Abstract
Hyperactivation of signal transducer and activator of transcription 3 (STAT3) has been linked to tumorigenesis in most malignancies, including head and neck squamous cell carcinoma. Intravenous delivery of a chemically modified cyclic STAT3 decoy oligonucleotide with improved serum and thermal stability demonstrated antitumor efficacy in conjunction with downmodulation of STAT3 target gene expression such as cyclin D1 and Bcl-XL in a mouse model of head and neck squamous cell carcinoma. The purpose of the present study was to determine the toxicity and dose-dependent antitumor efficacy of the cyclic STAT3 decoy after multiple intravenous doses in Foxn1 nu mice in anticipation of clinical translation. The two doses (5 and 10 mg/kg) of cyclic STAT3 decoy demonstrated a significant decrease in tumor volume compared with the control groups (mutant cyclic STAT3 decoy or saline) in conjunction with downmodulation of STAT3 target gene expression. There was no dose-dependent effect of cyclic STAT3 decoy on tumor volume or STAT3 target gene expression. There were no significant changes in body weights between the groups during the dosing period, after the dosing interval or on the day of euthanasia. No hematology or clinical chemistry parameters suggested toxicity of the cyclic STAT3 decoy compared with saline control. No gross or histological pathological abnormalities were noted at necropsy in any of the animals. These findings suggest a lack of toxicity of intravenous administration of a cyclic STAT3 decoy oligonucleotide. In addition, comparable antitumor effects indicate a lack of dose response at the two dose levels investigated.
Similar content being viewed by others
Introduction
Signal transducer and activator of transcription 3 (STAT3) is frequently activated in a diverse range of human cancers, including head and neck squamous cell carcinoma (1). Cytokineinduced intracellular signaling through members of the STAT3 pathway plays an essential role in regulating many genes linked to proliferation, angiogenesis, metastasis and survival, among other phenotypes (1,2). Stimulation by a wide variety of growth factors or cytokines mediates cell surface receptor dimerization leading to the activation of Janus kinases (JAKs), which in turn phosphorylate and activate cytoplasmic STAT proteins. Activated STATs translocate to the nucleus, where they bind to specific DNA response elements in the promoter regions of target genes and induce the expression of proteins such as Bcl-XL, c-Myc, cyclin D1 and VEGF (3,4).
Cumulative evidence supports a critical role for STAT3 in cancer development and progression, highlighting STAT3 as an attractive therapeutic target (5,6). Various approaches have been proposed to block STAT3 signaling, although few have reached clinical testing. Phosphotyrosinebased peptidomimetic inhibitors have been shown to target the SH2 domain and block STAT3 dimerization (5,7). A dominant-negative form of STAT3, STAT3β, abrogated activated STAT3 and suppressed growth and invasion in human lung cancer cells (8). G-quartet oligodeoxynucleotides have been shown to inhibit interleukin-6-stimulated STAT3 activation by interacting with the SH2 domain of STAT3 (9). A double-stranded, linear STAT3 decoy oligonucleotide, targeting activated STAT3, disrupted binding of STAT3 to DNA sequences on a variety of STAT3-responsive promoters. This STAT3 decoy inhibited proliferation and STAT3-mediated gene expression in head and neck squamous cell carcinoma (HNSCC) (10), as well as other cancers (11–13). Several natural products are also under development to target STAT3, including curcumin, resveratrol and cucurbitacin, among others, although these agents lack specificity (5).
