Abstract
Objectives
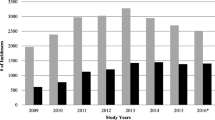
Increases of mild traumatic brain injuries in children have been reported in the USA and Ontario over the past decade. The main objective of this study is to calculate the pediatric rates of mild traumatic brain injury in Quebec, and our second objective is to compare them with those in Ontario.
Methods
Analysts from the Régie de l’Assurance Maladie du Québec (RAMQ, Quebec Health Insurance Board) compiled tables, by age and sex, of all medical services for mild traumatic brain injuries (concussions and minor head injuries) between 2003 and 2016. Quebec’s population rates were calculated and yearly graphs were plotted by age and sex.
Results
In Quebec, there were statistically significant increases in rates of mild traumatic brain injury (concussion and minor head injury) in older children: a 2.0-fold increase for those aged 13–17 years, and 1.4-fold increase for those aged 9–12 years. When only considering concussions, girls (13–17 years) had more concussions than boys in 2015 and 2016. The increase in the rates of concussion was significantly higher in Ontario than in Quebec: 4.4- vs. 2.2-fold increase.
Conclusions
The recent increase in rates of mild traumatic brain injuries reported in the scientific literature has also been observed in Quebec. The fact that the rate of visits for mild traumatic brain injury, per person, remained the same from 2003 to 2016 suggests that the increase was not the result of parents seeking more medical services, but that more of them consulted when their child injured his/her head.
Résumé
Objectifs
Des augmentations de taux de traumatismes crâniens (commotions et traumatismes crâniens mineurs) chez les enfants, ont été rapportés aux États-Unis et en Ontario au cours de la dernière décennie. L’objectif principal de cette étude est de calculer les taux de traumatismes crâniens au Québec et comme second objectif, les comparer avec ceux de l’Ontario.
Méthode
Les analystes de La Régie de l’Assurance Maladie du Québec ont compilé des tableaux, par groupe d’âge et sexe, de tous les actes médicaux pour un traumatisme crânien, entre 2003 et 2016. Les taux populationnels du Québec ont été calculés par âge et sexe, et présentés sous formes de graphiques.
Résultats
Au Québec, il y a eu des augmentations significatives dans les taux de traumatismes crâniens (commotion et traumatisme crânien mineur) chez les enfants de plus de 13 ans : augmentation de 2,0 fois plus chez les 13-17 ans, et de 1,4 chez les 9-12 ans. Depuis 2015 les filles (13-17 ans) ont eu plus de commotions cérébrales que les garçons. L’augmentation des taux de commotions cérébrales fut significativement plus élevée en Ontario qu’au Québec: 4,4 contre 2,2.
Conclusions
Comme aux États Unis et en Ontario, les taux de traumatismes crâniens ont aussi augmenté au Québec au cours des dernières années. Le fait que le taux de visites pour traumatismes crâniens, par personne, soit demeuré le même de 2003 à 2016, suggère que l’augmentation ne résulte pas d’une augmentation dans les services, mais que plus de parents consultent lorsque leur enfant se blesse à la tête.








Similar content being viewed by others
Notes
As calculated by RAMQ analysts.
Statistics from The Montreal Children’s Hospital Trauma Centre
References
Bakhos, L. L., Lockhart, G. R., Myers, R., & Linakis, J. G. (2010). Emergency department visits for concussion in young child athletes. Pediatrics, 126(3), e550–e556.
Birchard, M. (2014). Concussion legislation and education. Mouri Journal of Health, Physical Education, Recreation and Dance, 74.
Blue Cross Shields (2016). The steep rise in concussion diagnosis in the U.S. Available from: https://tinyurl.com/ydbx4tpl.
Brazinova, A., Rehorcikova, V., Taylor, M. S., Buckova, V., Majdan, M., Psota, M., et al. (2016). Epidemiology of traumatic brain injury in Europe: a living systematic review. Journal of Neurotrauma.
Caron, J. G., Bloom, G. A., Falcão, W. R., & Sweet, S. N. (2015). An examination of concussion education programmes: a scoping review methodology. Injury Prevention, 21(5), 301–308.
Carroll, L., Cassidy, J. D., Peloso, P., Borg, J., Von Holst, H., Holm, L., et al. (2004). Prognosis for mild traumatic brain injury: results of the WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. J Rehabil Med, 36(0), 84–105.
