Abstract
Background
The role of N classification is controversial in several prognostication systems proposed for pancreatic neuroendocrine neoplasms (pNENs). The widely accepted modified European Neuroendocrine Tumor Society (mENETS) system suggests this contradiction may be related to T classification.
Methods
Data were collected retrospectively from 981 patients in the Surveillance, Epidemiology, and End Results (SEER) database (1973–2012; cohort 1) and 140 patients from the Pancreatic Cancer Institute of Fudan University (2006–2016; cohort 2). All patients had resected well- to moderately differentiated locoregional pNENs, whereby the mENETS system was adopted. Factors related to N1 classification and the association between N and T classifications were analyzed, and N classification prognosis based on T classification was assessed.
Results
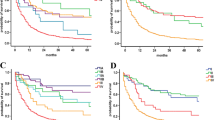
In cohorts 1 and 2, tumor size (2–4 cm: p < 0.001 and p = 0.037, respectively; > 4 cm: p < 0.001 and p = 0.012, respectively) and tumors extending beyond the pancreas (p < 0.001 and p = 0.016, respectively), which are factors for T classification, affected N1 classification. For tumors limited to the pancreas, the N1 classification was associated with tumor size (p < 0.001 and p = 0.046, respectively) and predicted poor disease-specific survival (DSS), while for tumors extending beyond the pancreas, the N1 classification did not affect patient outcomes. Findings obtained with data from the SEER database were reproducible with our institutional data.
Conclusions
N classification is associated with T classification, limiting the value of N1 classification for the pNENs tumor-node-metastasis system. A new risk model is necessary to predict patient outcomes and guide clinical practice for the prognosis of pNENs.


Similar content being viewed by others
References
Yao JC, Hassan M, Phan A, et al. One hundred years after “carcinoid”: epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol. 2008; 26(18): 3063–72.
Ricci C, Casadei R, Taffurelli G, et al. The role of lymph node ratio in recurrence after curative surgery for pancreatic endocrine tumours. Pancreatology. 2013; 13(6): 589–93.
Bettini R, Boninsegna L, Mantovani W, et al. Prognostic factors at diagnosis and value of WHO classification in a mono-institutional series of 180 non-functioning pancreatic endocrine tumours. Ann Oncol. 2008; 19(5): 903–8.
Ballian N, Loeffler AG, Rajamanickam V, Norstedt PA, Weber SM, Cho CS. A simplified prognostic system for resected pancreatic neuroendocrine neoplasms. HPB (Oxford). 2009; 11(5): 422-8.
Scarpa A, Mantovani W, Capelli P, et al. Pancreatic endocrine tumors: improved TNM staging and histopathological grading permit a clinically efficient prognostic stratification of patients. Mod Pathol. 2010; 23(6): 824-33.
Haynes AB, Deshpande V, Ingkakul T, et al. Implications of incidentally discovered, nonfunctioning pancreatic endocrine tumors: short-term and long-term patient outcomes. Arch Surg. 2011; 146(5): 534-8.
Tsutsumi K, Ohtsuka T, Mori Y, et al. Analysis of lymph node metastasis in pancreatic neuroendocrine tumors (PNETs) based on the tumor size and hormonal production. J Gastroenterol. 2012; 47(6): 678-85.
Krampitz GW, Norton JA, Poultsides GA, Visser BC, Sun L, Jensen RT. Lymph nodes and survival in pancreatic neuroendocrine tumors. Arch Surg. 2012; 147(9): 820-7.
Boninsegna L, Panzuto F, Partelli S, et al. Malignant pancreatic neuroendocrine tumour: lymph node ratio and Ki67 are predictors of recurrence after curative resections. Eur J Cancer. 2012; 48(11): 1608-15.
Partelli S, Gaujoux S, Boninsegna L, et al. Pattern and clinical predictors of lymph node involvement in nonfunctioning pancreatic neuroendocrine tumors (NF-PanNETs). JAMA Surg. 2013; 148(10): 932-9.
Toste PA, Kadera BE, Tatishchev SF, et al. Nonfunctional pancreatic neuroendocrine tumors <2 cm on preoperative imaging are associated with a low incidence of nodal metastasis and an excellent overall survival. J Gastrointest Surg. 2013; 17(12): 2105-13.
Hashim YM, Trinkaus KM, Linehan DC, et al. Regional lymphadenectomy is indicated in the surgical treatment of pancreatic neuroendocrine tumors (PNETs). Ann Surg. 2014; 259(2): 197-203.
Curran T, Pockaj BA, Gray RJ, Halfdanarson TR, Wasif N. Importance of lymph node involvement in pancreatic neuroendocrine tumors: impact on survival and implications for surgical resection. J Gastrointest Surg. 2015; 19(1): 152-60; discussion 160.
