Abstract
OBJECTIVES: Lifestyle interventions can reduce type 2 diabetes risk. The Primary Care Diabetes Prevention Program (PCDPP) was implemented by the Government of Ontario to lower diabetes risk. This study first evaluated the program, and second used a validated tool to estimate a potential population impact if the program were implemented more broadly in the province.
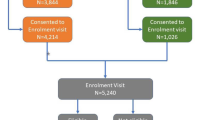
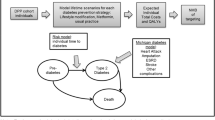
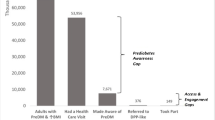
METHODS: PCDPP was implemented in six primary care settings serving communities with high mortality risk due to chronic diseases. In total, 1916 adults with prediabetes or metabolic syndrome were enrolled from January 2011 to December 2012. Body weight was the primary outcome variable, and was modeled using four time periods (i.e., baseline, 3rd, 6th and 9th month). The intervention effect was estimated using multilevel mixed-effects linear regression, and was stratified by gender and age. In the population impact analysis, a number needed to treat (NNT) for the intervention to prevent one case of diabetes and an absolute number of diabetes cases averted were estimated.
RESULTS: Weight loss over 9 months was 7.5% (or 6.8 kg), with 7.4% (or 6.4 kg) in females and 8.6% (or 8.6 kg) in males. When modeled, changes in weight were all statistically significant. The models for male participants predicted, however, some gains in weight in the last 3 months of the program. Dropout rates were 26.8%, 46.8% and 63.0% at 3rd, 6th and 9th month respectively. Scaling up the program would produce an NNT of approximately 36 and would avert 6401 cases of diabetes in five years.
CONCLUSION: PCDPP may represent a potentially effective tool for population-level diabetes risk reduction.
Résumé
OBJECTIFS: Les interventions sur le mode de vie peuvent réduire le risque de diabète de type 2. Le Programme de prévention du diabète en soins primaires (PPDSP) a été mis en œuvre par le gouvernement de l’Ontario pour diminuer le risque de diabète. Premièrement, notre étude a évalué ce programme; deuxièmement, elle a utilisé un outil validé pour estimer l’incidence possible sur la population de l’application du programme à plus grande échelle dans la province.
MÉTHODE: Le PPDSP a été mis en œuvre dans six milieux de soins primaires servant des communautés où le risque de mortalité dû aux maladies chroniques est élevé. En tout, 1 916 adultes atteints de prédiabète ou du syndrome métabolique ont été inscrits entre janvier 2011 et décembre 2012. Le poids était la principale variable de résultat, et nous l’avons modélisé à l’aide de quatre intervalles (base de référence, 3e, 6e et 9e mois). Nous avons estimé l’effet de l’intervention au moyen d’une régression linéaire multiniveau à effets mixtes, et nous l’avons stratifié selon le sexe et l’âge. Dans l’analyse d’incidence sur la population, nous avons estimé le nombre nécessaire pour traiter (NNT) pour que l’intervention prévienne un cas de diabète et le nombre absolu de cas de diabète évités.
RÉSULTATS: La perte de poids sur 9 mois a été de 7,5 % (ou 6,8 kg), soit 7,4 % (ou 6,4 kg) chez les femmes et 8,6 % (ou 8,6 kg) chez les hommes. Avec la modélisation, les changements du poids étaient tous significatifs. Les modèles pour les participants de sexe masculin ont cependant prédit des gains de poids au cours des 3 derniers mois du programme. Les taux d’abandon ont été de 26,8 %, 46,8 % et 63 % au 3e, 6e et 9e mois, respectivement. La mise à l’échelle du programme produirait un NNT d’environ 36 et éviterait 6 401 cas de diabète sur cinq ans.
CONCLUSION: Le PPDSP est un outil potentiellement efficace pour réduire le risque de diabète dans la population.
Similar content being viewed by others
References
Shaw J, Sicree R, Zimmet P. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pr 2010;87(1):4–14. doi: 10.1016/j.diabres. 2009.10.007.
Lipscombe LL, Hux JE. Trends in diabetes prevalence, incidence, and mortality in Ontario, Canada 1995–2005: A population-based study. Lancet 2007;369(9563):750–56. doi: 10.1016/S0140-6736(07)60361-4.
Booth G, Polsky J, Gozdyra P, Cauch-Dudek K, Kiran T, Shah BR, et al. Regional Measures of Diabetes Burden in Ontario. Toronto, ON: Institute for Clinical Evaluative Sciences, 2012.
Emerging Risk Factors Collaboration, Sarwar N, Gao P, Seshasai SR, Gobin R, Kaptoge S, et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: A collaborative meta-analysis of 102 prospective studies. Lancet 2010;375(9733):2215–22. PMID: 20609967. doi: 10.1016/ S0140-6736(10)60484-9.
Diabetes Control and Complications Trial Research Group (DCCT). The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993;30(329):977–86. doi: 10.1056/NEJM199309303291401.
UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998; 352(9131):837–53. doi: 10.1016/S0140-6736(98)07019-6.
Alberti KGMM, Zimmet P, Shaw J. International diabetes federation: A consensus on type 2 diabetes prevention. Diabet Med 2007;24(5):451–63. PMID: 17470191. doi: 10.1111/j.1464-5491.2007.02157.x.
Tuomilehto J, Schwarz P, Lindstrom J. Long-term benefits from lifestyle interventions for type 2 diabetes prevention: Time to expand the efforts. Diabetes Care 2011;34(Suppl 2):S210–14. doi: 10.2337/dc11-s222.
