Abstract
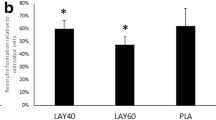
To address the controversial issue of the toxicity of dental alloys and silver nanoparticles in medical applications, an in vivo-like LO2 3-D model was constructed within polyvinylidene fluoride hollow fiber materials to mimic the microenvironment of liver tissue. The use of microscopy methods and the measurement of liver-specific functions optimized the model for best cell performances and also proved the superiority of the 3-D LO2 model when compared with the traditional monolayer model. Toxicity tests were conducted using the newly constructed model, finding that four dental castings coated with silver nanoparticles were toxic to human hepatocytes after cell viability assays. In general, the toxicity of both the castings and the coated silver nanoparticles aggravated as time increased, yet the nanoparticles attenuated the general toxicity by preventing metal ion release, especially at high concentrations.
概要
目的
应用体外三维模型模拟肝脏组织微环境,更真实地反映和评估纳米银材料和牙科合金对于人体的潜在毒性。
创新点
借助中空纤维管和胶原蛋白首次构建了LO2 细胞三维聚集体,并将该模型应用到医用材料毒性的评价中。
方法
首先,采用扫描电镜观察中空纤维材料的孔径, 确保营养物质的正常交换。然后,将混合有胶原 蛋白的细胞悬液注入到中空纤维管的内胆,通过 尿素氮和白蛋白检测,确定最佳细胞密度进行长 期培养。在显微镜下观察细胞聚集体的形态,确 保模型的成功建立。其次,应用水热法制作纳米 银颗粒并将颗粒包裹到预先购买的合金材料上。 最后,用不同牙科材料的浸提液培养细胞1、3 和5 天,通过MTT 检测细胞死亡率,从而间接 评价材料的毒性。
结论
中空纤维材料的表征结果显示该材料具有较好的耐热性和细胞粘附性,孔径大小适宜营养物质交 换,可以应用到三维模型的构建中。通过白蛋白 和尿素氮两个指标来评价三维模型的活性,发现 每毫升5×104 细胞的浓度最适宜细胞生长(图4)。 进一步模型评价表明,相比于传统单层培养的细胞,三维模型中的细胞能保持长期活力(图6) 且可以在更短时间内对低药物浓度作出反应。
Similar content being viewed by others
References
Al-Hiyasat AS, Bashabsheh OM, Darmani H, 2002. Elements released from dental casting alloys and their cytotoxic effects. Int J Prosthodont, 155:473–478.
Aksakal B, Yildirim OS, Gul H, 2004. Metallurgical failure analysis of various implant materials used in orthopedic applications. J Fail Anal Prev, 43:17–23. https://doi.org/10.1007/s11668-996-0007-9
Allaker RP, 2010. The use of nanoparticles to control oral biofilm formation. J Dent Res, 8911:1175–1186. https://doi.org/10.1177/0022034510377794
AshaRani PV, Mun GLK, Hande MP, et al., 2009. Cytotoxicity and genotoxicity of silver nanoparticles in human cells. ACS Nano, 32:279–290. https://doi.org/10.1021/nn800596w
Burcham PC, 2014. Target-organ toxicity: liver and kidney. In: An Introduction to Toxicology. Springer London, p.151–187. https://doi.org/10.1007/978-1-4471-5553-9_6
Chu Q, Zhao Y, Shi X, et al., 2017. in vivo-like 3-D model for sodium nitrite-and acrylamide-induced hepatotoxicity tests utilizing HepG2 cells entrapped in micro-hollow fibers. Sci Rep, 71:14837. https://doi.org/10.1038/s41598-017-13147-z
Dambach DM, Andrews BA, Moulin F, 2005. New technologies and screening strategies for hepatotoxicity: use of in vitro models. Toxicol Pathol, 331:17–26. https://doi.org/10.1080/01926230590522284
de Bartolo L, Salerno S, Morelli S, et al., 2006. Long-term maintenance of human hepatocytes in oxygen-permeable membrane bioreactor. Biomaterials, 2727:4794–4803. https://doi.org/10.1016/j.biomaterials.2006.05.015
Fadeel B, Garcia-Bennett AE, 2010. Better safe than sorry: understanding the toxicological properties of inorganic nanoparticles manufactured for biomedical applications. Adv Drug Deliv Rev, 623:362–374. https://doi.org/10.1016/j.addr.2009.11.008
García-Contreras R, Argueta-Figueroa L, Mejía-Rubalcava C, et al., 2011. Perspectives for the use of silver nanoparticles in dental practice. Int Dent J, 616:297–301. https://doi.org/10.1111/j.1875-595X.2011.00072.x
Gómez-Lechón MJ, Castell JV, Donato MT, 2007. Hepatocytes— the choice to investigate drug metabolism and toxicity in man: in vitro variability as a reflection of in vivo. Chem Biol Interact, 1681:30–50. https://doi.org/10.1016/j.cbi.2006.10.013
Hamouda IM, 2012. Current perspectives of nanoparticles in medical and dental biomaterials. J Biomed Res, 263: 143–151.