Centers for Disease Control and Prevention. (2013). CDC grand rounds: reducing severe traumatic brain injury in the United States. MMWR Morb Mortal Wkly Rep, 62(27), 549–552.
Centers for Disease Control and Prevention (2014a). Traumatic brain injury & concussion. Available from: https://tinyurl.com/ybrrunav.
Centers for Disease Control and Prevention (2014b). Traumatic brain injury in the United States: fact sheet. Available from: https://tinyurl.com/ybrrunav.
Chan, V., Thurairajah, P., & Colantonio, A. (2015). Defining pediatric traumatic brain injury using international classification of diseases version 10 codes: a systematic review. BMC Neurol, 15(1), 7.
Colvin, J. D., Thurm, C., Pate, B. M., Newland, J. G., Hall, M., & Meehan 3rd., W. P. (2013). Diagnosis and acute management of patients with concussion at children’s hospitals. Arch Dis Child, 98(12), 934–938.
Coronado, V. G., Haileyesus, T., Cheng, T. A., Bell, J. M., Haarbauer-Krupa, J., Lionbarger, M. R., et al. (2015). Trends in sports-and recreation-related traumatic brain injuries treated in US emergency departments: the National Electronic Injury Surveillance System-All Injury Program (NEISS-AIP) 2001-2012. J Head Trauma Rehabil, 30(3), 185–197.
Fainaru-Wada, M., Fainaru, S. (2013). League of denial: The NFL, concussions, and the battle for truth: Three Rivers Press.
Gardner, R. C., & Yaffe, K. (2015). Epidemiology of mild traumatic brain injury and neurodegenerative disease. Mol Cell Neurosci, 66(Pt B), 75–80.
Greenhow, A., & East, J. (2015). Custodians of the game: ethical considerations for football governing bodies in regulating concussion management. Neuroethics, 8(1), 65–82.
Harmon, K. G., Drezner, J. A., Gammons, M., Guskiewicz, K. M., Halstead, M., Herring, S. A., et al. (2013). American Medical Society for Sports Medicine position statement: concussion in sport. Br J Sports Med, 47(1), 15–26.
Institut de la Statistque du Quebec (2017). Québec population estimate, by age and sex, 2001–2016. Gouverneent du Quebec; Available from: https://tinyurl.com/y8y7z8k9
Keays, G., & Pless, I. B. (2010). Impact of a celebrity death on children’s injury-related emergency room visits. Can J Public Health, 101(2), 115–118.
Kostylova, A., Swaine, B., & Feldman, D. (2005). Concordance between childhood injury diagnoses from two sources: an injury surveillance system and a physician billing claims database. Injury Prevention., 11(3), 186–190.
Kristman, V. L., Borg, J., Godbolt, A. K., Salmi, L. R., Cancelliere, C., Carroll, L. J., et al. (2014). Methodological issues and research recommendations for prognosis after mild traumatic brain injury: results of the International Collaboration on Mild Traumatic Brain Injury Prognosis. Arch Phys Med Rehabil, 95(3), S265–SS77.
LaRoche, A. A., Nelson, L. D., Connelly, P. K., Walter, K. D., & McCrea, M. A. (2016). Sport-related concussion reporting and state legislative effects. Clinical journal of sport medicine: official journal of the Canadian Academy of Sport Medicine, 26(1), 33.
Lowrey, K. M., & Morain, S. R. (2014). State experiences implementing youth sports concussion laws: challenges, successes, and lessons for evaluating impact. The Journal of Law, Medicine & Ethics, 42(3), 290–296.
Mackenzie, S. G., & Pless, I. B. (1999). CHIRPP: Canada’s principal injury surveillance program. Injury Prevention, 5(3), 208–213.
Mannix, R., Meehan, W. P. III, Pascual-Leone, A. (2016). Sports-related concussions—media, science and policy. Nature Reviews Neurology.
Marin, J. R., Weaver, M. D., Yealy, D. M., & Mannix, R. C. (2014). Trends in visits for traumatic brain injury to emergency departments in the United States. JAMA, 311(18), 1917–1919.
McCrory, P., Meeuwisse, W. H., Aubry, M., Cantu, B., Dvořák, J., Echemendia, R. J., et al. (2013). Consensus statement on concussion in sport: the 4th International Conference on Concussion in Sport held in Zurich, November 2012. Br J Sports Med, 47(5), 250–258.
