Abstract
Background
Historically, more than one-third of patients with ductal carcinoma in situ (DCIS) treated with breast-conserving surgery (BCS) underwent additional surgery. The SSO-ASTRO guidelines advise 2 mm margins for patients with DCIS having BCS and whole-breast radiation (WBRT). Here we examine guideline impact on additional surgery and factors associated with re-excision.
Patients and Methods
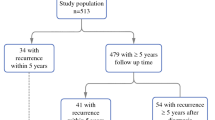
Patients treated with BCS for pure DCIS from August 2015 to January 2018 were identified. Guidelines were adopted on September 1, 2016, and all patients had separately submitted cavity-shave margins. Clinicopathologic characteristics, margin status, and rates of additional surgery were examined.
Results
Among 650 patients with DCIS who attempted BCS, 50 (8%) converted to mastectomy. Of 600 who had BCS as final surgery, 336 (56%) received WBRT and comprised our study group. One hundred twenty-eight (38%) were treated pre-guideline and 208 (62%) were treated post-guideline. Characteristics and margin status were similar between groups. The re-excision rate was 38% pre-guideline adoption and 29% post-guideline adoption (p = 0.09), with 91% having only one re-excision. Re-excision for ≥ 2 mm margins was uncommon (6% pre-guideline vs. 5% post-guideline). On multivariate analysis, younger age (OR 0.97, 95% CI 0.94–0.99, p = 0.02) and larger DCIS size (OR 1.43, 95% CI 1.2–1.8, p < 0.001) were predictive of re-excision; guideline era was not. Younger age (OR 0.93, 95% CI 0.9–0.97, p < 0.001) and larger size (OR 1.64, 95% CI 1.3–2.1, p < 0.001) were predictive of conversion to mastectomy, but residual tumor burden was low.
Conclusions
The SSO-ASTRO guidelines did not significantly change re-excision rates for DCIS in our practice, likely since re-excision for margins ≥ 2 mm was uncommon even prior to guideline adoption, dissimilar to historically observed variations in surgeon practices. Younger age and larger DCIS size were associated with additional surgery.

Similar content being viewed by others
References
Morrow M, Jagsi R, Alderman AK, et al. Surgeon recommendations and receipt of mastectomy for treatment of breast cancer. JAMA. 2009;302(14):1551–6.
Faverly DR, Burgers L, Bult P, Holland R. Three dimensional imaging of mammary ductal carcinoma in situ: clinical implications. Semin Diagn Pathol. 1994;11(3):193–8.
Warnberg F, Garmo H, Emdin S, et al. Effect of radiotherapy after breast-conserving surgery for ductal carcinoma in situ: 20 years follow-up in the randomized SweDCIS Trial. J Clin Oncol. 2014;32(32):3613–8.
Donker M, Litiere S, Werutsky G, et al. Breast-conserving treatment with or without radiotherapy in ductal carcinoma in situ: 15-year recurrence rates and outcome after a recurrence, from the EORTC 10853 randomized phase III trial. J Clin Oncol. 2013;31(32):4054–9.
Wapnir IL, Dignam JJ, Fisher B, et al. Long-term outcomes of invasive ipsilateral breast tumor recurrences after lumpectomy in NSABP B-17 and B-24 randomized clinical trials for DCIS. J Natl Cancer Inst. 2011;103(6):478–88.
Correa C, McGale P, Taylor C, et al. Overview of the randomized trials of radiotherapy in ductal carcinoma in situ of the breast. J Natl Cancer Inst Monogr. 2010;2010(41):162–77.
Azu M, Abrahamse P, Katz SJ, Jagsi R, Morrow M. What is an adequate margin for breast-conserving surgery? Surgeon attitudes and correlates. Ann Surg Oncol. 2010;17(2):558–63.
Morrow M, Van Zee KJ, Solin LJ, et al. Society of Surgical Oncology-American Society for Radiation Oncology-American Society of Clinical Oncology consensus guideline on margins for breast-conserving surgery with whole-breast irradiation in ductal carcinoma in situ. J Clin Oncol. 2016;34(33):4040–6.