Few STAT3 inhibitory strategies have undergone toxicology testing. WP1066, an inhibitor of the JAK2/STAT3 pathway, showed acute and chronic toxicity in mice treated at doses >40 mg/kg, and, hence, the maximum tolerated dose selected ranged from 20 to 40 mg/kg (14). WHI-P131, a potent and selective inhibitor of JAK3, was well tolerated in a study with three cynomolgus monkeys at a dose level ranging from 20 to 100 mg/kg (15). The toxicological effects of ISIS 481464, a constrained ethyl modified phosphorothioate antisense oligonucleotide targeting STAT3, have been studied both in mice and cynomolgus monkeys (16). The toxicity profile of ISIS 481464 was similar to the antisense oligonucleotide containing 2′-O-methoxyethylribose modification, and no new toxicity was revealed (16). The toxicity study of the linear STAT3 decoy oligonucleotide conducted in a nonhuman primate model demonstrated no acute toxicity, and the no-observable adverse-effect level was >3.2 mg/kg, suggesting that direct injection of the STAT3 decoy does not cause local or systemic abnormalities (4). However, thermal and enzymatic instability of the linear STAT3 decoy has limited its application in the clinic to intratumoral administration. Thus, we linked the double strands of the linear STAT3 decoy by using hexaethylene glycol spacers to generate a cyclic STAT3 decoy (17). The cyclic STAT3 decoy demonstrated increased thermal and nuclease stability (17). Further, the cyclic STAT3 decoy bound to STAT3 protein with high affinity, inhibited cellular viability, demonstrated antitumor efficacy and reduced STAT3 target gene expression in cancer cells both in vitro and in vivo (17). In anticipation of implementing a clinical trial in HNSCC patients, the present study was undertaken to test the biological efficacy and safety of systemic administration of the cyclic STAT3 decoy. Systemic administration of the cyclic STAT3 decoy in tumor-bearing mice demonstrated antitumor effects at either of two dose levels, with no apparent dose-dependency observed in measurements of tumor volumes or STAT3 target gene expression. The potential toxicity of the cyclic STAT3 decoy was determined after multiple intravenous doses in mice. Although STAT3 was shown to be upregulated in cancers, the physiological importance of STAT3 in normal development raises concerns that targeting STAT3 may have toxic side effects. We found that the no-observable-adverse-effect level of cyclic STAT3 decoy is 100 mg/kg.
Materials and Methods
The cyclic STAT3 decoy was generated by linking the double-stranded oligonucleotide strands of the linear STAT3 decoy with hexaethylene glycol spacers (Oligos Etc., Wilsonville, OR, USA), followed by enzymatic ligation of the 3′ and 5′ ends of the oligonucleotides, as previously described (17). The control, mutant cyclic STAT3 decoy differed by one nucleotide, position 9 (G to T), and was deficient in binding STAT3. The cyclic STAT3 decoy and the mutant cyclic STAT3 decoy were formulated in saline (Baxter Healthcare Corporation, Deerfield, IL, USA). For the toxicity study, cyclic STAT3 decoy was ligated to result in stock concentrations of 10 mg/mL (100 mg/kg), 6.7 mg/mL (67 mg/kg) and 3.3 mg/mL (33 mg/kg). Before administration, a sample of each stock, sufficient for dosing on that day, was removed from the stock vials and placed into cryovials to ensure the stock solutions at each dose level were not contaminated during the study. The dose levels for this maximum tolerated dose study were selected to be approximately 20-, 13.4- and 6.6-fold higher than the daily efficacious doses of the cyclic STAT3 decoy (17).
Animals
Toxicity study. Female Foxn1 nu/Foxn1+ heterozygous nude mice (20 mice, 4–6 wks of age) were purchased from Harlan Sprague-Dawley (Indianapolis, IN, USA). Mice were allowed to acclimate to the University of Pittsburgh Animal Facility for at least 1 wk before initiation of the studies to assure that the mice were healthy. To minimize exogenous infection, mice were maintained in microisolator cages and handled in accordance with the Guide for the Care and Use of Laboratory Animals (18; National Research Council, 2011) and on a protocol approved by the University of Pittsburgh IACUC. The 20 mice were stratified into four different treatment groups (five mice/group): 100, 67 or 33 mg/kg cyclic STAT3 decoy or vehicle (saline; 0.01 mL/g body weight), such that there were no differences in body weights between the treatment groups. Doses were administered once daily on d 1–5 and d 8–12 followed by 10 d of observation. Doses on each dosing day were 0.01 mL/g exact body weight, as determined on that day. Clinical observations and body weights were recorded daily during dosing and twice weekly for 14 d after dosing.
