Abstract
We compared the lipid profiles and serum levels of leptin, adiponectin and tumor necrosis factor-α (TNF-α) in rats with/without hyperlipidemia and with/without concomitant diabetes mellitus. Forty 10-wk-old male Wistar rats were divided into four groups. Groups A and C received standard food for 12 wks. Groups B and D received a high-fat diet enriched with 2% additional cholesterol. Moreover, insulin-deficient (type I) diabetes mellitus was induced in rats in groups C and D with intraperitoneal injections of streptozotocin. Fasting serum leptin levels were decreased in diabetic groups (groups C and D) compared with controls. Fasting serum adiponectin levels were decreased in groups C and D compared with group A. Serum TNF-α levels were augmented in groups B and D, those fed with an atherogenic diet. By contrast, TNF-α levels were decreased in group C. Our data suggest that serum leptin, adiponectin and TNF-α levels may serve as markers of obesity and type I diabetes mellitus.
Similar content being viewed by others
Introduction
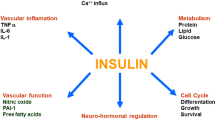
Type I diabetes mellitus (DM I) and obesity have received increasing attention because of the rising epidemic in the population. Adipose tissue regulates energy balance and glucose and lipid metabolism via the secretion of adipocytokines. Leptin, adiponectin and tumor necrosis factor-α (TNF-α) levels are different in diabetic and obese individuals compared with nondiabetic, nonobese individuals. Morbid rates of leptin and adiponectin may provide a link between obesity, diabetes and increased cardiovascular risk. The protein leptin, a satiety hormone, regulates appetite, energy homeostasis and glucose/lipid metabolism (1–5). Adiponectin exerts profound antidiabetic, antiatherogenic and antiinflammatory roles (2,6–8). Both hormones improve insulin resistance (9), although their blood concentrations may be contradictory, depending on adipocyte deposition (10). Plasma leptin levels correlate with body fat content (1–3,11); the increase of fat cells in number and in size is coupled with an increase in leptin secretion (11–13). Obesity is characterized by hyperleptinemia (11,13,14), whereas leptin levels decrease considerably during weight loss (15). Although plasma leptin levels are elevated in obesity and type II diabetes mellitus (DM II), they are decreased in DM I and are positively associated with body mass index (BMI) (16,17). Adiponectin levels are increased in DM I (18,19) and decreased in DM II (20–22). Obesity is also characterized by hypoad-iponectinemia, because adiponectin is inversely correlated with BMI (6,8–10,19). TNF-α, a cytokine secreted by adipocytes, influences energy balance and glucose homeostasis. TNF-α causes insulin resistance and plays a major role in the pathogenesis of obesity-linked DM II (23,24). TNF-α levels are increased in DM I; TNF-α is involved in the autoimmunity process leading to pancreatic β-cell damage and the induction of DM I (25,26). It has been suggested that TNF-α may be an indicator for the quality of metabolic control in DM I (26). Furthermore, TNF-α levels are also increased in obesity (27).
In the present study we compared serum levels of leptin, adiponectin and TNF-α in diabetic rats subjected to different dietary manipulations, and investigated the complex interrelations between adipocytokines, hyperglycemia and hyperlipidemia.
Materials and Methods
Animal Preparation and Induction of Diabetes
The experiments were carried out on 40 male 10-wk-old Wistar rats weighing 220–300 g each. The rats were housed in plastic cages according to European standards (Tecniplast, Buguggiate, Italy) in the Laboratory for Experimental Surgery and Surgical Research, in a controlled environment at 20°C ± 2°C, with 55% relative humidity, central ventilation (15 air changes/h) and an artificial 12-h light-dark cycle. All animal experiments were carried out in compliance with the Guide for the Care and Use of Laboratory Animals published by the National Academy of Sciences. The protocol was approved by the Institutional Animal Care and Use Committee of the University of Athens Medical School and Veterinary Directorate of the Athens Prefecture (permit number K/2927). After acclimatization for 1 wk, the animals were randomly divided into four groups (A–D) of 8–12 rats each. Access to food and water was unrestricted for all groups.
