Abstract
Objective
Vitamin D intake in childhood is primarily for the prevention of rickets. Inconsistent evidence has associated adequate blood concentrations with a decreased risk of certain health conditions. Further, obese individuals may have lower vitamin D status. The estimated average requirement (EAR) for children recently doubled to 400 IU/day. Our aim was to examine dietary intake of vitamin D in different body mass index (BMI) categories, in addition to assessing determinants.
Methods
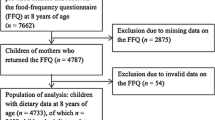
Data from two provincial surveys of grade 5 children, including a food frequency questionnaire and measured BMI, were used. Rao-Scott chi-square statistic tested the bivariate association between provinces and adequate dietary vitamin D intake. Key correlates were examined using multilevel logistic regression.
Results
Those below the EAR differed between Alberta (78%) and Nova Scotia (81 %). Those drinking <2 glasses of milk/day had 0.02 times the odds of meeting the EAR (95% CI: 0.01 -0.02) compared to those drinking more. No significant difference was observed for BMI, though those consuming <1 glass of milk/day were more likely to be obese than those consuming >-2 glasses/day. Income and physical activity were negatively correlated with meeting the EAR.
Conclusion
Many children did not meet the EAR for vitamin D from dietary sources and milk consumption was an important determinant. Given trends towards a more sedentary lifestyle and limited sun exposure, we recommend prioritizing public health efforts to support dietary vitamin D intake alongside interventions to increase physical activity and reduce sedentary behaviour. Further investigation is required to determine the need for targeted strategies for obese children.
Résumé
Objectif
L’apport en vitamine D durant l’enfance sert principalement à prévenir le rachitisme. Bien que les données probantes divergent, des études associent des concentrations sanguines adéquates à un moindre risque de contracter certains troubles médicaux. De plus, les personnes obèses pourraient avoir un statut plus faible en vitamine D. Le besoin moyen estimatif (BME) en vitamine D des enfants a récemment été doublé à 400 Ul/jour. Notre but était d’examiner l’apport alimentaire en vitamine D dans différentes catégories de l’indice de masse corporelle (IMC), en plus d’en évaluer les déterminants.
Méthode
Nous avons utilisé les données de deux enquêtes provinciales auprès d’élèves de 5e année comportant un questionnaire sur la fréquence de consommation des produits alimentaires et des mesures de l’IMC des élèves. Le test du khi-carré de Rao-Scott a analysé l’association bivariée entre les deux provinces et la suffisance de l’apport alimentaire en vitamine D. Les principaux corrélats ont été examinés par régression logistique multiniveau.
Résultats
La proportion d’enfants dont l’apport est en-deçà du BME était différente en Alberta (78 %) et en Nouvelle-Écosse (81 %). Les enfants qui buvaient <2 verres de lait/jour avaient 0,02 fois la probabilité d’avoir un apport supérieur ou égal au BME (IC de 95 %: 0,01 -0,02) que ceux qui en buvaient plus. Aucun écart significatif n’a été observé pour l’IMC, mais les enfants qui consommaient <1 verre de lait/jour étaient plus susceptibles d’être obèses que ceux qui en consommaient >-2 verres/jour. Le revenu et l’activité physique présentaient des corrélations négatives avec le statut par rapport au BME.
Conclusion
De nombreux enfants avaient un apport en vitamine D de sources alimentaires en-deçà du BME, et la consommation de lait en était un important déterminant. Étant donné la tendance à la sédentarisation des modes de vie et l’exposition limitée au soleil, nous recommandons de privilégier les efforts de santé publique qui appuient l’apport alimentaire en vitamine D en plus des interventions pour accroître l’activité physique et réduire les comportements sédentaires. Il est nécessaire de pousser la recherche pour déterminer s’il faudrait des stratégies ciblant les enfants obèses.