Blood and tissue collection. Mice were euthanized by CO2 inhalation 10 d following the last day of cyclic STAT3 decoy or vehicle administration. Following euthanasia, blood was collected by cardiac puncture and organs and tissues were evaluated at necropsy for any gross abnormalities. The following organs were examined and pieces of each tissue were placed in cassettes and stored in 10% phosphate-buffered formalin in anticipation of being embedded in paraffin and sectioned into 5-µm sections for hematoxolin and eosin staining: bone (femur), bone marrow (sternum, rib, costochondral junction), brain, cecum, colon, duodenum, esophagus, eyes, gall bladder, gonads, heart, ileum, jejunum, kidneys, liver, lungs, lymph nodes (bronchial, mandibular, and mesenteric), pancreas, thyroid and parathyroid glands, salivary gland, sciatic nerve, skeletal muscle (biceps femoris), skin (ventral abdomen) and mammary gland, spinal cord (thoracolumbar), spleen, stomach (cardiac, fundic, and pyloric), thymus, trachea, urinary bladder and uterus. Upon gross examination, all of the tissues from the treatment and control groups appeared normal and no gross lesions were observed in any of the groups.
Histopathological exam of all tissues was performed by an experienced pathologist (LW). Each lesion was listed and coded by the most specific topographical and morphological diagnoses, severity and distribution using the Pathology Terminology Guidelines of the Toxicology Data Management system (TDMS) for the National Toxicology Program. Microscopic findings were graded semiquantitatively according to the following scale. Minimal (grade 1) represented the least detectable lesion; mild (grade 2) represented an easily discernible lesion unlikely to have any biological significance; moderate (grade 3) represented a change affecting a large area of the represented tissue that had the potential to be of some significance; and grade 4 was reserved for lesions that approached a theoretical maximum in severity, with entire tissue involvement (that is, hepatocellular necrosis affecting practically all hepatocytes in every section).
Hematology and clinical chemistry. Blood was collected by cardiac puncture using 3-cc syringes and 1.5-inch 22-gauge needles and divided into tubes supplied by Marshfield Laboratories (Marshfield, WI, USA). The samples were sent to Marshfield Laboratories for hematology and clinical chemistry analyses. An Olympus 860 was used for the clinical chemistry analyses, and hematology was performed by using the Cell Dyn 3500 Hemotology Analyzer. However, for small samples and differentials, manual assessments were done.
Dose-response therapeutic efficacy study. Female athymic nude mice nu/nu (4-6 wks old; 20 g; Harlan Sprague Dawley) were inoculated subcutaneously on the right flank with an HNSCC cell line (UM-SCC1) (3 × 106 cells per mouse). Once the tumors were palpable, the mice were randomized into five group containing 10 mice/group and injected intravenously once a day with cyclic STAT3 decoy (5 or 10 mg/kg), mutant cyclic STAT3 decoy (5 or 10 mg/kg) or saline for a period of 2 wks. During the treatment period, tumors were measured three times a week by using two-dimensional vernier calipers. At the end of the treatment period, the xenograft tumors were harvested and analyzed by immunoblotting for the expression levels of cyclin D1 and Bcl-XL, the products of STAT3 target genes.
Statistical Analyses
Statistical analysis of hematology and clinical chemistry was performed by using the program Minitab (Minitab, State College, PA, USA). Group comparisons were conducted by using analysis of variance (ANOVA) with pair-wise comparison by the Fisher exact test and, for nonparametric analysis, Kruskal-Wallis with pair-wise comparisons using the Mann-Whitney test. Significance was set at p ≤ 0.05. Comparisons of in vivo tumor volumes and STAT3 target gene expression were performed using a non-parametric, two-tailed Mann-Whitney test.
All supplementary materials are available online at https://doi.org/www.molmed.org .