Marinovich ML, Azizi L, Macaskill P, et al. The association of surgical margins and local recurrence in women with ductal carcinoma in situ treated with breast-conserving therapy: a meta-analysis. Ann Surg Oncol. 2016;23(12):3811–21.
Rosenberger LH, Mamtani A, Fuzesi S, et al. Early adoption of the SSO-ASTRO consensus guidelines on margins for breast-conserving surgery with whole-breast irradiation in stage I and II invasive breast cancer: initial experience from Memorial Sloan Kettering Cancer Center. Ann Surg Oncol. 2016;23(10):3239–46.
Chung A, Gangi A, Amersi F, Bose S, Zhang X, Giuliano A. Impact of consensus guidelines by the Society of Surgical Oncology and the American Society for Radiation Oncology on margins for breast-conserving surgery in stages 1 and 2 invasive breast cancer. Ann Surg Oncol. 2015;22(Suppl 3):S422–7.
Bhutiani N, Mercer MK, Bachman KC, et al. Evaluating the effect of margin consensus guideline publication on operative patterns and financial impact of breast cancer operation. J Am Coll Surg. 2018;227(1):6–11.
Havel L, Naik H, Ramirez L, Morrow M, Landercasper J. Impact of the SSO-ASTRO margin guideline on rates of re-excision after lumpectomy for breast cancer: a meta-analysis. Ann Surg Oncol. 2019;26(5):1238–44.
R Core Team (2019) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/. Accessed 3 Mar 2020.
Morrow M, Abrahamse P, Hofer TP, et al. Trends in reoperation after initial lumpectomy for breast cancer: addressing overtreatment in surgical management. JAMA Oncol. 2017;3(10):1352–7.
DeSnyder SM, Hunt KK, Dong W, et al. American Society of Breast Surgeons’ practice patterns after publication of the SSO-ASTRO-ASCO DCIS consensus guideline on margins for breast-conserving surgery with whole-breast irradiation. Ann Surg Oncol. 2018;25(10):2965–74.
Tadros AB, Smith BD, Shen Y, et al. Ductal carcinoma in situ and margins < 2 mm: contemporary outcomes with breast conservation. Ann Surg. 2019;269(1):150–7.
Langhans L, Jensen MB, Talman MM, Vejborg I, Kroman N, Tvedskov TF. Reoperation rates in ductal carcinoma in situ vs invasive breast cancer after wire-guided breast-conserving surgery. JAMA Surg. 2017;152(4):378–84.
Wilke LG, Czechura T, Wang C, et al. Repeat surgery after breast conservation for the treatment of stage 0 to II breast carcinoma: a report from the National Cancer Data Base, 2004–2010. JAMA Surg. 2014;149(12):1296–305.
Rutter CE, Park HS, Killelea BK, Evans SB. Growing use of mastectomy for ductal carcinoma-in situ of the breast among young women in the United States. Ann Surg Oncol. 2015;22(7):2378–86.
Park HL, Chang J, Lal G, Lal K, Ziogas A, Anton-Culver H. Trends in treatment patterns and clinical outcomes in young women diagnosed with ductal carcinoma in situ. Clin Breast Cancer. 2018;18(2):e179–85.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
The preparation of this manuscript was supported in part by NIH/NCI Cancer Center Support Grant No. P30 CA008748 to Memorial Sloan Kettering Cancer Center, and this study was accepted for presentation in ePoster format at the 2020 Society of Surgical Oncology International Conference on Surgical Cancer Care. Dr. Monica Morrow has received honoraria from Genomic Health, and all other authors have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mamtani, A., Romanoff, A., Baser, R. et al. Adoption of SSO-ASTRO Margin Guidelines for Ductal Carcinoma in Situ: What Is the Impact on Use of Additional Surgery?. Ann Surg Oncol 28, 295–302 (2021). https://doi.org/10.1245/s10434-020-08610-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-08610-7