Abstract
Background
Parents are increasingly placing amber necklaces on their infants or toddlers to prevent teething pain. The use of the necklaces can pose a risk of death by strangulation, however, there are no data on the potential infectious risk linked to bacterial colonisation associated with the necklaces.
Objectives
We aimed to analyse bacterial colonisation of amber necklaces worn by children during hospital consultations.
Material & methods
This prospective observational study included all children wearing a teething necklace at consultation in the Paediatric Dermatology and the Paediatric Emergency Department of our hospital from April to December 2014. The study included 27 children (median age: 10.7 months; 70.4% female). The surface of necklaces underwent bacteriological analyses using three different agar cultures. Parents completed a brief questionnaire to provide reasons for using necklaces and express awareness of risks.
Results
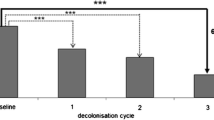
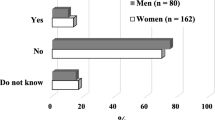
One child had a history of impetigo. All necklaces were colonised by bacteria (median: four species per necklace [range: 1-9]); 32 different species were found, the most frequent being coagulase-negative staphylococci (Staphylococcus epidermidis in 88.9% of cases). In three cases, methicillin-sensitive Staphylococcus aureus was found. The most frequent reason for wearing a necklace was to prevent teething pain (n = 17; 63.0%); the necklace was judged effective (moderately/highly effective) in 74.1% of cases, however, 70.4% of parents considered the use of the necklace to be risky.
Conclusion
Amber necklaces may be highly colonised by commensal germs of the skin, mainly coagulase-negative staphylococci. Although these bacteria are saprophytes, they may become pathogenic in particular conditions.
Similar content being viewed by others
References
Reinberg O. Les colliers d’ambre sont dangereux pour les petits enfants. Paediatrica 1992; 4: 24–7.
Reinberg O. Collier d’ambre: le danger est toujours présent. Paediatrica 2009; 20: 75.
Korsaga-Somé N, Maruani A, Nadal M, et al. Acné et folliculites du nourrisson liées à un mésusage du liniment oléo-calcaire. Ann Dermatol Venereol 2015; 142: 577–8.
Maruani A, Lorette G, Barbarot S, et al. Re-emergence of papulonodular napkin dermatitis with use of reusable diapers: report of 5 cases. Eur J Dermatol 2013; 23: 246–9.
Taillefer A, Casasoprana A, Cascarigny F, Claudet I. Port de colliers de dentition chez le nourrisson. Arch Pediatr 2012; 19: 1058–64.
Zigon G, Gregori D, Corradetti R, et al. Child mortality due to suffocation in Europe (1980-1995): a review of official data. Acta Otorhinolaryngol Ital 2006; 26: 154–61.
Tarrago SB. Prevention of choking, strangulation, and suffocation in childhood. WMJ 2000; 99: 43–6.
Chin N, Berns SD. Near-hanging caused by a toy necklace. Ann Emerg Med 1995; 26: 522–5.
Feldmann KW, Simms RJ. Strangulation in childhood: epidemiology and clinical course. Pediatrics 1980; 65: 1079–85.
Legifrance. Decret no. 91-1292 (20 December 1991) on the prevention of risks linked to childcare articles and toys. Available at: http://www.legifrance.gouv.fr/affichTexte.do?cidTexte = JORFTEXT000000701248&categorieLien = cid.(last accessed 20 October 2015).
Hoffman PN, Cooke EM, McCarville MR, Emmerson AM. Microorganisms isolated from skin under wedding rings worn by hospital staff. BMJ 1985; 290: 206–7.
Trick WE, Vernon MO, Hayes RA, et al. Impact of ring wearing on hand contamination and comparison of hand hygiene agents in a hospital. Clin Infect Dis 2003; 36: 1383–90.
Wongworawat MD, Jones SG. Influence of rings on the efficacy of hand sanitization and residual bacterial contamination. Infect Control Hosp Epidemiol 2007; 28: 351–3.