Results
In Vivo Therapeutic Efficacy Study
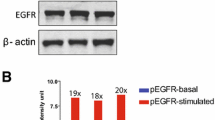
In initial studies, we evaluated the impact of cyclic STAT3 decoy or mutant cyclic STAT3 decoy on xenograft tumors derived from the HNSCC cell line UM-SCC1. The decoys were administered daily via intravenous delivery at either 5 or 10 mg/kg for a total of 2 wks. At the end of the treatment period, both the doses of the cyclic STAT3 decoy exhibited significant inhibition of tumor growth when compared with the mutant cyclic STAT3 decoy or saline. However, there were no significant differences in tumor volumes at the two different doses of the cyclic STAT3 decoy, demonstrating the absence of a dose-dependent effect at these concentrations (Figure 1A). To ascertain the impact of the systemically administered cyclic STAT3 decoy on the expression of STAT3 target genes, tumors were harvested after 15 d of treatment and the levels of cyclin D1 and Bcl-XL in the tumors were determined. Systemic administration of the cyclic STAT3 decoy at a dose of 10 mg/kg resulted in a significant decrease in cyclin D1/ β-tubulin ratio (p < 0.0001, p = 0.0078) and Bcl-XL/β-tubulin ratio (p = 0.001, p = 0.024) relative to treatment with saline and the mutant cyclic STAT3 decoy, which were used as controls (Figure 1B). Similarly, treatment with cyclic STAT3 decoy at a dose of 5 mg/kg, resulted in a significant decrease in cyclin D1/ β-tubulin ratio (p = 0.0004, p = 0.02) and Bcl-XL/β-tubulin ratio (p = 0.0003, p = 0.0002) relative to treatment with saline and the mutant cyclic STAT3 decoy (Figure 1C). Although there was a greater downreg-ulation of cyclin D1 expression levels in the 10 mg/kg STAT3 decoy group (65%) compared with the 5 mg/kg cyclic STAT3 decoy treated group (58%) compared with their respective mutant controls, these differences were not statistically significant. These results indicate that the cyclic STAT3 decoy exerts its antitumor effects by affecting STAT3 signaling. Unlike less selective chemotherapy agents or radiation, there was no evidence of a dose response of the cyclic STAT3 decoy, indicating that the decoy resembles biological compounds in that higher concentrations are not necessarily more effective.
Intravenous administration of cyclic STAT3 decoy suppressed xenograft tumor growth and downmodulated STAT3 target genes in the tumors of mice. (A) Mean tumor volume by day of treatment and treatment groups. UM-SCC1 cells (3 × 106 cells) were inoculated subcutaneously in the right flank of athymic nude mice. Mice were randomized after developing palpable tumors and were injected intravenously once a day, with 5 or 10 mg/kg of the cyclic STAT3 decoy or the mutant cyclic STAT3 decoy, or saline, for 2 wks (7 d/wk). Tumor volumes were measured three times a week using two-dimensional vernier calipers and measured to d 15. A significant decrease in tumor volume was observed in the mice treated with a cyclic STAT3 decoy (5 or 10 mg/kg) compared with the mutant cyclic STAT3 decoy group (p = 0.01) or saline (p = 0.01 for cyclic STAT3 decoy (5 mg/kg), p = 0.04 for cyclic STAT3 decoy (10 mg/kg)), as indicated by a nonparametric, two-tailed Mann-Whitney test. (B, C) At the end of the treatment period, the xenograft tumors were harvested and analyzed for STAT3 target gene expression, by performing immunoblotting for cyclin D1 and Bcl-XL. β-Tubulin was used to assess protein loading. In (B), the bar graph is a quantitative representation of cyclin D1/β-tubulin (p < 0.0001, p = 0.0078) and Bcl-XL/β-tubulin (p = 0.001, p = 0.024) in tumors from mice treated with cyclic STAT3 decoy (10 mg/kg) versus the saline or cyclic mutant control decoy (10 mg/kg), respectively. ln (C), the bar graph is a quantitative representation of cyclin D1/β-tubulin (p = 0.0004, p = 0.02) and Bcl-XL/β-tubulin (p = 0.0003, p = 0.0002) in tumors from mice treated with cyclic STAT3 decoy (5 mg/kg) versus the saline or cyclic mutant control decoy (5 mg/kg), respectively.
Clinical Observations and Body Weights
To determine potential toxicities of the cyclic STAT3 decoy, mice were treated for 2 wks (IV once daily, 5 d per wk) with saline control or with 100, 67 or 33 mg/kg of the cyclic decoy. The treatment groups administered the highest doses (100 and 67 mg/kg) were observed to be transiently hyperactive after dosing for the first 3 d. The 33 mg/kg cyclic STAT3 decoy treatment group also appeared to be hyperactive after d 8 of dosing. The vehicle treatment group did not experience hyperactivity. The two highest treatment groups remained hyperactive in the week of observation after dosing. During the dosing schedule, observations were made for clinical signs of toxicity, and none were noted. The relevance of the transient hyperactivity is unknown. Mice were monitored for changes in body weight, which would indicate possible toxic effects of the drug. The changes in percentage of body weight during the treatment are shown in Figure 2. There were no significant changes in body weights between the different treatment groups during the dosing period or after the dosing interval or on the day of euthanasia.