Group A (control group) and group C received a standard rat diet, and groups B and D received a high-fat diet. The composition of the control diet was protein 20%, carbohydrates 40%, fat 5%, fiber 3% and other constituents 32%. The composition of the high-fat diet was enriched with 2% cholesterol. In groups C and D, insulin-deficient DM I was induced by intraperitoneal injections of freshly prepared streptozotocin (catalog number S0130/Lot #119K159; Sigma, St. Louis, MO, USA) at a dose of 50 mg/dL/kg in ice-cold 0.5 mol/L citrate buffer (pH 4.5). The body weight and food and water consumption of the animals were measured daily.
Animal Measurements
During the study period, blood samples were collected at the beginning and after 4, 8, 10 and 12 wks for serum lipid, glucose and hormonal measurements. Using capillary tubes, we collected blood from the retroorbital plexus of the rats, which were under light ether anesthesia. The blood samples were then placed into Eppendorf tubes containing heparin. The blood samples were collected at the same time of the day for every measurement. Food was withdrawn 10 h before blood collection. All animals were killed by exsanguination 12 wks after initiation of the study. Blood was drawn from the inferior vena cava while the rats were under deep ether anesthesia. The plasma was separated by centrifugation (15 min at 3000g) and the serum aliquots were stored at −80°C until analyzed.
Diabetic Status
The diagnosis of diabetes was determined on the basis of a full clinical examination and serum tests. Fasting plasma glucose levels were measured by using the hexokinase/glucose-6-phosphate dehydrogenase method (28). Serum insulin levels were measured by a radio-immunoassay kit using rat insulin as a standard. The homeostasis model assessment for insulin resistance (HOMA-R) was calculated as an indicator of insulin resistance, according to the formula HOMA-R = fasting glucose (mmol/L) × fasting insulin (µU/mL)/22.5.
Serum Lipid Measurement
High-density lipoprotein cholesterol (HDL-C) was isolated by precipitating chylomicrons, and very low-density lipoprotein cholesterol and low-density lipoprotein cholesterol (LDL-C) by adding phosphotungstic acid and magnesium ions to the samples. Serum cholesterol and HDL-C were determined en-zymatically by the cholesterol oxidase peroxidase-amidopyrine method using a commercially available kit (Biosis, Athens, Greece). Serum triglycerides were measured by the enzymatic glycerol-3-phosphate-oxidase peroxidase-amidopyrine method using a commercially available kit (Biosis). LDL-C was estimated by use of the Friedewald formula: LDL = total cholesterol level — HDL — [triglyceride level/5].
Hormone Measurement
Serum leptin, adiponectin and TNF-α levels were measured by use of various commercially available rat enzyme-linked immunosorbent assay (ELISA) kits. Specifically, for leptin levels measurements the R&D Systems ELISA kit was used (catalog number MOB00; R&D Systems, Minneapolis, MN, USA), for serum adiponectin levels the Alpco ELISA kit (catalog number 44-ADPRT-E01; Alpco, Salem, NH, USA) and for TNF-α levels the Invitrogen ELISA kit (catalog number KRC3014; Invitrogen, Carlsbad, CA, USA). Fasting serum insulin levels were measured by the Mercodia ELISA kit (catalog number 10-1124-01; Mercodia, Uppsala, Sweden).
Statistical Analyses
Data are expressed as mean ± standard deviation for continuous variables and as percentages for categorical data. The Shapiro-Wilk test was used to assess whether the distribution of variables followed the normal distribution. Comparisons of continuous variables were analyzed by using the Mann-Whitney nonparametric test as appropriate, and categorical variables were assessed by using the Spearman χ2 test. Linear relationships between quantitative variables were assessed with the Spearman rho for nonparametric data. Multivariate analysis of variance as well as analysis of covariance were performed to analyze the effects of each measured variable, not only within the groups but also between different groups (primary assumption: covariates such as age, sex and weight were already normalized, owing to the fact that the rats used in the experiment were set as equal from the start). All statistical tests were examined at a 5% level of significance. In other words, null hypothesis was rejected with >95% confidence (confidence interval two-tailed P < 0.5).
