Abstract
Background
After radical resection of pancreatic ductal adenocarcinoma (PDAC), approximately 80% of patients will develop disease recurrence. It remains unclear to what extent the location of recurrence carries prognostic significance. Additionally, stratifying the pattern of recurrence may lead to a deeper understanding of the heterogeneous biological behavior of PDAC.
Objective
The aim of this study was to characterize the relationship of recurrence patterns with survival in patients with resected PDAC.
Methods
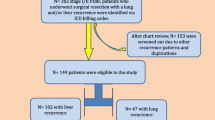
This single-center cohort study included patients undergoing pancreatectomy at the Johns Hopkins Hospital between 2000 and 2013. Exclusion criteria were neoadjuvant therapy and incomplete follow-up. Sites of first recurrence were stratified into five groups and survival outcomes were estimated using Kaplan–Meier curves. The association of specific recurrence locations with overall survival (OS) was analyzed using Cox proportional-hazards models with and without landmark analysis.
Results
Accurate follow-up data were available for 877 patients, 662 (75.5%) of whom had documented recurrence at last follow-up. Patients with multiple-site (n = 227, 4.7 months) or liver-only recurrence (n = 166, 7.2 months) had significantly worse median survival after recurrence when compared with lung- (n = 93) or local-only (n = 158) recurrence (15.4 and 9.7 months, respectively). On multivariable analysis, the unique recurrence patterns had variable predictive values for OS. Landmark analyses, with landmarks set at 12, 18, and 24 months, confirmed these findings.
Conclusions
This study demonstrates that specific patterns of PDAC recurrence result in different survival outcomes. Furthermore, distinct first recurrence locations have unique independent predictive values for OS, which could help with prognostic stratification and decisions regarding treatment after the diagnosis of recurrence.


Similar content being viewed by others
References
Rahib L, Smith BD, Aizenberg R, Rosenzweig AB, Fleshman JM, Matrisian LM. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. 2014;74:2913–21.
Riall TS, Cameron JL, Lillemoe KD, Winter JM, Campbell KA, Hruban RH, et al. Resected periampullary adenocarcinoma: 5-year survivors and their 6- to 10-year follow-up. Surgery. 2006;140:764–72.
Cameron JL, Riall TS, Coleman J, Belcher KA. One thousand consecutive pancreaticoduodenectomies. Ann Surg. 2006;244:10–15.
Cameron JL, He J. Two thousand consecutive pancreaticoduodenectomies. J Am Coll Surg. 2015;220:530–6.
Sperti C, Pasquali C, Piccoli A, Pedrazzoli S. Recurrence after resection for ductal adenocarcinoma of the pancreas. World J Surg. 1997;21:195–200.
Van den Broeck A, Sergeant G, Ectors N, Van Steenbergen W, Aerts R, Topal B. Patterns of recurrence after curative resection of pancreatic ductal adenocarcinoma. Eur J Surg Oncol. 2009;35:600–4.
Hernandez JM, Morton CA, Al-Saadi S, Villadolid D, Cooper J, Bowers C, et al. The natural history of resected pancreatic cancer without adjuvant chemotherapy. Am Surg. 2010;76:480–5.
Suenaga M, Fujii T, Kanda M, Takami H, Okumura N, Inokawa Y, et al. Pattern of first recurrent lesions in pancreatic cancer: hepatic relapse is associated with dismal prognosis and portal vein invasion. Hepatogastroenterology. 2014;61:1756–61.
Groot VP, Daamen LA, Hagendoorn J, Borel Rinkes IHM, van Santvoort HC, Molenaar IQ. Use of imaging during symptomatic follow-up after resection of pancreatic ductal adenocarcinoma. J Surg Res. 2018;221:152–60.
Groot VP, Rezaee N, Wu W, Cameron JL, Fishman EK, Hruban RH, et al. Patterns, timing, and predictors of recurrence following pancreatectomy for pancreatic ductal adenocarcinoma. Ann Surg. 2018;267:936–45.
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187–96.
Anderson JR, Cain KC, Gelber RD. Analysis of survival by tumor response. J Clin Oncol. 1983;1:710–9.
Weeden S, Grimer RJ, Cannon SR, Taminiau AH, Uscinska BM. The effect of local recurrence on survival in resected osteosarcoma. Eur J Cancer. 2001;37:39–46.
Dafni U. Landmark analysis at the 25-year landmark point. Circ Cardiovasc Qual Outcomes. 2011;4:363–71.