Body weights of mice during dosing and the 10-d observation period. Mice were followed for 10 d after dosing with cyclic STAT3 decoy at 100, 67 or 33 mg/kg or saline as a vehicle and were monitored for clinical signs of toxicity. The graph represents multiple-dose cyclic STAT3 decoy MTD mean body weights expressed as percentage of starting mean body weight.
Select Organ Weights and Body Weights at Euthanasia
No gross pathology of any organs was noted at necropsy in any of the animals. Moreover, there were no differences in mean and median body weights between the treatment groups at euthanasia. Weights for liver, kidneys, spleen, heart, thymus, lungs and brain were measured immediately after removal from the animal. There were no significant differences in mean or median tissue weights or the tissue weights based on percentage of body weight between treatment groups. Percentage of starting body weight on d 1 and throughout the course of the multiple-dose range-finding study are presented in Table 1, and the body weights and tissue weights at euthanasia are presented in Table 2.
Hematology and Clinical Chemistries
The mean ± standard deviation (SD) of the various hematology and clinical chemistry parameters are presented in Figures 3 and 4, and a significant difference from values obtained in the vehicle-treated mice (p ≤ 0.05) is indicated by an asterisk. The exact p values for the ANOVA with significant pair differences and for Kruskal-Wallis with significant pair differences using the MannWhitney test are presented in Table 3. There were no hematology results for one mouse (67 mg/kg cyclic STAT3 decoy treatment group) because the sample clotted before analysis. Although there were instances where one of the treatment groups was significantly different from the control group, there were no consistent trends in any of the hematology or clinical chemistry parameters, suggesting a lack of toxicity in the cyclic STAT3 decoy-treated mice compared with the saline-treated control group. Blood urea nitrogen concentrations were significantly lower in the 67 and 33 mg/kg groups compared with the control saline-treated groups (Figure 4J). Bicarbonate was higher in all treatment groups compared with the control group; however, only the values for the 100 and 33 mg/kg groups were significantly different than the saline-treated control group (Figure 4Q). In the case of anion gap, the values were lower in all the treatment groups compared with control; however, only the 100 mg/kg group and the 33 mg/kg group were significantly different when compared with the saline-treated control group (Figure 4R). The clinical significance of these parameter changes is unknown.
Cyclic STAT3 decoy administration effects on hematological parameters in mice. Panels A-L demonstrate distribution of hematological indices in the blood of mice injected with cyclic STAT3 decoy. Five mice were injected with cyclic STAT3 decoy at 100 mg/kg, five mice at 67 mg/kg, five mice at 33 mg/kg and five mice with saline as a vehicle, and blood was collected from each mouse by cardiac puncture. Data for each parameter for the groups are shown in the form of a bar graph as means ± SD.
Cyclic STAT3 decoy administration effects on and serum chemistry parameters in mice. Panels A-S demonstrate distribution of serum chemistries in the blood of mice injected with cyclic STAT3 decoy. Five mice were injected with cyclic STAT3 decoy at 100 mg/kg, five mice at 67 mg/kg, five mice at 33 mg/kg and five mice with saline as a vehicle, and blood was collected from each mouse by cardiac puncture. Data for each parameter for the groups are shown in the form of a bar graph as means ± SD.