Results
Determination of Diabetes
Animals injected with streptozotocin became markedly diabetic, as manifested by fasting serum glucose levels (Tables 1 and 2). Baseline values of glucose were similar in all groups. Two rats in group D died on d 2 and d 3, respectively, after streptozotocin injection. The diabetic animals presented with increased polyuria, polyphagia and polydipsia compared with the control group. Fasting serum glucose levels were significantly higher in groups C and D compared with the control groups (Tables 2 and 3) (group A, 153.00 ± 14.4 mg/dL; group B, 114.00 ± 35.7 mg/dL; group C, 255.30 ± 129.9 mg/dL; group D, 244.50 ± 209.9 mg/dL; P < 0.01). There was no significant difference in insulin and HOMA-R levels among the groups.
Lipid Profile
Total cholesterol in group D was increased compared with the control group (Tables 2 and 3) (group A, 67.25 ± 12.2 mg/dL; group B, 76.00 ± 7.6 mg/dL; group C, 67.25 ± 18.8 mg/dL; group D, 129.66 ± 157.3 mg/dL; P < 0.05). Total cholesterol levels varied between the diabetic groups (group C versus group D; P < 0.01) (Table 4). Triglyceride levels did not vary among the groups (Tables 3 and 4). LDL-C levels were increased in group D compared with controls (group A, 22.65 ± 12.8 mg/dL; group C, 14.63 ± 9.4 mg/dL; group D, 105.90 ± 143.6 mg/dL; P < 0.05). LDL-C levels also varied among the diabetic groups (group C versus group D; P < 0.05). HDL-C levels were decreased in group B compared with controls (Tables 2 and 3), whereas there was no significant difference among the diabetic groups (Table 4) (group A, 25.50 ± 4.8 mg/dL; group B, 20.30 ± 5.2 mg/dL; group C, 28.50 ± 8.1 mg/dL; group D, 22.91 ± 14.7 mg/dL; P < 0.01).
Hormonal Profile
Baseline values of leptin, adiponectin and TNF-α levels were similar among all groups. Fasting serum leptin levels were significantly decreased in diabetic groups C and D compared with controls (Tables 1–3) (group A, 242.80 ± 104.5 pg/mL; group C, 124.56 ± 115.5 pg/mL; group D, 89.24 ± 72.88 pg/mL; P < 0.05). Leptin levels did not vary between the diabetic groups (C versus D) (Table 4).
Fasting serum adiponectin levels were decreased in groups C and D compared with group A (Tables 2 and 3) (group A, 109.15 ± 95.4 ng/mL; group B, 10.64 ± 7.1 ng/mL; group C, 16.90 ± 10.4 ng/mL; group D, 17.29 ± 15.07 ng/mL; P < 0.01). Adiponectin levels were also decreased in group B compared with group A (P < 0.001) (Table 3). No difference in adiponectin levels was found between groups C and D (Table 4). Leptin levels were correlated to fasting insulin (r = 0.420, P < 0.05) and glucose (r = −0.415, P < 0.05). Adiponectin was correlated to glucose (r = −0.359, P < 0.05) and leptin (r = 0.530, P < 0.01).
Serum TNF-α levels were increased in groups B and D fed with an atherogenic diet compared with group A (Tables 2 and 3) (group A, 2.02 ± 0.7 pg/mL; group B, 20.51 ± 18.4 pg/mL; group D, 10.52 ± 19.7 pg/mL; P < 0.05). In contrast, TNF-α levels were decreased in group C compared with group B and D (P < 0.005) (Table 4). TNF-α was correlated to total cholesterol (r = 0.754, P < 0.005) and HDL-C (r = 0.823, P < 0.001).
Discussion
Our study results demonstrated that serum leptin, adiponectin and TNF-α levels were altered after the induction of DM I and/or hyperlipidemia.
Diabetes induced by high-dose streptozotocin resembles human DM I, with reduced leptin secretion due to decreased insulin-mediated glucose metabolism in adipose tissue (29). Serum leptin levels were decreased in diabetic rats compared with their nondiabetic counterparts. This finding is in agreement with previous studies showing that leptin levels decrease in DM I (16). It was hypothesized almost a decade ago that the reduced leptin levels in DM I patients are associated with the insulin deficiency observed in these patients (30). A recent study on nonobese DM I mice revealed that recombinant leptin treatment, either alone or in combination with low-dose insulin therapy, provided equivalent or superior glycemic stability without the increase in body fat and upregulation of cholesterologenic and lipogenic transcription factors and enzymes observed with insulin monotherapy (30). Recombinant leptin treatment profoundly reduced food intake, body weight and body fat (30). The antidiabetic effects of leptin may be mediated by glucagon suppression (30,31). Verification of these results in humans holds implications for future use of leptin as an antidiabetic agent. Thus, like insulin, leptin is a potent suppressor of glucagon and may be used both as a marker of diabetic status as well as a potential therapeutic tool for the management of DM I.