Hanawa T, 2002. Evaluation techniques of metallic biomaterials in vitro. Sci Technol Adv Mater, 34:289–295. https://doi.org/10.1016/S1468-6996(02)00028-1
Hiromoto S, Noda K, Hanawa T, 2002. Development of electrolytic cell with cell-culture for metallic biomaterials. Corros Sci, 445:955–965. https://doi.org/10.1016/S0010-938X(01)00110-X
Hussain SM, Hess KL, Gearhart JM, et al., 2005. In vitro toxicity of nanoparticles in BRL 3A rat liver cells. Toxicol in Vitro, 197:975–983. https://doi.org/10.1016/j.tiv.2005.06.034
Kino Y, Sawa M, Kasai S, et al., 1998. Multiporous cellulose microcarrier for the development of a hybrid artificial liver using isolated hepatocytes. J Surg Res, 791:71–76. https://doi.org/10.1006/jsre.1998.5389
Kittler S, Greulich C, Diendorf J, et al., 2010. Toxicity of silver nanoparticles increases during storage because of slow dissolution under release of silver ions. Chem Mater, 2216:4548–4554. https://doi.org/10.1021/cm100023p
Kmiec Z, 2001. Cooperation of liver cells in the synthesis and degradation of eicosanoids. In: Cooperation of Liver Cells in Health and Disease. Springer Berlin Heidelberg, p.51–59.
Li Y, Lv XL, 2001. Research progress of modification of poly (vinylidene fluoride) porous membrane. J Tianjin Polytech Univ, 5:74–78.
Manivasagam G, Dhinasekaran D, Rajamanickam A, 2010. Biomedical implants: corrosion and its prevention— a review. Recent Pat Corros Sci, 21:40–54. https://doi.org/10.2174/1877610801002010040
Mizumoto H, Ishihara K, Nakazawa K, et al., 2008. A new culture technique for hepatocyte organoid formation and long-term maintenance of liver-specific functions. Tissue Eng Part C Methods, 142:167–175. https://doi.org/10.1089/ten.tec.2007.0373
Morones JR, Elechiguerra JL, Camacho A, et al., 2005. The bactericidal effect of silver nanoparticles. Nanotechnology, 1610:2346–2353. https://doi.org/10.1088/0957-4484/16/10/059
Niinomi M, Hattori T, Morikawa K, et al., 2002. Development of low rigidity β-type titanium alloy for biomedical applications. Mater Trans, 4312:2970–2977. https://doi.org/10.2320/matertrans.43.2970
Ren YB, Yang C, Liang Y, 2002. Research and development of new biomedical metallic material. Mater Rev, 162: 12–15.
Schmalz G, Langer H, Schweikl H, 1998. Cytotoxicity of dental alloy extracts and corresponding metal salt solutions. J Dent Res, 7710:1772–1778. https://doi.org/10.1177/00220345980770100401
Silva T, Pokhrel LR, Dubey B, et al., 2014. Particle size, surface charge and concentration dependent ecotoxicity of three organo-coated silver nanoparticles: comparison between general linear model-predicted and observed toxicity. Sci Total Environ, 468-469:968–976. https://doi.org/10.1016/j.scitotenv.2013.09.006
Sung JH, Ji JH, Yoon JU, et al., 2008. Lung function changes in Sprague-Dawley rats after prolonged inhalation exposure to silver nanoparticles. Inhal Toxicol, 206:567–574. https://doi.org/10.1080/08958370701874671
Wataha JC, 2000. Biocompatibility of dental casting alloys: a review. J Prosth Dent, 832:223–234. https://doi.org/10.1016/S0022-3913(00)80016-5
Wong KKY, Cheung SOF, Huang L, et al., 2009. Further evidence of the anti-inflammatory effects of silver nanoparticles. Chem Med Chem, 47:1129–1135. https://doi.org/10.1002/cmdc.200900049
Yamamoto A, Honma R, Sumita M, 1998. Cytotoxicity evaluation of 43 metal salts using murine fibroblasts and osteoblastic cells. J Biomed Mater Res, 392:331–340. https://doi.org/10.1002/(SICI)1097-4636(199802)39:2<331::AID-JBM22<3.0.CO;2-E
Zreiqat H, Howlett CR, Zannettino A, et al., 2002. Mechanisms of magnesium-stimulated adhesion of osteoblastic cells to commonly used orthopaedic implants. J Biomed Mater Res, 622:175–184. https://doi.org/10.1002/jbm.10270
Author information
Authors and Affiliations
Corresponding authors
Additional information
Project supported by the Zhejiang Provincial Natural Science Foundation of China (No. LZ14C200001) and the Public Welfare Project of Science Technology Department of Zhejiang Province (No. 2013c33139), China
Rights and permissions
About this article
Cite this article
Zhao, Yy., Chu, Q., Shi, Xe. et al. Toxicity testing of four silver nanoparticle-coated dental castings in 3-D LO2 cell cultures. J. Zhejiang Univ. Sci. B 19, 159–167 (2018). https://doi.org/10.1631/jzus.B1600482
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1631/jzus.B1600482