Administration of Cyclic STAT3 Decoy Did Not Result in Organ Damage
Histopathological studies were performed on hematoxylin and eosin-stained paraffin sections of the following tissues: bone (femur), bone marrow (sternum, rib, costochondral junction), brain, cecum, colon, duodenum, esophagus, eyes, gall bladder, gonads, heart, ileum, jejunum, kidneys, liver, lungs, lymph nodes (bronchial, mandibular, mesenteric), pancreas, thyroid and parathyroid glands, salivary gland, sciatic nerve, skeletal muscle (biceps femoris), skin (ventral abdomen) and mammary gland, spinal cord (thoracolumbar), spleen, stomach (cardiac, fundic and pyloric), thymus, trachea, urinary bladder and uterus. The inflammatory changes in the endometrium of the uterus and lung were found in both control and cyclic STAT3 decoy treatment groups and therefore were likely unrelated to cyclic decoy treatment. Representative histological sections for vital organs such as bone marrow, brain, kidney, heart, liver and thymus demonstrated healthy tissues, thus suggesting that treatment with cyclic STAT3 decoy at 10 mg/kg did not have any effect (Supplementary Figure S1). The microscopic findings of other organs are also unremarkable, indicating that cyclic STAT3 decoy treatment did not cause histological changes in any organs (data not shown).
Discussion
STAT3 is persistently activated in many different cancers including solid and hematological malignancies (19). Approximately 95% of head and neck cancers overexpress STAT3 (19). Targeted deletion of STAT3 prevented epithelial cancers in skin cells (20), and the oncogenic role of STAT3 was shown by the ability of a constitutively active mutant to transform fibroblasts in vitro (7) and initiate tumor formation in vivo (21). Increased expression of activated STAT3 has been correlated with tumor stage and poor prognosis (7). These cumulative results point to STAT3 as a promising cancer therapeutic target. A double-stranded transcription factor decoy oligonucleotide was developed in our laboratory that inhibits STAT3-mediated DNA binding to the promoter region of STAT3 target genes and demonstrates antitumor efficacy in preclinical models of HNSCC and several other cancers (4,10). A toxicity study in cynomolgus monkeys administered a single intramuscular injection of this linear STAT3 decoy at a low-dose of 0.8 mg and a high dose of 3.2 mg. Neither dose resulted in the death of any animal and neither demonstrated signs of toxicity (4) when compared with the control group injected with saline (4). The linear STAT3 decoy was also administered to head and neck cancer patients in a placebo-controlled phase 0 clinical trial where there was demonstrable downregulation of target genes in tumor tissue but no evidence of toxicity (17). However, the linear decoy formulation is limited by the requirement for intratumoral administration.
Recent studies have evaluated the safety and efficacy of the oligonucleotide ISIS 481464 in preclinical and clinical studies. ISIS 481464 is and ethyl-modified phosphorothioate antisense oligonucleotide that targets STAT3 mRNA (16). Toxicology studies in mice and nonhuman primates have revealed that the toxicity profile of ISIS 481464 is consistent with the 2′MOE-modified version of the oligonucleotide and no new toxicities were detected (16). A phase I study of ISIS 481464 to establish the maximum tolerated dose (MTD) in addition to determining the safety, tumor response, pharmacokinetics (PK) and pharmacodynamics in patients with advanced cancers reported one dose-limiting toxicity at a dosage of 4 mg/kg. Additionally, three patients, one at 2 mg/kg and two at 4 mg/kg, experienced nadirs in platelet counts below 50 × 109/L (range 16–33 × 109/L), and MTD was not reached. There was a partial response in two out of three diffuse large B-cell lymphoma patients, and PK studies revealed increased plasma trough levels (indicative of tissue concentrations) with increased dose (22).
The use of a decoy oligonucleotide to target and inhibit activated STAT3 is particularly attractive because of the specificity and potency of the STAT3 decoy (7). Preclinical studies with the linear formulation of the STAT3 decoy have shown significant antitumor effects in vivo in HNSCC as well as in several other cancers (11,13,23,24). Moreover, a phase 0 clinical trial of the linear STAT3 decoy in HNSCC patients demonstrated pharmacodynamics effects of the decoy on STAT3 target gene expression in tumor tissues (17). However, these effects were elicited after in-tratumoral injection of the linear decoy. Preclinical studies have shown that intravenous administration of the linear STAT3 decoy molecule fails to inhibit xenograft tumor growth in nude mice, likely due to degradation of the decoy by serum nucleases (17). Thus, the weak stability of the linear STAT3 decoy has been a major impediment to the clinical development of this approach in HNSCC. To address this problem, we chemically modified the STAT3 decoy by linking the 5′ and 3′ ends of both the sense and antisense strand of the parent STAT3 decoy by using a hexaethylene glycol spacer to generate a cyclic molecule (17). The cyclic STAT3 decoy demonstrated increased thermal and serum stability and retained potency and binding affinity when compared with the linear STAT3 decoy. Importantly, intravenous administration of the cyclic STAT3 decoy inhibited the growth of HNSCC xenograft tumors (17).