Adiponectin is a possible insulinsensitizing agent (5,6,20–22). Serum adiponectin levels are negatively associated with the BMI in healthy individuals and are decreased in DM II (6,20,21). By contrast, adiponectin levels are increased in patients with DM I (32). An immune mechanism has been proposed to account for this increase (32). We found decreased adiponectin levels in hyperlipidemic rats alone and in DM I rats alone, as well as in rats having both DM I and hyperlipidemia. The reason may be the lack of an immune mechanism that leads to β-cell damage and absolute insulin deficiency in our model of streptozotocin-induced diabetes. It was recently suggested that the high-molecular weight form of adiponectin may serve as a significant surrogate marker for the prediction of DM II in the Japanese population (33). In an earlier report, investigators postulated that decreased total and high-molecular weight adiponectin levels are independent risk factors for the development of DM II in Japanese-Americans (34). Finally, the high-molecular weight multimeric form of adiponectin may serve as a useful marker to evaluate insulin resistance and the metabolic syndrome in men (6,35). Thus, there is already preliminary evidence suggesting that adiponectin may serve as an early marker of DM.
In addition to being an early marker of the metabolic syndrome, insulin resistance and DM II (33–35), low plasma adiponectin levels are also a marker of subclinical atherosclerosis. In a study performed 8 years ago, circulating adiponectin levels were demonstrated to correlate with the presence of early atherosclerosis, as measured by an increased intima media thickness in the carotid artery bulb (36). These results were verified a few years later (37). Plasma adiponectin levels were shown to be a marker of glucose metabolism and obesity, as well as carotid intima media thickness in a large study (n = 887) of middle-aged individuals (37). Finally, a recent study confirmed that serum adiponectin levels are associated with indices of subclinical atherosclerosis (such as intima media thickness and arterial compliance) in obese patients (38).
TNF-α levels are increased in both DM (33,34) and obesity (35). We also found increased TNF-α levels in animals receiving a high-fat diet. It is well known and firmly established that TNF-α levels serve as markers of both obesity and cachexia (23,24,39). In the absence of a high-fat diet, TNF-α levels were low and similar to the control group despite the induction of DM I. Again, the reason for this variation may be the lack of similarities at the molecular level between DM I and the streptozotocin-induced diabetes in our model. This finding is in contrast with studies performed on humans with DM I more than 10 years ago, which showed that in patients with DM I, TNF-α levels were elevated compared with nondiabetic individuals and correlated with the quality of glycemic control (40,41).
In our study, although animals fed with a high-fat diet presented with hypercholesterolemia, no difference was observed in leptin and adiponectin levels among diabetic groups with different lipid profiles. This finding is in agreement with the weak correlation between these hormones and levels of total cholesterol. In contrast, TNF-α levels were significantly different between diabetic groups with different lipid profiles. The reason may be the strong correlation between total cholesterol and TNF-α levels. This acute increase of TNF-α levels in subclinical dyslipidemia suggests that TNF-α levels are useful indicators of inflammation and a tool to optimize therapeutic management and reduce diabetic complications.
Adipocytokines have clinical implications as useful markers and potential therapeutic targets of glucose, lipid and cardiovascular abnormalities in all age groups. Serum leptin, adiponectin and TNF-α levels may accurately predict the presence of hyperlipidemia and/or DM in an animal model. We formulated the hypothesis, elaborated in previous studies, that these molecules may serve as prognostic indices in cases of subclinical dyslipidemia/DM I. This theory, however, must be confirmed in human studies before any definitive conclusions can be drawn.
Disclosure
The authors declare that they have no competing interests as defined by Molecular Medicine, or other interests that might be perceived to influence the results and discussion reported in this paper.