Ministère de la Santé du Québec (2017a). Regie de l'Assurance Maladie du Quebec. Available from: http://www.ramq.gouv.qc.ca/fr/Pages/accueil.aspx.
Ministère de la Santé du Québec (2017b). Eligibility for the Québec health insurance plan your obligations. [cited 2017 November 11, 2017]; Available from: https://tinyurl.com/ydbbn6of.
Moscote-Salazar, L. R. (2016). The elephant in the room: The case of re-categorization of moderate traumatic brain injury. Archivos de Medicina, 1(3), 18.
Pabian, P. S., Oliveira, L., Tucker, J., Beato, M., & Gual, C. (2017). Interprofessional management of concussion in sport. Physical Therapy in Sport, 23, 123–132.
Peeters, W., van den Brande, R., Polinder, S., Brazinova, A., Steyerberg, E. W., Lingsma, H. F., et al. (2015). Epidemiology of traumatic brain injury in Europe. Acta Neurochir, 157(10), 1683–1696.
Rimel, R. W., Giordani, B., Barth, J. T., Boll, T. J., & Jane, J. A. (1981). Disability caused by minor head injury. Neurosurgery, 9(3), 221–228.
Roozenbeek, B., Maas, A. I., & Menon, D. K. (2013). Changing patterns in the epidemiology of traumatic brain injury. Nat Rev Neurol, 9(4), 231–236.
Schlosser, A. J. (2016). Concussion knowledge and attitudes: the impact of hegemonic masculinity: The University of North Dakota.
Swaine, B. R., Tremblay, C., Platt, R. W., Grimard, G., Zhang, X., & Pless, I. B. (2007). Previous head injury is a risk factor for subsequent head injury in children: a longitudinal cohort study. Pediatrics, 119(4), 749–758.
Tator, C. H. (2013). Concussions and their consequences: current diagnosis, management and prevention. Can Med Assoc J, 185(11), 975–979.
Taylor, A. M., Nigrovic, L. E., Saillant, M. L., Trudell, E. K., Proctor, M. R., Modest, J. R., et al. (2015). Trends in ambulatory care for children with concussion and minor head injury from eastern Massachusetts between 2007 and 2013. J Pediatr, 167(3), 738–744.
Wolfe, C. (2015). Traumatic brain injury (TBI): comprehensive review: University of Pittsburgh.
Zemek R, Duval S, Demattero C, et al. Guidelines for diagnosing and managing pediatric concussion. Toronto: Ontario Neurotrauma Foundation, 2014a.
Zemek, R., Maps, K. E., & Farion, K. J. (2014b). Knowledge of paediatric concussion among front-line primary care providers/Les connaissances des dispensateurs de soins de première ligne sur les commotions cérébrales en pédiatrie. Paediatr Child Health, 19(9), 475.
Zemek, R. L., Grool, A. M., Rodriguez Duque, D., DeMatteo, C., Rothman, L., Benchimol, E. I., et al. (2017). Annual and seasonal trends in ambulatory visits for pediatric concussion in Ontario between 2003 and 2013. J Pediatr, 181, 222–228 e2.
Zhang, A. L., Sing, D. C., Rugg, C. M., Feeley, B. T., Senter, C. The rise of concussions in the adolescent population. Orthopaedic Journal of Sports Medicine 2016;4(8):2325967116662458. https://doi.org/10.1177/2325967116662458
Zonfrillo, M. R., Kim, K. H., & Arbogast, K. B. (2015). Emergency department visits and head computed tomography utilization for concussion patients from 2006 to 2011. Acad Emerg Med, 22(7), 872–877.
Acknowledgements
We thank Mr. Claude Verville, analyst at RAMQ, for his help and support in providing the data. We also thank Dr. Roger Zemek, and all the contributing authors of the Ontario study, who provided numerous supplemental tables and data, without which the comparisons with Quebec’s data would have been impossible.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Keays, G., Friedman, D. & Gagnon, I. Rates of concussions and minor head injuries in Quebec, 2003 and 2016, in children under 18 years old, and comparisons with Ontario’s rates of mild traumatic brain injuries. Can J Public Health 109, 52–60 (2018). https://doi.org/10.17269/s41997-018-0037-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.17269/s41997-018-0037-6