The present study was undertaken to evaluate dose-dependent antitumor efficacies and potential toxicities of systemic delivery of the cyclic STAT3 decoy. Significant inhibition of tumor growth was observed with both the 5 and 10 mg/kg doses of the cyclic STAT3 decoy, although no dose-dependency was observed. During detailed examination, we found no evidence of systemic or organ-specific toxicity at the high concentrations administered. The clinical relevance of the transient hyperactivity observed in the STAT3 decoy-treated groups is unclear. We could find no reports in the literature of an anticancer agent inducing hyperactivity. In general, serum chemistries were no different in the cyclic STAT3 decoy-treated animals compared with controls. Blood urea nitrogen and anion gap levels were lower, and bicarbonate levels were higher in the cyclic STAT3 decoy-treated group compared with the saline control group, although the clinical significance of these findings is unknown. In the absence of a mouse model of head and neck cancer, we required athymic nude mice for the efficacy studies upon implantation of human cancer cells. We elected to use immunocompetent animals for the toxicity experiments to account for the contributions of the immune system. It is possible that the toxicity in tumor-bearing mice may be different because of the lack of immune system. However, our previous toxicology study of a singular intramuscular injection of the linear STAT3 decoy in cynomolgus monkeys also demonstrated no evidence of toxicity (4). This is the first in vivo study to demonstrate lack of toxicity of the chemically modified, cyclic STAT3 decoy given intravenously in mice.
Conclusion
Our results suggest that the cyclic STAT3 decoy is able to inhibit tumor volume in a head and neck squamous cell carcinoma xenograft model when injected intravenously both at 5 and 10 mg/kg; however, there is no dose-dependent effect. Further toxicity study with the cyclic STAT3 decoy demonstrated no significant changes in body weights, hematology or clinical chemistry parameters, or gross or histological pathological abnormalities during the dosing period, after the dosing interval or on the day of euthanasia. These results suggest lack of toxicity of intravenous administration of a cyclic STAT3 decoy oligonucleotide.
Disclosure
The authors declare that they have no competing interests as defined by Molecular Medicine, or other interests that might be perceived to influence the results and discussion reported in this paper.
References
Yu H, Pardoll D, Jove R. (2009) STATs in cancer inflammation and immunity: a leading role for STAT3. Nat. Rev. Cancer. 9:798–809.
Kawano M, et al. (1988) Autocrine generation and requirement of BSF-2/IL-6 for human multiple myelomas. Nature 332:83–85.
Catlett-Falcone R, et al. (1999) Constitutive activation of Stat3 signaling confers resistance to apoptosis in human U266 myeloma cells. Immunity. 10:105–15.
Sen M, et al. (2009) Lack of toxicity of a STAT3 decoy oligonucleotide. Cancer Chemother. Pharmacol. 63:983–95.
Deng J, Grande F, Neamati N. (2007) Small molecule inhibitors of Stat3 signaling pathway. Curr. Cancer Drug Targets. 7:91–107.
Koppikar P, Bromberg J. (2012) STATe-of-the-art approach: using oligonucleotide decoys to target the “undruggable.” Cancer Discov. 2:670–2.
Leeman RJ, Lui VW, Grandis JR. (2006) STAT3 as a therapeutic target in head and neck cancer. Expert Opin. Biol. Ther. 6:231–41.
Xu G, Zhang C, Zhang J. (2009) Dominant negative STAT3 suppresses the growth and invasion capability of human lung cancer cells. Mol. Med. Rep. 2:819–24.
Jing N, et al. (2003) Targeting Stat3 with G-quartet oligodeoxynucleotides in human cancer cells. DNA Cell Biol. 22:685–96.