References
Havel PJ. (2002) Control of energy homeostasis and insulin action by adipocyte hormones: leptin, acylation stimulating protein, and adiponectin. Curr. Opin. Lipidol 13:51–9.
Meier U, Gressner AM. (2004) Endocrine regulation of energy metabolism: review of pathobiochemical and clinical chemical aspects of leptin, ghrelin, adiponectin, and resistin. Clin. Chem. 50:1511–25.
Havel PJ. (2004) Update on adipocyte hormones: regulation of energy balance and carbohydrate/lipid metabolism. Diabetes. 53(Suppl 1):S143–51.
Ahima RS. (2006) Adipose tissue as an endocrine organ. Obesity. 14(Suppl 5):242S–9S.
Ahima RS. (2006) Metabolic actions of adipocyte hormones: focus on adiponectin. Obesity. 14(Suppl 1):9S–15S.
Kadowaki T, et al. (2006) Adiponectin and adiponectin receptors in insulin resistance, diabetes, and the metabolic syndrome. J. Clin. Invest. 116:1784–92.
Gannagé-Yared MH, et al. (2006) Serum adiponectin and leptin levels in relation to the metabolic syndrome, androgenic profile and somatotropic axis in healthy non-diabetic elderly men. Eur. J. Endocrinol. 155:167–76.
Yan E, et al. (2008) Insulin, hs-CRP, leptin, and adiponectin. An analysis of their relationship to the metabolic syndrome in an obese population with an elevated waist circumference. Metab. Syndr. Relat. Disord. 6:64–73.
Silha JV, et al. (2003) Plasma resistin, adiponectin and leptin levels in lean and obese subjects: correlations with insulin resistance. Eur. J. Endocrinol. 149:331–5.
Oda N, et al. (2008) The ratio of leptin to adiponectin can be used as an index of insulin resistance. Metabolism. 57:268–73.
Considine RV, et al. (1996) Serum immunoreactive-leptin concentrations in normal-weight and obese humans. N. Engl. J. Med. 334:292–5.
Maffei M, et al. (1995) Leptin levels in human and rodent: measurement of plasma leptin and ob RNA in obese and weight-reduced subjects. Nat. Med. 1:1155–61.
Drevon CA. (2005) Fatty acids and expression of adipokines. Biochim. Biophys. Acta. 1740:287–92.
Ravussin E, Smith SR. (2002) Increased fat intake, impaired fat oxidation, and failure of fat cell proliferation result in ectopic fat storage, insulin resistance, and type 2 diabetes mellitus. Ann. N. Y. Acad. Sci. 967:363–78.
Anderlová K, et al. (2006) The influence of very-low-calorie-diet on serum leptin, soluble leptin receptor, adiponectin and resistin levels in obese women. Physiol. Res. 55:277–83.
Kiess W, et al. (1998) Serum leptin levels in children and adolescents with insulin-dependent diabetes mellitus in relation to metabolic control and body mass index. Eur. J. Endocrinol. 138:501–9.
Reinehr T, Kratzsch J, Kiess W, Andler W. (2005) Circulating soluble leptin receptor, leptin, and insulin resistance before and after weight loss in obese children. Int. J. Obes. (Lond) 29:1230–5.
Leth H, et al. (2008) Elevated levels of high-molecular-weight adiponectin in type 1 diabetes. J. Clin. Endocrinol. Metab. 93:3186–91.
Galler A, et al. (2007) Elevated serum levels of adiponectin in children, adolescents and young adults with type 1 diabetes and the impact of age, gender, body mass index and metabolic control: a longitudinal study. Eur. J. Endocrinol. 157:481–9.
Hotta K, et al. (2000) Plasma concentrations of a novel, adipose-specific protein, adiponectin, in type 2 diabetic patients. Arterioscler. Thromb. Vasc. Biol. 20:1595–9.
Weyer C, et al. (2001) Hypoadiponectinemia in obesity and type 2 diabetes: close association with insulin resistance and hyperinsulinemia. J. Clin. Endocrinol. Metab. 86:1930–5.
Yamauchi T, et al. (2001) The fat-derived hormone adiponectin reverses insulin resistance associated with both lipoatrophy and obesity. Nat. Med. 7:941–6.
