Abstract
Background
Compared to open rectal surgery, laparoscopy is associated with lower perioperative morbidity but unclear oncologic outcomes. Unique technical challenges exist with laparoscopic rectal surgery and access based on geographical location is unknown. The purpose of this study was to determine whether proximity to colorectal fellowship training sites influences laparoscopy utilization for rectal cancer surgery.
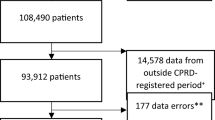
Methods
Population based retrospective spatial analysis assessing regional rates of laparoscopy use in patients (≥ 18 years of age) undergoing rectal cancer surgery in Canada (excluding Quebec) from April 2008 to March 2014.
Results
Overall, 11,261 patients underwent rectal cancer surgery. Four Canadian colorectal fellowship training centers were identified. Rectal surgeries were performed laparoscopically 27% of the time, and this significantly increased from 18.1 to 40.3% between 2008 and 2014. Multivariate analysis adjusting for province, disease, hospital, patient, and surgeon factors demonstrated that patients living within 25 km of a colorectal fellowship training site had 2.5 times higher odds of laparoscopy use and those living within 26–100 km had 1.8 times higher odds of laparoscopy [95% confidence interval (CI) 2.14–2.71, p < 0.001, 95% CI 1.64–2.07, p < 0.001 respectively]. High-volume surgeons and hospitals were associated with increased laparoscopy use (1.25, 95% CI 1.11–1.4 and 1.36, 95% CI 1.21–1.53, p < 0.001 respectively).
Conclusions
Significant geographical variation to laparoscopic rectal cancer surgery access in a publicly funded healthcare system currently exists. The inverse relationship between colorectal fellowship training site distance and undergoing a laparoscopic rectal surgery highlights the current disparities in Canadian health care and the need for surgical mentorship to increase uptake of advanced surgical techniques in rural neighbourhoods.

Similar content being viewed by others
References
Jacobs M, Verdeja JC, Goldstein HS. Minimally invasive colon resection (laparoscopic colectomy). Surg Laparosc Endosc. 1991;1(3):144–50.
Fowler DL, White SA. Laparoscopy-assisted sigmoid resection. Surg Laparosc Endosc. 1991;1(3):183–8.
Fleshman J, Branda M, Sargent DJ, et al. Effect of laparoscopic-assisted resection vs open resection of stage II or III rectal cancer on pathologic outcomes. JAMA. 2015;314(13):1346. https://doi.org/10.1001/jama.2015.10529
Stevenson ARL, Solomon MJ, Lumley JW, et al. Effect of laparoscopic-assisted resection vs open resection on pathological outcomes in rectal cancer. JAMA. 2015;314(13):1356. https://doi.org/10.1001/jama.2015.12009
Bonjer HJ, Deijen CL, Abis GA, et al. A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med. 2015;372(14):1324–32. https://doi.org/10.1056/nejmoa1414882
van der Pas MH, Haglind E, Cuesta MA, et al. Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol. 2013;14(3):210–8. https://doi.org/10.1016/s1470-2045(13)70016-0
Green BL, Marshall HC, Collinson F, et al. Long-term follow-up of the Medical Research Council CLASICC trial of conventional versus laparoscopically assisted resection in colorectal cancer. Br J Surg. 2013;100(1):75–82. https://doi.org/10.1002/bjs.8945
Jeong S-Y, Won Park J, Ho Nam B, et al. Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. 2014. https://doi.org/10.1016/s1470-2045(14)70205-0
Jamali FR, Soweid AM, Dimassi H, Bailey C, Leroy J, Marescaux J. Evaluating the degree of difficulty of laparoscopic colorectal surgery. Arch Surg. 2008;143(8):762. https://doi.org/10.1001/archsurg.143.8.762
Heald RJ. A new approach to rectal cancer. Br J Hosp Med. 1979;22:277–81.
Suwanabol P, Maykel J. Transanal total mesorectal excision: a novel approach to rectal surgery. Clin Colon Rectal Surg. 2017;30(02):120–9. https://doi.org/10.1055/s-0036-1597314
Luglio G, De Palma GD, Tarquini R, et al. Laparoscopic colorectal surgery in learning curve: role of implementation of a standardized technique and recovery protocol. A cohort study. Ann Med Surg. 2015;4(2):89–94. https://doi.org/10.1016/j.amsu.2015.03.003
Harling H, Bulow S, Moller LN, Jorgensen T. Hospital volume and outcome of rectal cancer surgery in Denmark 1994–99. Color Dis. 2005;7(1):90–5. https://doi.org/10.1111/j.1463-1318.2004.00751.x
Harinath G, Shah PR, Haray PN, Foster ME. Laparoscopic colorectal surgery in Great Britain and Ireland–where are we now? Colorectal Dis. 2005;7(1):86–9. https://doi.org/10.1111/j.1463-1318.2004.00682.x
Mavrantonis C, Wexner SD, Nogueras JJ, Weiss EG, Potenti F, Pikarsky AJ. Current attitudes in laparoscopic colorectal surgery. Surg Endosc Other Interv Tech. 2002;16(8):1152–7. https://doi.org/10.1007/s004640080072
Reames BN, Sheetz KH, Waits SA, Dimick JB, Regenbogen SE. Geographic variation in use of laparoscopic colectomy for colon cancer. J Clin Oncol. 2014;32(32):3667–72. https://doi.org/10.1200/jco.2014.57.1588
Gruber K, Soliman AS, Schmid K, Rettig B, Ryan J, Watanabe-Galloway S. Disparities in the utilization of laparoscopic surgery for colon cancer in rural Nebraska: a call for placement and training of rural general surgeons. J Rural Health. 2015;31(4):392–400. https://doi.org/10.1111/jrh.12120
Bardakcioglu O, Khan A, Aldridge C, Chen J. Growth of laparoscopic colectomy in the United States. Ann Surg. 2013;258(2):270–4. https://doi.org/10.1097/sla.0b013e31828faa66
Reames BN, Sheetz KH, Waits SA, Dimick JB, Regenbogen SE. Geographic variation in use of laparoscopic colectomy for colon cancer. J Clin Oncol. 2014;6:3667–72. https://doi.org/10.1200/jco.2014.57.1588
Doumouras AG, Saleh F, Eskicioglu C, Amin N, Cadeddu M, Hong D. Neighborhood variation in the utilization of laparoscopy for the treatment of colon cancer. Dis Colon Rectum. 2016;59(8):781–8. https://doi.org/10.1097/dcr.0000000000000600
Birkmeyer JD, Reames BN, McCulloch P, Carr AJ, Campbell WB, Wennberg JE. Understanding of regional variation in the use of surgery. Lancet. 2013;382(9898):1121–9. https://doi.org/10.1016/s0140-6736(13)61215-5
Canada S. Population estimates on July 1st, by age and sex. Table 17-10-0005-01.