Similar content being viewed by others
References
Canadian adolescents meet their nutrient requirements through food intake alone? Health Canada, Ottawa, ON, 2012. Available at: https://doi.org/www.hc-sc.gc.ca/fn-an/surveill/nutrition/commun/art-nutr-adol-eng.php (Accessed December 17, 2013).
Gillis L, Gillis A. Nutrient inadequacy in obese and non-obese youth. Can J Diet Pract Res 2005;66(4):237–42.
Vanlint S. Vitamin D and obesity. Nutrients 2013;5(3):949–56.
Alemzadeh R, Kichler J, Babar G, Calhoun M. Hypovitaminosis D in obese children and adolescents: Relationship with adiposity, insulin sensitivity, ethnicity, and season. Metabolism 2008;57(2):183–91.
Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D. Washington, DC: National Academy Press, 2010.
Canada’s Food and Drugs Act & Regulations. Health Canada, Ottawa, ON. Available at: https://doi.org/www.hc-sc.gc.ca/fn-an/legislation/acts-lois/act-loi_reg-eng.php (Accessed May 3, 2013).
Fortmann SP, Burda BU, Senger CA, Lin J, Beil T, O’ Connor E, Whitlock ER. Vitamin, Mineral, and Multivitamin Supplements for the Primary Prevention of Cardiovascular Disease and Cancer: A Systematic Evidence Review for the U.S. Preventive Services Task Force. Evidence Report No. 108. AHRQ Public No. 14-05199-EF-1. Rockville, MD: Agency for Healthcare Research and Quality, 2013.
Abrams SA, Coss- Bu JA, Tiosano D. Vitamin D: Effects on childhood health and disease. Nat Rev Endocrinol 2013;9(3):162–70.
Salo A, Logomarsino JV. Relationship of vitamin D status and cardiometabolic risk factors in children and adolescents. Pediatr Endocrinol Rev 2011;9(1):456–62.
CLASS II: Children’s Lifestyle and School Performance Study Dalhousie University, Halifax, NS. Available at: https://doi.org/nsclass.ca (Accessed December 17, 2013).
REAL Kids Alberta. University of Alberta, Edmonton, AB. Available at: https://doi.org/www.realkidsalberta.ca/ (Accessed December 17, 2013).
Rockett HR, Breitenbach M, Frazier AL, Witschi J, Wolf Am, Field AE, Colditz GA. Validation of a youth/adolescent food frequency questionnaire. Prev Med 1997;26(6):808–16.
Cole TJ, Bellizi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ 2000; 320(7244): 1240–43.
Canadian Nutrient File (CNF), 2010. Health Canada. Available at: https://doi.org/www.hc-sc.gc.ca/fn-an/nutrition/fiche-nutri-data/cnf_downloads-telechargement_fcen-eng.php (Accessed November 1, 2013).
Willet W. Nutritional Epidemiology, Third Edition. New York, NY: Oxford University Press, 2012.
Fung C, Kuhle S, Lu C, Purcell M, Schwartz M, Storey K, Veugelers PJ. From “best practice” to “next practice”: The effectiveness of school-based health promotion in improving healthy eating and physical activity and preventing childhood obesity. Int J Behav Nutr Phys Act 2012;9:27.
Kim S, Haines PS, Siega- Riz AM, Popkin BM. The Diet Quality Index- International (DQI-I) provides an effective tool for cross-national comparison of diet quality as illustrated by China and the United States. J Nutr 2003;133(11):3476–84.
Janz KF, Lutuchy EM, Wenthe P, Levy SM. Measuring activity in children and adolescents using self-report: PAQ-C and PAQ-A. Med Sci Sports Exerc 2008;40(4):767–72.
Rao J, Scott A. The analysis of categorical data from complex sample surveys: Chi-squared tests for goodness of fit and independence in two-way tables. J Am Stat Assoc 1981;76:221–30.
Veugelers PJ, Fitzgerald AL. Prevalence of and risk factors for childhood overweight and obesity. CMAJ 2005;173(6):607–13.
Simen-Kapeu A, Veugelers PJ. Should public health interventions aimed at reducing childhood overweight and obesity be gender-focused? BMC Public Health 2010;10:340.