Argiles JM, Lopez-Soriano J, Busquets S, Lopez-Soriano FJ. (1997) Journey from cachexia to obesity by TNF. FASEB J. 11:743–51.
Warne JP. (2003) Tumour necrosis factor alpha: a key regulator of adipose tissue mass. J. Endocrinol. 177:351–5.
Feugeas JP, et al. (1997) Influence of metabolic and genetic factors on tumour necrosis factor-alpha and lymphotoxin-alpha production in insulin-dependent diabetes mellitus. Diabetes Metab. 23:295–301.
Lechleitner M, Koch T, Herold M, Hoppichler F. (1999) Relationship of tumor necrosis factor-alpha plasma levels to metabolic control in type 1 diabetes. Diabetes Care. 22:1749.
Spiegelman BM, Hotamisligil GS. (1993) Through thick and thin: wasting, obesity, and TNF alpha. Cell. 73:625–7.
Neeley WE. (1972) Simple automated determination of serum or plasma glucose by a hexokinaseglucose-6-phosphate dehydrogenase method. Clin. Chem. 18:509–15.
Havel PJ, et al. (2000) Effects of streptozotocin-induced diabetes and insulin treatment on the hypothalamic melanocortin system and muscle uncoupling protein 3 expression in rats. Diabetes. 49:244–52.
Wang MY, et al. (2010) Leptin therapy in insulin-deficient type I diabetes. Proc. Natl. Acad. Sci. U. S. A. 107:4813–9.
Tudurí E, et al. (2009) Inhibitory effects of leptin on pancreatic alpha-cell function. Diabetes. 58:1616–24.
Imagawa A, et al. (2002) Elevated serum concentration of adipose-derived factor, adiponectin, in patients with type 1 diabetes. Diabetes Care. 25:1665–6.
Satoh H, Fujii S, Tsutsui H. (2010) The high-molecular weight (HMW) form of adiponectin is a significant surrogate marker for the prediction of type 2 diabetes mellitus in the Japanese population. Nutr. Metab. Cardiovasc. Dis. 20:e9–10.
Nakashima R, et al. (2006) Decreased total and high molecular weight adiponectin are independent risk factors for the development of type 2 diabetes in Japanese-Americans. J. Clin. Endocrinol. Metab. 91:3873–7.
Seino Y, Hirose H, Saito I, Itoh H. (2007) High molecular weight multimer form of adiponectin as a useful marker to evaluate insulin resistance and metabolic syndrome in Japanese men. Metabolism. 56:1493–9.
Jansson PA, et al. (2003) A novel cellular marker of insulin resistance and early atherosclerosis in humans is related to impaired fat cell differentiation and low adiponectin. FASEB J. 17:1434–40.
Nilsson PM, et al. (2006) Plasma adiponectin levels in relation to carotid intima media thickness and markers of insulin resistance. Arterioscler. Thromb. Vasc. Biol. 26:2758–62.
Shargorodsky M, et al. (2009) Adiponectin and vascular properties in obese patients: is it a novel biomarker of early atherosclerosis? Int. J. Obes. (Lond). 33:553–8.
Rydén M, Arner P. (2007) Tumour necrosis factor-alpha in human adipose tissue-from signalling mechanisms to clinical implications. J. Intern. Med. 262:431–8.
Lechleitner M, Koch T, Herold M, Dzien A, Hoppichler F. (2000) Tumour necrosis factor-alpha plasma level in patients with type 1 diabetes mellitus and its association with glycaemic control and cardiovascular risk factors. J. Intern. Med. 248:67–76.
Foss MC, Foss NT, Paccola GM, Silva CL. (1992) Serum levels of tumor necrosis factor in insulin-dependent diabetic patients. Braz. J. Med. Biol. Res. 25:239–42.
Acknowledgments
This project was partially supported by the Special Account for Research Grants of the University of Athens (“Kapodistrias” Program). We thank I Habeos for helpful comments and suggestions.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Margoni, A., Perrea, D.N., Vlachos, I. et al. Serum Leptin, Adiponectin and Tumor Necrosis Factor-α in Hyperlipidemic Rats with/without Concomitant Diabetes Mellitus. Mol Med 17, 36–40 (2011). https://doi.org/10.2119/molmed.2010.00167
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.2119/molmed.2010.00167