Moloo H, Haggar F, Martel G, et al. The adoption of laparoscopic colorectal surgery: a national survey of general surgeons. Can J Surg. 2009;52(6):455–62.
Doumouras AG, Saleh F, Gmora S, Anvari M, Hong D. Regional variations in the public deliver y of bariatric surgery: an evaluation of the center of excellence model. Ann Surg. 2016. https://doi.org/10.1097/sla.0000000000001129
Doumouras AG, Anvari S, Cadeddu M, Anvari M, Hong D. Geographic variation in the provider of screening colonoscopy in Canada: a population-based cohort study. C Open. 2018. https://doi.org/10.9778/cmajo.20170131
Akhtar-Danesh GG, Doumouras AG, Flageole H, Hong D. Geographic and socioeconomic predictors of perforated appendicitis: a national Canadian cohort study. J Pediatric Surge. 2018.
Jeong S-Y, Park JW, Nam BH, et al. Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol. 2014;15(7):767–74. https://doi.org/10.1016/s1470-2045(14)70205-0
Fleshman J, Branda ME, Sargent DJ, et al. Disease-free survival and local recurrence for laparoscopic resection compared with open resection of stage II to III rectal cancer. Ann Surg. 2019;269(4):589–595. https://doi.org/10.1097/sla.0000000000003002
Stevenson ARL, Solomon MJ, Brown CSB, et al. Disease-free survival and local recurrence after laparoscopic-assisted resection or open resection for rectal cancer. Ann Surg. 2019;269(4):596–602. https://doi.org/10.1097/sla.0000000000003021
Fox J, Gross CP, Longo W, Reddy V. Laparoscopic colectomy for the treatment of cancer has been widely adopted in the United States. Dis Colon Rectum. 2012;55(5):501–8. https://doi.org/10.1097/dcr.0b013e318249ce5a
AlNasser M, Schneider EB, Gearhart SL, et al. National disparities in laparoscopic colorectal procedures for colon cancer. Surg Endosc. 2014;28(1):49–57. https://doi.org/10.1007/s00464-013-3160-8
Sanmartin C, Ross N. Experiencing difficulties accessing first-contact health services in Canada. Healthc Policy | Polit Santé. 2006;1(2):103–19. https://doi.org/10.12927/hcpol.2006.17882
Maddison AR, Asada Y, Urquhart R. Inequity in access to cancer care: a review of the Canadian literature. Cancer Causes Control. 2011;22(3):359–66. https://doi.org/10.1007/s10552-010-9722-3
Jarman BT, Cogbill TH, Mathiason MA, et al. Factors correlated with surgery resident choice to practice general surgery in a rural area. JSURG. 2009;66:319–24. https://doi.org/10.1016/j.jsurg.2009.06.003
Bennett CL, Stryker SJ, Ferreira MR, Adams J, Beart RW. The learning curve for laparoscopic colorectal surgery. Arch Surg. 1997;132(1):41. https://doi.org/10.1001/archsurg.1997.01430250043009
Borowski DW, Bradburn DM, Mills SJ, et al. Volume-outcome analysis of colorectal cancer-related outcomes. Br J Surg. 2010;97(9):1416. https://doi.org/10.1002/bjs.7111
Aquina CT, Probst CP, Becerra AZ, et al. High volume improves outcomes: the argument for centralization of rectal cancer surgery. Surgery. 2016;159(3):736–48. https://doi.org/10.1016/j.surg.2015.09.021
Lee DS, Stitt A, Wang X, et al. Administrative hospitalization database validation of cardiac procedure codes. Med Care. 2013;51(4):e22–6. https://doi.org/10.1097/mlr.0b013e3182329778
Canadian Institute for Health Information. Canadian MIS database-hospital financial performance indicators, 1999–2000 to 2009–2010, Methodological Notes. Ottawa; 2011.
Fowler A, Maclean A, Caycedo-Marulanda A, et al. Pan-Canadian standards for rectal cancer surgery—Canadian Partnership Against Cancer. Canadian Partnership Against Cancer. https://www.partnershipagainstcancer.ca/topics/rectal-cancer-surgical-standards/. Accessed 6 April 2019.
Acknowledgments
This study was presented as a podium presentation at the meeting of the American Society of Colon and Rectal Surgeons, Cleveland, OH, June 5, 2019.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Springer, J.E., Doumouras, A.G., Eskicioglu, C. et al. Regional Variation in the Utilization of Laparoscopy for the Treatment of Rectal Cancer: The Importance of Fellowship Training Sites. Ann Surg Oncol 27, 2478–2486 (2020). https://doi.org/10.1245/s10434-019-08115-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-08115-y