistent with our previous findings (15). This observation suggests that BD750 may be a specific inhibitor of STAT5. We are interested in further examining the molecular mechanisms underlying the action of BD750 in regulating T cell immunity.
Myelin-specific Th1 and Th17 cells are responsible for the pathogenesis of EAE and MS. To understand the potential regulatory role of BD750-induced tolDC, we adoptively transferred antigen peptide-loaded tolDC during the development of EAE in mice. We found that adoptive transfer with antigen peptide-loaded tolDC, particularly at the early stage of inducing EAE, significantly delayed the development of EAE and reduced its severity in mice. Furthermore, treatment with tolDC also reduced inflammatory infiltrates and the degree of demyelination in the spinal cords of mice. Given that tolDC are relatively stable in phenotype and function (13), autologous tolDC may be valuable for inducing T cell tolerance (29). Although it might be difficult for tolDC to pass the CNS (26), they did inhibit splenic Th1 and Th17 responses in EAE mice, similar to a previous report (26). In addition, although BD750 did not affect IL-10 production by LPS-stimulated DCs, BD750-DC secreted a low level of IL-12. A previous study reported that decreased IL-12 production of tolDC plays an important role in inducing Treg differentiation (25), so BD750-DC secreted a low level of IL-12, which could enhance tolDC-mediated Tregs differentiation in MLR and subsequently expand the Treg population.
tolDC induced T cell tolerance, dependent on antigen peptide loading. Therefore, tolDC loaded with antigen peptide may be promising for inhibiting T cell autoimmunity and EAE progression. Our data indicate that adoptive transfer with antigen peptide-loaded tolDC should start at the early stage of the disease process. We speculate that this was because antigen-specific T cell response in the CNS was possibly the first demyelinating event. Similarly, we found that continual transfer of tolDC loaded with antigen peptide was necessary for the control of disease progression. Because MS is a chronic disease, it is also very difficult for us to speculate the long-term efficacy of passive transfer therapy and how frequently therapy is necessary to control disease progression. Therefore, further investigations are warranted to determine the safety and effectiveness of tolDC-based immunotherapies for MS.
Conclusion
Our data indicate that BD750 induced tolDC by downregulating their costimulatory molecule expression and cytokine production. BD750-treated DCs impaired allogeneic antigen-stimulated T cell proliferation. BD750-modified DCs induced hyporesponsiveness and impaired proinflammatory cytokine secretion by allogeneic T cells in MLR. In addition, the tolDC pulsed with MOG35-55 effectively attenuated autoantigen-specific Th1/Th17 differentiation, and adoptive transfer of tolDC loaded with antigen peptide inhibited autoimmune responses in a mouse model of MS. Therefore, our findings may provide new insights into inducible immune tolerance and aid in the design of new therapies for MS.
Disclosure
The authors declare that they have no competing interests as defined by Molecular Medicine, or other interests that might be perceived to influence the results and discussion reported in this paper.
References
Pelletier D, Hafler DA. (2012) Fingolimod for multiple sclerosis. New Engl. J. Med. 366:339–47.
Compston A, Coles A. (2008) Multiple sclerosis. Lancet. 372:1502–17.
Viglietta V, Baecher-Allan C, Weiner HL, Hafler DA. (2004) Loss of functional suppression by CD4+CD25+ regulatory T cells in patients with multiple sclerosis. J. Exper. Med. 199:971–9.
Gross CC, Jonuleit H, Wiendl H. (2012) Fulfilling the dream: tolerogenic dendritic cells to treat multiple sclerosis. Eur. J. Immunol. 42:569–72.
Steinman RM. (2012) Decisions about dendritic cells: past, present, and future. Annu. Rev. Immunol. 30:1–22.
Steinman RM, Hawiger D, Nussenzweig MC. (2003) Tolerogenic dendritic cells. Annu. Rev. Immunol. 21:685–711.
Torres-Aguilar H, Blank M, Jara LJ, Shoenfeld Y. (2010) Tolerogenic dendritic cells in autoimmune diseases: crucial players in induction and prevention of autoimmunity. Autoimmun. Rev. 10:8–17.
Price S. (2010) Therapeutic effects of tolerogenic dendritic cells. Nat. Rev. Rheumatol. 6:674.
Llanos C, Mackern-Oberti JP, Vega F, Jacobelli SH, Kalergis AM. (2013) Tolerogenic dendritic cells as a therapy for treating lupus. J. Clin. Immunol. 148:237–45.
Stoop JN, et al. (2010) Therapeutic effect of tolerogenic dendritic cells in established collagen-induced arthritis is associated with a reduction in Th17 responses. Arthritis Rheum. 62:3656–65.
Kang HK, Liu M, Datta SK. (2007) Low-dose peptide tolerance therapy of lupus generates plasmacytoid dendritic cells that cause expansion of autoantigen-specific regulatory T cells and contraction of inflammatory Th17 cells. J. Immunol. 178:7849–58.