Leong PL, et al. (2003) Targeted inhibition of Stat3 with a decoy oligonucleotide abrogates head and neck cancer cell growth. Proc. Natl. Acad. Sci. U. S. A. 100:4138–43.
Souissi I, et al. (2011) A STAT3-decoy oligonucleotide induces cell death in a human colorectal carcinoma cell line by blocking nuclear transfer of STAT3 and STAT3-bound NF-kappaB. BMC Cell Biol. 12:14.
Zhang X, Zhang J, Wei H, Tian Z. (2007) STAT3-decoy oligodeoxynucleotide inhibits the growth of human lung cancer via down-regulating its target genes. Oncol. Rep. 17:1377–82.
Shen J, Li R, Li G. (2009) Inhibitory effects of decoy-ODN targeting activated STAT3 on human glioma growth in vivo. In Vivo. 23:237–43.
Kong LY, et al. (2008) A novel inhibitor of signal transducers and activators of transcription 3 activation is efficacious against established central nervous system melanoma and inhibits regulatory T cells. Clin. Cancer Res. 14:5759–68.
Uckun FM, Ek O, Liu XP, Chen CL. (1999) In vivo toxicity and pharmacokinetic features of the janus kinase 3 inhibitor WHI-P131 [4-(4′hydroxyphenyl)-amino-6,7-dimethoxyquinazoline]. Clin. Cancer Res. 5:2954–62.
Burel SA, et al. (2013) Preclinical evaluation of the toxicological effects of a novel constrained ethyl modified antisense compound targeting signal transducer and activator of transcription 3 in mice and cynomolgus monkeys. Nucleic Acid Ther. 23:213–27.
Sen M, et al. (2012) First-in-human trial of a STAT3 decoy oligonucleotide in head and neck tumors: implications for cancer therapy. Cancer Discov. 2:694–705.
Committee for the Update of the Guide for the Care and Use of Laboratory Animals, Institute for Laboratory Animal Research, Division on Earth and Life Studies, National Research Council of the National Academies. (2011) Guide for the Care and Use of Laboratory Animals. 8th edition. Washington (DC): National Academies Press. [cited 20XX Month Day]. Available from: https://doi.org/oacu.od.nih.gov/regs/.
Darnell JE. (2005) Validating Stat3 in cancer therapy. Nat. Med. 11:595–6.
Chan KS, et al. (2004) Disruption of Stat3 reveals a critical role in both the initiation and the promotion stages of epithelial carcinogenesis. J. Clin. Invest. 114:720–8.
Demaria M, et al. (2012) STAT3 can serve as a hit in the process of malignant transformation of primary cells. Cell Death Differ. 19:1390–7.
Hong DS, et al. (2013) A phase I study of ISIS 481464 (AZD9150), a first-in-human, first-in-class, antisense oligonucleotide inhibitor of STAT3, in patients with advanced cancers [abstract]. J. Clin. Oncol. 31(15 Suppl). Abstr. No. 8523.
Zhang X, Zhang J, Wang L, Wei H, Tian Z. (2007) Therapeutic effects of STAT3 decoy oligodeoxynu-cleotide on human lung cancer in xenograft mice. BMC Cancer. 7:149.
Sun Z, Yao Z, Liu S, Tang H, Yan X. (2006) An oligonucleotide decoy for Stat3 activates the immune response of macrophages to breast cancer. Immunobiology. 211:199–209.
Acknowledgments
This work was supported by National Institutes of Health Grants P50CA097190 and R01CA77308 and the American Cancer Society. Research support was provided by Johnson & Johnson and the Cancer Center Core Grant P30CA47904.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, and provide a link to the Creative Commons license. You do not have permission under this license to share adapted material derived from this article or parts of it.
The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this license, visit (https://doi.org/creativecommons.org/licenses/by-nc-nd/4.0/)
About this article
Cite this article
Sen, M., Paul, K., Freilino, M.L. et al. Systemic Administration of a Cyclic Signal Transducer and Activator of Transcription 3 (STAT3) Decoy Oligonucleotide Inhibits Tumor Growth without Inducing Toxicological Effects. Mol Med 20, 46–56 (2014). https://doi.org/10.2119/molmed.2013.00104
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.2119/molmed.2013.00104