Hallet J, Sa Cunha A, Adam R, Goéré D, Bachellier P, Azoulay D, et al. Factors influencing recurrence following initial hepatectomy for colorectal liver metastases. Br J Surg. 2016;103:1366–76.
Groot VP, Gemenetzis G, Blair AB, Rivero-Soto RJ, Yu J, Javed AA, et al. Defining and predicting early recurrence in 957 Patients with resected pancreatic ductal adenocarcinoma. Ann Surg. Epub 23 Mar 2018. https://doi.org/10.1097/sla.0000000000002734.
Tani M, Kawai M, Miyazawa M, Hirono S, Ina S, Nishioka R, et al. Liver metastasis as an initial recurrence has no impact on the survival of patients with resectable pancreatic adenocarcinoma. Langenbecks Arch Surg. 2009;394:249–53.
Zhang Y, Frampton AE, Kyriakides C, Bong, J.J., Habib, N., Ahmad, R, et al. Loco-recurrence after resection for ductal adenocarcinoma of the pancreas: predictors and implications for adjuvant chemoradiotherapy. J Cancer Res Clin Oncol. 2012;138:1063–71.
Groot VP, van Santvoort HC, Rombouts SJE, Hagendoorn J, Borel Rinkes IH, van Vulpen M, et al. Systematic review on the treatment of isolated local recurrence of pancreatic cancer after surgery; re-resection, chemoradiotherapy and SBRT. HPB (Oxford). 2017;19:83–92.
Ryan JF, Groot VP, Rosati LM, Hacker-Prietz A, Narang AK, McNutt TR, et al. Stereotactic body radiation therapy for isolated local recurrence after surgical resection of pancreatic ductal adenocarcinoma appears to be safe and effective. Ann Surg Oncol. 2018;25:280–89.
Arnaoutakis GJ, Rangachari D, Laheru DA, Iacobuzio-Donahue CA, Hruban RH, Herman JM, et al. Pulmonary resection for isolated pancreatic adenocarcinoma metastasis: an analysis of outcomes and survival. J Gastrointest Surg. 2011;15:1611–7.
Downs-Canner S, Zenati M, Boone BA, Varley PR, Steve J, Hogg ME, et al. The indolent nature of pulmonary metastases from ductal adenocarcinoma of the pancreas. J Surg Oncol. 2015;112:80–85.
Wangjam T, Zhang Z, Zhou XC, Lyer L, Faisal F, Soares KC, et al. Resected pancreatic ductal adenocarcinomas with recurrence limited in lung have a significantly better prognosis than those with other recurrence patterns. Oncotarget. 2015;6:36903–10.
Lu F, Poruk KE, Weiss MJ. Surgery for oligometastasis of pancreatic cancer. Chin J Cancer Res. 2015;27:358–67.
Yamashita K, Miyamoto A, Hama N, Asaoka T, Maeda S, Omiya H, et al. Survival impact of pulmonary metastasis as recurrence of pancreatic ductal adenocarcinoma. Dig Surg. 2015;32:464–71.
Zheng B, Ohuchida K, Yan Z, Okumura T, Ohtsuka T, Nakamura M. Primary recurrence in the lung is related to favorable prognosis in patients with pancreatic cancer and postoperative recurrence. World J Surg. 2017;41: 2858–66.
Poruk KE, Kim Y, Cameron JL, He J, Eckhauser FE, Rezaee N, et al. What is the significance of indeterminate pulmonary nodules in patients undergoing resection for pancreatic adenocarcinoma? J Gastrointest Surg. 2015;19:841–47.
Acknowledgement
The authors would like to thank the Foundation “De Drie Lichten”, Prins Bernhard Cultuurfonds, VSBfonds, Prof. Michaël-van Vloten Fonds, Nijbakker-Morra Foundation, and the Living With Hope Foundation (all from The Netherlands) for funding this study in the form of grants for a research fellowship by VPG.
Disclosures
Vincent P. Groot, Georgios Gemenetzis, Alex B. Blair, Ding Ding, Ammar A. Javed, Richard A. Burkhart, Jun Yu, Inne H. Borel Rinkes, I. Quintus Molenaar, John L. Cameron, Elliot K. Fishman, Ralph H. Hruban, Matthew J. Weiss, Christopher L. Wolfgang, and Jin He have no financial disclosures or conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Groot, V.P., Gemenetzis, G., Blair, A.B. et al. Implications of the Pattern of Disease Recurrence on Survival Following Pancreatectomy for Pancreatic Ductal Adenocarcinoma. Ann Surg Oncol 25, 2475–2483 (2018). https://doi.org/10.1245/s10434-018-6558-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-018-6558-7