Yildirim I, Ceyhan M, Cengiz AB, et al. A prospective comparative study of the relationship between different types of ring and microbial hand colonization among pediatric intensive care unit nurses. Int J Nurs Stud 2008; 45: 1572–6.
Hughes WT, Williams B, Williams B, Pearson T. The nosocomial colonization of T. Bear. Infect Control 1986; 7: 495–500.
Van R, Marrow AL, Reves RR, Pickering LK. Environmental contamination in child day-care centers. Am J Epidemiol 1991; 133: 460–70.
Rogers M, Weinstock DM, Eagan J, et al. Rotavirus outbreak on a pediatric oncology floor: possible association with toys. Am J Infect Control 2000; 28: 378–80.
Davies MW, Mehr S, Garland ST, Morley CJ. Bacterial colonization of toys in neonatal intensive care cots. Pediatrics 2000; 106: E18.
Avila-Aguero ML, German G, Paris MM, Herrera JF. Toys in a pediatric hospital: are they a bacterial source? Am J Infect Control 2004; 32: 287–90.
Richet H, Hubert B, Nitemberg G, et al. Prospective multicenter study of vascular-catheter-related complications and risk factors for positive central-catheter cultures in intensive care unit patients. J Clin Microbiol 1990; 28: 2520–5.
Otto M. Staphylococcus epidermidis-the “accidental” pathogen. Nat Rev Microbiol 2009; 7: 555–67.
Uckay I, Pittet D, Vaudaux P, et al. Foreign body infections due to Staphylococcus epidermidis. Ann Med 2009; 41: 109–19.
Becker K, Heilmann C, Peters G. Coagulase-negative staphylococci. Clin Microbiol Rev 2014; 27: 870–926.
Costerton JW, Stewart PS, Greenberg EP. Bacterial biofilms: a common cause of persistent infections. Science 1999; 284: 1318–22.
De Silva GD, Kantzanou M, Justice A, et al. The ica operon and biofilm production in coagulase-negative Staphylococci associated with carriage and disease in a neonatal intensive care unit. J Clin Microbiol 2002; 40: 382–8.
Moolenaar RL, Crutcher JM, San Joaquin VH, et al. A prolonged outbreak of Pseudomonas aeruginosa in a neonatal intensive care unit: did staff fingernails play a role in disease transmission? Infect Control Hosp Epidemiol 2000; 21: 80–5.
Foca M, Jakob K, Whittier S, et al. Endemic Pseudomonas aeruginosa infection in a neonatal intensive care unit. N Engl J Med 2000; 343: 695–700.
Parry MF, Grant B, Yukna M, et al. Candida osteomyelitis and diskitis after spinal surgery: an outbreak that implicates artificial nail use. Clin Infect Dis 2001; 32: 352–7.
Arrowsmith VA, Maunder JA, Sargent R, Taylor R. Removal of nail polish and finger rings to prevent surgical infection. Cochrane Database Syst Rev 2001; 4: CD003325.
Wilde J, Van R, Picketing L, et al. Detection of rotaviruses in the day care environment by reverse transcriptase polymerase chain reaction. J Infect Dis 1992; 166: 507–11.
Owais AI, Zawaideh F, Bataineh O. Challenging parents’ myths regarding their children’s teething. Int J Dent Hyg 2010; 8: 28–34.
Kossowsky J, Kaptchuk TJ. Placebo effects in infants, toddlers, and parents. JAMA Pediatr 2015; 169: 505.
Whalley B, Hyland ME. Placebo by proxy: the effect of parents’ beliefs on therapy for children’s temper tantrums. J Behav Med 2013; 36: 341–6.
Piolot M, Fagot JP, Rivière S, et al. Homeopathy in France in 2011-2012 according to reimbursements in the French national health insurance database (SNIIRAM). Fam Pract 2015; 32: 442–8.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Machet, P., Lanotte, P., Giraudeau, B. et al. Amber necklaces: reasons for use and awareness of risk associated with bacterial colonisation. Eur J Dermatol 26, 580–585 (2016). https://doi.org/10.1684/ejd.2016.2871
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1684/ejd.2016.2871