Farias AS, et al. (2013) Vitamin D3 induces IDO+ tolerogenic DCs and enhances Treg, reducing the severity of EAE. CNS Neurosci. Ther. 19:269–77.
Raiotach-Regue D, et al. (2012) Stable antigen-specific T-cell hyporesponsiveness induced by tolerogenic dendritic cells from multiple sclerosis patients. Eur. J. Immunol. 42:771–82.
Matsumoto T, et al. (2013) Protein kinase C inhibitor generates stable human tolerogenic dendritic cells. J. Immunol. 191:2247–57.
Liu Y, et al. (2013) BD750, a benzothiazole derivative, inhibits T cell proliferation by affecting the JAK3/STAT5 signalling pathway. Brit. J. Pharmacol. 168:632–43.
Rivas-Caicedo A, et al. (2009) Jak3 is involved in dendritic cell maturation and CCR7-dependent migration. PLoS One 4:e7066.
Zhou Y, et al. (2016) Tolerogenic dendritic cells generated with tofacitinib ameliorate experimental autoimmune encephalomyelitis through modulation of Th17/Treg balance. J. Immunol. Res. 2016:5021537.
Bell BD, et al. (2013) The transcription factor STAT5 is critical in dendritic cells for the development of TH2 but not TH1 responses. Nat. Immunol. 14:364–71.
Stromnes IM, Goverman JM. (2006) Active induction of experimental allergic encephalomyelitis. Nat. Protoc. 1:1810–19.
Inaba K, et al. (1992) Generation of large numbers of dendritic cells from mouse bone marrow cultures supplemented with granulocyte/macrophage colony-stimulating factor. J. Exper. Med. 176:1693–702.
Yanagawa Y, Onoe K. (2002) CCL19 induces rapid dendritic extension of murine dendritic cells. Blood. 100:1948–56.
Tanaka H, Demeure CE, Rubio M, Delespesse G, Sarfati M. (2000) Human monocyte-derived dendritic cells induce naive T cell differentiation into T helper cell type 2 (Th2) or Th1/Th2 effectors. Role of stimulator/responder ratio. J. Exper. Med. 192:405–12.
Segura E, et al. (2013) Human inflammatory dendritic cells induce Th17 cell differentiation. Immunity. 38:336–48.
Harry RA, Anderson AE, Isaacs JD, Hilkens CM. (2010) Generation and characterisation of therapeutic tolerogenic dendritic cells for rheumatoid arthritis. Ann. Rheum. Dis. 69:2042–50.
Sonobe Y, et al. (2012) Midkine inhibits inducible regulatory T cell differentiation by suppressing the development of tolerogenic dendritic cells. J. Immunol. 188:2602–11.
Mansilla MJ, et al. (2015) Beneficial effect of tolerogenic dendritic cells pulsed with MOG autoantigen in experimental autoimmune encephalomyelitis. CNS Neurosci. Therap. 21:222–30.
van de Laar L, et al. (2011) Tight control of STAT5 activity determines human CD34-derived interstitial dendritic cell and langerhans cell development. J. Immunol. 186:7016–24.
Toniolo PA, et al. (2015) Inhibiting STAT5 by the BET bromodomain inhibitor JQ1 disrupts human dendritic cell maturation. J. Immunol. 194:3180–90.
Giannoukakis N, Phillips B, Finegold D, Harnaha J, Trucco M. (2011) Phase I (safety) study of autologous tolerogenic dendritic cells in type 1 diabetic patients. Diabetes Care. 34:2026–32.
Acknowledgments
We thank Medjaden Bioscience Limited for assisting in the preparation of this manuscript. This work was supported by grants from the National Natural Science Foundation of China (nos. 81202363, 81302786, 81273530), the Research Fund of Development and Regeneration Key Laboratory of Sichuan Province (no. SYS16-002), the Program for Provincial Universities Innovative Research Team in Sichuan Province (no. 13TD0028), the Innovative Research Team Fund of Chengdu Medical College (no. CYTD15-01), the Scientific Research Fund of Sichuan Provincial Education Department (no. 16ZB0271) and the National Undergraduates Innovating Experimentation Project (no. 201513705005).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, and provide a link to the Creative Commons license. You do not have permission under this license to share adapted material derived from this article or parts of it.
The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this license, visit (https://doi.org/creativecommons.org/licenses/by-nc-nd/4.0/)
About this article
Cite this article
Zhou, Y., Leng, X., Li, H. et al. Tolerogenic Dendritic Cells Induced by BD750 Ameliorate Proinflammatory T cell Responses and Experimental Autoimmune Encephalitis in Mice. Mol Med 23, 204–214 (2017). https://doi.org/10.2119/molmed.2016.00110
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.2119/molmed.2016.00110