Goldenberg R, Punthakee Z. Definition, classification and diagnosis of diabetes, prediabetes and metabolic syndrome. Can J Diabetes 2013;37: S8–11. PMID: 24070969. doi: 10.1016/j.jcjd.2013.01.011.
Tuomilehto J, Lindström J, Eriksson J, Valle T, Hämäläinen H, Ilanne-Parikka P, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 2001;344(18):1343–50. PMID: 11333990. doi: 10.1056/NEJM200105033441801.
Pan X, Cao H-B, Li G-W, Liu P-A, Hu Y-H, Jiang X-G, et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. Diabetes Care 1997;20(4):537–44. PMID: 9096977. doi: 10.2337/diacare.20.4.537.
Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002; 346(6):393–403. doi: 10.1056/NEJMoa012512.
Diabetes Prevention Program Research Group, Knowler WC, Fowler SE, Hamman RF, Christophi CA, Hoffman HJ, et al. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet 2009;374(9702):1677–86. doi: 10.1016/S0140-6736(09)61457-4.
Seidel MC, Powell RO, Zgibor JC, Siminerio LM, Piatt GA. Translating the Diabetes Prevention Program into an urban medically underserved community: A nonrandomized prospective intervention study. Diabetes Care 2008;31(4):684–89. PMID: 18252904. doi: 10.2337/dc07-1869.
Lindström J, Ilanne-Parikka P, Peltonen M, Aunola S, Eriksson JG, Hemiö K, et al. Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: Follow-up of the Finnish Diabetes Prevention Study. Lancet 2006;368(9548):1673–79. doi: 10.1016/S0140-6736(06)69701-8.
Ma J, Yank V, Xiao L, Lavori PW, Wilson SR, Rosas LG, et al. Translating the Diabetes Prevention Program lifestyle intervention for weight loss into primary care: A randomized trial. JAMA Intern Med 2013;173(2):113. PMID: 23229846. doi: 10.1001/2013.jamainternmed.987.
Kramer MK, McWilliams JR, Chen H-Y, Siminerio LM. A community-based diabetes prevention program: Evaluation of the group lifestyle balance program delivered by diabetes educators. Diabetes Educ 2011;37(5):659–68. PMID: 21918204. doi: 10.1177/0145721711411930.
Jiang L, Manson SM, Beals J, Henderson WG, Huang H, Acton KJ, et al. Translating the Diabetes Prevention Program into American Indian and Alaska Native communities: Results from the Special Diabetes Program for Indians Diabetes Prevention demonstration project. Diabetes Care 2013; 36(7):2027–34. PMID: 23275375. doi: 10.2337/dc12-1250.
Kramer MK, Kriska AM, Venditti EM, Miller RG, Brooks MM, Burke LE, et al. Translating the Diabetes Prevention Program: A comprehensive model for prevention training and program delivery. Am J Prev Med 2009;37(6):505–11. PMID: 19944916. doi: 10.1016/j.amepre.2009.07.020.
Walsemann KM, Ailshire JA, Bell BA, Frongillo EA. Body mass index trajectories from adolescence to midlife: Differential effects of parental and respondent education by race/ethnicity and gender. Ethn Health 2012; 17(4):337–62. PMID: 22107248. doi: 10.1080/13557858.2011.635374.
Rosella LC, Manuel DG, Burchill C, Stukel TA, for the PHIAT-DM team. A population-based risk algorithm for the development of diabetes: Development and validation of the Diabetes Population Risk Tool (DPoRT). J Epidemiol Community Health 2011;65(7):613–20. PMID: 20515896. doi: 10. 1136/jech.2009.102244.
Manuel D, Rosella L, Tuna M, Bennett C. How Many Canadians Will be Diagnosed With Diabetes Between 2007 and 2017? Assessing Population Risk. Toronto, ON: Institute for Clinical Evaluative Sciences, 2010.
Cook R, Sackett D. The number needed to treat: A clinically useful measure of treatment effect. BMJ 1995;310(6977):452–54. PMID: 7873954. doi: 10.1136/ bmj.310.6977.452.
Sach TH, Barton GR, Doherty M, Muir KR, Jenkinson C, Avery AJ. The relationship between body mass index and health-related quality of life: Comparing the EQ-5D, EuroQol VAS and SF-6D. Int J Obes 2007;31(1): 189–96. doi: 10.1038/sj.ijo.0803365.
Korda RJ, Joshy G, Paige E, Butler JRG, Jorm LR, Liu B, et al. The relationship between body mass index and hospitalisation rates, days in hospital and costs: Findings from a large prospective linked data study. PLoS ONE 2015; 10(3):e0118599. PMID: 25739093. doi: 10.1371/journal.pone.0118599.
United States Preventive Screening Task Force. Screening for Type 2 Diabetes Mellitus in Adults, 2008 (Accessed November 1, 2013).
Canadian Task Force on Preventative Health Care. Recommendations on screening for type 2 diabetes in adults. Can Med Assoc J 2012;184(15): 1687–96. doi: 10.1503/cmaj.120732.
Author information
Authors and Affiliations
Corresponding author
Additional information
Conflict of Interest: All authors except for Laura Rosella either work or worked for the Ontario Ministry of Health and Long-Term Care at the time this program was implemented and/or the review of the program was conducted.
Rights and permissions
About this article
Cite this article
Hillmer, M., Sandoval, G.A., Elliott, J.A. et al. Diabetes risk reduction in primary care: Evaluation of the Ontario Primary Care Diabetes Prevention Program. Can J Public Health 108, e176–e184 (2017). https://doi.org/10.17269/CJPH.108.5287
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.17269/CJPH.108.5287