Abstract
Purpose
Tumor stage and distinct histological subtypes in epithelial ovarian cancer (EOC) show different prognostic outcome. The aim of this study is to evaluate whether the frequency of lymph node (LN) metastases in patients with different tumor stages and histological subtypes undergoing systematic pelvic and paraaortic lymphadenectomy is coincidentally divergent.
Methods
Patients with EOC treated with upfront staging or debulking surgery between January 2000 and December 2016 were included. Systematic lymphadenectomy was performed in all consecutive patients with optimal debulking and without medical contraindications.
Results
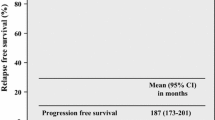
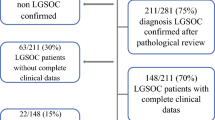
Seven hundred sixty-two patients including 27.2% with early-stage EOC were included. The median number of removed LNs was 69, and metastases to LNs were found in 54.7%. No LN metastases were found in patients with low-grade endometrioid carcinoma, independently of tumor stage. LN metastases in early-stage low-grade serous (N = 5), mucinous (N = 31), and clear cell (N = 28) EOC were found in one (20%), zero, and one (3.6%) patient, respectively. LN metastases were detected in more than 10% of patients with all other histological subtypes. On multivariate analyses, overall survival was significantly impaired in patients with LN metastases, as compared with patients without LN metastases (p = 0.001).
Conclusions
The risk of LN metastases in patients with EOC is dependent on stage and histological subtype. Patients with incidental finding of early mucinous or low-grade endometrioid EOC are at very low risk of retroperitoneal lymph node metastases. Reoperation for lymph node staging only should be discussed individually with caution.




Similar content being viewed by others

References
DeSantis CE, Lin CC, Mariotto AB, Siegel RL, Stein KD, Kramer JL, Alteri R, Robbins AS, Jemal A. Cancer treatment and survivorship statistics, 2014. CA: A Cancer J Clin. 2014;64(4):252-71.
Heintz AP, Odicino F, Maisonneuve P, Quinn MA, Benedet JL, Creasman WT, et al. Carcinoma of the ovary. FIGO 26th annual report on the results of treatment in gynecological cancer. Int J Gynaecol Obstet. 2006;PMID: 17161157.
Rochon J, du Bois A. Clinical research in epithelial ovarian cancer and patients’ outcome. Ann Oncol. 2011;PMID: 22039139.
du Bois A, Reuss A, Pujade-Lauraine E, Harter P, Ray-Coquard I, Pfisterer J (2009) Role of surgical outcome as prognostic factor in advanced epithelial ovarian cancer: a combined exploratory analysis of 3 prospectively randomized phase 3 multicenter trials: by the Arbeitsgemeinschaft Gynaekologische Onkologie Studiengruppe Ovarialkarzinom (AGO-OVAR) and the Groupe d’Investigateurs Nationaux Pour les Etudes des Cancers de l’Ovaire (GINECO). Cancer. 2009;115(6):1234-44.
Malpica A, Deavers MT, Lu K, Bodurka DC, Atkinson EN, Gershenson DM, et al. Grading ovarian serous carcinoma using a two-tier system. Am J Surg Pathol. 2004;28(4):496-504.
Shih Ie M, Kurman RJ. Ovarian tumorigenesis: a proposed model based on morphological and molecular genetic analysis. Am J Pathol. 2004;164(5):1511-8.
Wiegand KC, Shah SP, Al-Agha OM, Zhao Y, Tse K, Zeng T, et al. ARID1A mutations in endometriosis-associated ovarian carcinomas. N Engl J Med. 2010;363(16):1532-43.
Mackay HJ, Brady MF, Oza AM, Reuss A, Pujade-Lauraine E, Swart AM, et al. Prognostic relevance of uncommon ovarian histology in women with stage III/IV epithelial ovarian cancer. Int J Gynecol Cancer. 2010;20(6):945-52.
Heitz F, Harter P, Alesina PF, Walz MK, Lorenz D, Groeben H, et al. Pattern of and reason for postoperative residual disease in patients with advanced ovarian cancer following upfront radical debulking surgery. Gynecol Oncol. 2016;141(2):264-70.
Fotopoulou C, El-Balat A, du Bois A, Sehouli J, Harter P, Muallem MZ, et al. Systematic pelvic and paraaortic lymphadenectomy in early high-risk or advanced endometrial cancer. Arch Gynecol Obste. 2015;292(6):1321-7.
Harter P, Gnauert K, Hils R, Lehmann TG, Fisseler-Eckhoff A, Traut A, et al. Pattern and clinical predictors of lymph node metastases in epithelial ovarian cancer. Int J Gynecol Cancer. 2007;17(6):1238-44.
Ataseven B, Grimm C, Harter P, Prader S, Traut A, Heitz F, et al. Prognostic value of lymph node ratio in patients with advanced epithelial ovarian cancer. Gynecol Oncol. 2014;135(3):435-40.
Morice P, Joulie F, Camatte S, Atallah D, Rouzier R, Pautier P, et al. Lymph node involvement in epithelial ovarian cancer: analysis of 276 pelvic and paraaortic lymphadenectomies and surgical implications. J Am Coll Surg. 2003;197(2):198-205.
Burghardt E, Girardi F, Lahousen M, Tamussino K, Stettner H. Patterns of pelvic and paraaortic lymph node involvement in ovarian cancer. Gynecol Oncol. 1991;40(2):103-6.
Minig L, Heitz F, Cibula D, Bakkum-Gamez JN, Germanova A, Dowdy SC, et al. Patterns of lymph node metastases in apparent stage I low-grade epithelial ovarian cancer: a multicenter study. Ann Surg Oncol. 2017;24(9):2720-2726.
Rosso M, Majem B, Devis L, Lapyckyj L, Besso MJ, Llaurado M, et al. E-cadherin: A determinant molecule associated with ovarian cancer progression, dissemination and aggressiveness. PloS One. 2017;12(9):e0184439.
Trillsch F, Kuerti S, Eulenburg C, Burandt E, Woelber L, Prieske K, et al. E-Cadherin fragments as potential mediators for peritoneal metastasis in advanced epithelial ovarian cancer. Br J Cancer. 2016;114(2):213-20.
Kommoss S, Gilks CB, du Bois A, Kommoss F. Ovarian carcinoma diagnosis: the clinical impact of 15 years of change. Br J Cancer. 2016;115(8):993-9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
No relevant commercial interest or financial support to be disclosed.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Heitz, F., Harter, P., Ataseven, B. et al. Stage- and Histologic Subtype-Dependent Frequency of Lymph Node Metastases in Patients with Epithelial Ovarian Cancer Undergoing Systematic Pelvic and Paraaortic Lymphadenectomy. Ann Surg Oncol 25, 2053–2059 (2018). https://doi.org/10.1245/s10434-018-6412-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-018-6412-y