Abstract
Background
Complete mesocolic excision is becoming popular in colon cancer surgery in Western countries, and in the tumor-node-metastasis (TNM) classification of rectal cancer, a part of the lateral pelvic lymph nodes is classified as regional. However, the appropriateness of TNM staging according to the assessment of nodal status exclusively by extended lymphadenectomy remains unclear.
Patients and Methods
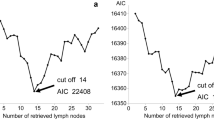
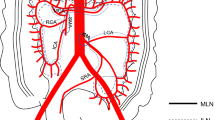
Using a nationwide multicenter database in Japan, we retrospectively analyzed 6866 patients with stage III colorectal cancer (CRC) treated with extended (D3) dissection. First, the best cutoff values for the number of metastatic nodes were explored. Second, the utility of the metastatic status of the main lymph nodes (i.e., at the origin of the feeding artery) and the lateral pelvic lymph nodes (“jN3” category in the Japanese staging system) as N staging criteria was evaluated. The modified N staging system that had the best risk stratification power was determined according to the Akaike information criterion (AIC).
Results
Excellent performance was noted when the number of metastatic nodes was categorized by cutoff values of “3/4” and “6/7.” Categorization of nodal metastasis was proven the most clinically efficacious when classified as modified-N1 (N1 and jN3-negative), modified-N2a (N2a and jN3-negative), and modified-N2b (N2b and/or jN3-positive; AIC, 22,810.8), rather than the classification based on the TNM (AIC, 22,849.2) or Japanese staging system (AIC, 22,811.1).
Conclusions
We structured a modified N staging system according to the number and extent of lymph node metastases. The modified system may be used in stage III cases for precise risk stratification.



Similar content being viewed by others
References
Astler VB, Coller FA. The prognostic significance of direct extension of carcinoma of the colon and rectum. Ann Surg. 1954; 139:846–52.
Gunderson LL, Sosin H. Areas of failure found at reoperation (second or symptomatic look) following “curative surgery” for adenocarcinoma of the rectum. Clinicopathologic correlation and implications for adjuvant therapy. Cancer. 1974; 34:1278–92.
Brierley JD, Gospodarowicz MK, Wittekind C, eds. TNM Classification of Malignant Tumors. 8th Edition. Hoboken: Wiley-Blackwell; 2017.
JSCCR. Japanese Classification of Colorectal Carcinoma Second English Edition ed. Tokyo: Kanehara; 2009.
Vaccaro CA, Bonadeo FA, Benati ML, et al. Colorectal cancer staging: reappraisal of N/PN classification. Dis Colon Rectum. 2004; 47:66–9.
Kendal WS. Lymph node-based prognostics: limitations with individualized cancer treatment. Am J Clin Oncol. 2006; 29:298–304.
Akagi Y, Fukushima T, Mizobe T, et al. Challenges in staging systems for colorectal cancer: clinical significance of metastatic lymph node number in colorectal cancer and mesorectal extension in rectal cancer. Digestion. 2010; 82:192–7.
Fukushima T, Akagi Y, Murakami H, et al. Estimation of the number of metastatic lymph nodes in Dukes’ C colorectal cancer. Anticancer Res. 2013; 33:2949–55.
Hermanek P, Guggenmoos-Holzmann I, Gall FP. Prognostic factors in rectal carcinoma. A contribution to the further development of tumor classification. Dis Colon Rectum. 1989; 32:593–9.
Wolmark N, Fisher B, Wieand HS. The prognostic value of the modifications of the Dukes’ C class of colorectal cancer. An analysis of the NSABP clinical trials. Ann Surg. 1986; 203:115–22.
Kobayashi H, Ueno H, Hashiguchi Y, Mochizuki H. Distribution of lymph node metastasis is a prognostic index in patients with stage III colon cancer. Surgery. 2006; 139:516–22.
Hida J, Okuno K, Yasutomi M, et al. Number versus distribution in classifying regional lymph node metastases from colon cancer. J Am Coll Surg. 2005; 201:217–22.
Newland RC, Dent OF, Lyttle MN, Chapuis PH, Bokey EL. Pathologic determinants of survival associated with colorectal cancer with lymph node metastases. A multivariate analysis of 579 patients. Cancer. 1994; 73:2076–82.
Shinto E, Hida J, Kobayashi H, et al. Prominent information of jN3-positive in stage III colorectal cancer removed by D3 dissection: retrospective analysis of 6866 patients from a multi-institutional database in Japan. Dis Colon Rectum. 2018; 61:447–53.
Watanabe T, Itabashi M, Shimada Y, et al. Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2014 for treatment of colorectal cancer. Int J Clin Oncol. 2015; 20:207–39.
Wang SJ, Lemieux A, Kalpathy-Cramer J, et al. Nomogram for predicting the benefit of adjuvant chemoradiotherapy for resected gallbladder cancer. J Clin Oncol. 2011; 29:4627–32.
Ueno H, Mochizuki H, Akagi Y, et al. Optimal colorectal cancer staging criteria in TNM classification. J Clin Oncol. 2012; 30:1519–26.
Akaike H. Information theory and extension of the maximum likelihood principle. In: Kotz S, Johnson NL, eds. Breakthroughs in Statistics Vol 1. Foundations and Basic Theory. New York: Springer-Verlag; 1973:610–24.
Fujita S, Akasu T, Mizusawa J, et al. Postoperative morbidity and mortality after mesorectal excision with and without lateral lymph node dissection for clinical stage II or stage III lower rectal cancer (JCOG0212): results from a multicentre, randomised controlled, non-inferiority trial. Lancet Oncol. 2012; 13:616–21.
Fujita S, Mizusawa J, Kanemitsu Y, et al. Mesorectal excision with or without lateral lymph node dissection for clinical stage II/III lower rectal cancer (JCOG0212): a multicenter, randomized controlled, noninferiority trial. Ann Surg. 2017; 266:201–7.
Gunderson LL, Jessup JM, Sargent DJ, Greene FL, Stewart AK. Revised TN categorization for colon cancer based on national survival outcomes data. J Clin Oncol. 2010; 28:264–71.
Ishihara S, Kawai K, Tanaka T, et al. Oncological outcomes of lateral pelvic lymph node metastasis in rectal cancer treated with preoperative chemoradiotherapy. Dis Colon Rectum. 2017; 60:469–76.
Kim HJ, Choi GS, Park JS, et al. Optimal treatment strategies for clinically suspicious lateral pelvic lymph node metastasis in rectal cancer. Oncotarget. 2017; 8:100724–33.
Acknowledgment
This work was supported by the Japanese Society for Cancer of the Colon and Rectum (JSCCR). We certify that we do not have any commercial associations that may pose a conflict of interest in connection with the submitted article.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Shinto, E., Hida, Ji., Ike, H. et al. A New N Staging System for Colorectal Cancer in the Era of Extended Lymphadenectomy. Ann Surg Oncol 25, 3891–3897 (2018). https://doi.org/10.1245/s10434-018-6786-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-018-6786-x