Fulgoni VL III, Keast DR, Bailey RL, Dwyer J. Foods, fortificants and dietary supplements: Where do Americans get their nutrients? J Nutr 2011;141:1847–54.
Mark S, Lambert M, O’ Loughlin J, Gray- Donald K. Household income, food insecurity and nutrition in Canadian youth. Can J Public Health 2012;103(2):94–99.
Cash SB, Wang C, Goddard EW. Dairy products and consumer demand for health foods. Advances in Dairy Technology 2005;17:67–80.
Sebastian RS, Goldman JD, Enns CW, LaComb RP. Fluid milk consumption in the United States. Food surveys research group dietary data brief no. 3, 2010. (United States Department of Agriculture). Available at: https://doi.org/www.ars.usda.gov/SP2UserFiles/Place/12355000/pdf/DBrief/3_milk_consumption_0506.pdf (Accessed February 19, 2014).
Garriguet D. Canadians’ eating habits. Health Rep 2007;18(2):17–32.
Garriguet D. Beverage consumption of children and teens. Health Rep 2008;19(4):17–22.
Whiting SJ, Langlois KA, Vatanparast H, Greene-Finestone LS. The vitamin D status of Canadians relative to the 2011 Dietary Reference Intakes: An examination in children and adults with and without supplement use. Am J Clin Nutr 2011;94(1):128–35.
Sarafin K, Hidiroglou N, Brooks S. A comparison of two immunoassay methods for analyzing plasma 25-hydroxyvitamin D. Open Clin Chem J 2011;4:45–49.
Au LE, Rogers GT, Harris SS, Dwyer JT, Jacques PF, Sacheck JM. Associations of vitamin D intake with 25-hydroxyvitamin D in overweight and racially/ethnically diverse US children. J Acad Nutr Diet 2013;113(11):1511–16.
Salamoun MM, Kizirian AS, Tannous RI, Nabulsi MM, Choucair MK, Deeb ME, et al. Low calcium and vitamin D intake in healthy children and adolescents and their correlates. Eur J Clin Nutr 2005;59(2):177–84.
Roth DE, Martz P, Yeo R, Prosser C, Bell M, Jones AB. Are national vitamin D guidelines sufficient to maintain adequate blood levels in children? Can J Public Health 2005;96(6):443–49.
Greene-Finestone LS, Langlois K, Whiting S. Characteristics of users of supplements containing vitamin D in Canada and associations between dose and 25-hydroxyvitamin D. Appl Physiol Nutr Metab 2013;38:707–15.
Author information
Authors and Affiliations
Corresponding author
Additional information
Funding sources: CLASS was funded through an operating grant from the Canadian Institutes of Health Research (CIHR [FRN: 93680]), and REAL Kids Alberta through a contract with Alberta Health. All interpretations and opinions in this article are those of the authors. Sara Kirk acknowledges support from a CIHR Canada Research Chair (CRC) in Health Services Research and an IWK Scholar Award. Paul Veugelers acknowledges his support through a CIHR CRC in Population Health, an Alberta Research Chair in Nutrition and Disease Prevention, and an Alberta Innovates Health Scholarship. Cynthia Colapinto is supported by a CIHR-Quebec Training Network in Perinatal Research postdoctoral fellowship.
Acknowledgements: The authors thank students, parents, schools and school jurisdictions in Nova Scotia and Alberta for their participation in and support for this research. We also thank the CLASS and REAL Kids Alberta coordinators, evaluation assistants and others involved in the data collection, as well as Connie Lu for data validation and management.
Conflict of Interest: None to declare.
Rights and permissions
About this article
Cite this article
Colapinto, C.K., Rossiter, M., Khan, M.K.A. et al. Obesity, lifestyle and socio-economic determinants of vitamin D intake: A population-based study of Canadian children. Can J Public Health 105, e418–e424 (2014). https://doi.org/10.17269/cjph.105.4608
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.17269/cjph.105.4608