Postlewait LM, Ethun CG, Baptiste GG, et al. Pancreatic neuroendocrine tumors: Preoperative factors that predict lymph node metastases to guide operative strategy. J Surg Oncol. 2016; 114(4): 440-5.
Conrad C, Kutlu OC, Dasari A, et al. Prognostic Value of Lymph Node Status and Extent of Lymphadenectomy in Pancreatic Neuroendocrine Tumors Confined To and Extending Beyond the Pancreas. J Gastrointest Surg. 2016; 20(12): 1966-1974.
Madeira I, Terris B, Voss M, et al. Prognostic factors in patients with endocrine tumours of the duodenopancreatic area. Gut. 1998; 43(3): 422-7.
Bilimoria KY, Talamonti MS, Tomlinson JS, et al. Prognostic score predicting survival after resection of pancreatic neuroendocrine tumors: analysis of 3851 patients. Ann Surg. 2008; 247(3): 490-500.
Franko J, Feng W, Yip L, Genovese E, Moser AJ. Non-functional neuroendocrine carcinoma of the pancreas: incidence, tumor biology, and outcomes in 2,158 patients. J Gastrointest Surg. 2010; 14(3): 541-8.
Poultsides GA, Huang LC, Chen Y, et al. Pancreatic neuroendocrine tumors: radiographic calcifications correlate with grade and metastasis. Ann Surg Oncol. 2012; 19(7): 2295-303.
Kuo EJ, Salem RR. Population-level analysis of pancreatic neuroendocrine tumors 2 cm or less in size. Ann Surg Oncol. 2013; 20(9): 2815-21.
Cherenfant J, Stocker SJ, Gage MK, et al. Predicting aggressive behavior in nonfunctioning pancreatic neuroendocrine tumors. Surgery. 2013; 154(4): 785-91; discussion 791-3.
Wong J, Fulp WJ, Strosberg JR, Kvols LK, Centeno BA, Hodul PJ. Predictors of lymph node metastases and impact on survival in resected pancreatic neuroendocrine tumors: a single-center experience. Am J Surg. 2014; 208(5): 775-80.
Teo R, Goh BK, Tai DW, et al. Validation and comparison between current prognostication systems for pancreatic neuroendocrine neoplasms: a single-institution experience with 176 patients. Surgery. 2017;161(5):1235–1245.
Ferrone CR, Tang LH, Tomlinson J, et al. Determining prognosis in patients with pancreatic endocrine neoplasms: can the WHO classification system be simplified. J Clin Oncol. 2007; 25(35): 5609-15.
Gebauer N, Schmidt-Werthern C, Bernard V, et al. Genomic landscape of pancreatic neuroendocrine tumors. World J Gastroenterol. 2014; 20(46): 17498-506.
Liu TC, Hamilton N, Hawkins W, Gao F, Cao D. Comparison of WHO Classifications (2004, 2010), the Hochwald grading system, and AJCC and ENETS staging systems in predicting prognosis in locoregional well-differentiated pancreatic neuroendocrine tumors. Am J Surg Pathol. 2013; 37(6): 853-9.
Luo G, Javed A, Strosberg JR, et al. Modified Staging Classification for Pancreatic Neuroendocrine Tumors on the Basis of the American Joint Committee on Cancer and European Neuroendocrine Tumor Society Systems. J Clin Oncol. 2017; 35(3): 274-280.
Parekh JR, Wang SC, Bergsland EK, et al. Lymph node sampling rates and predictors of nodal metastasis in pancreatic neuroendocrine tumor resections: the UCSF experience with 149 patients. Pancreas. 2012; 41(6): 840-4.
Neuroendocrine tumors. Version 2. 2017. NCCN Clinical Practice Guidelines in Oncology. Available at: http://www.nccn.org/professionals/physician_gls/pdf/neuroendocrine.pdf. Accessed 29 Mar 2017.
Panzuto F, Boninsegna L, Fazio N, et al. Metastatic and locally advanced pancreatic endocrine carcinomas: analysis of factors associated with disease progression. J Clin Oncol. 2011; 29(17): 2372-7.
Jin K, Luo G, Xu J, et al. Clinical outcomes and prognostic factors of resected pancreatic neuroendocrine neoplasms: a single-center experience in China. Oncol Lett. 2017; 13(5): 3163-3168.
Partelli S, Gaujoux S, Boninsegna L, et al. Pattern and clinical predictors of lymph node involvement in nonfunctioning pancreatic neuroendocrine tumors (NF-PanNETs). JAMA Surg. 2013; 148(10): 932-9.
Tol JA, Gouma DJ, Bassi C, et al. Definition of a standard lymphadenectomy in surgery for pancreatic ductal adenocarcinoma: a consensus statement by the International Study Group on Pancreatic Surgery (ISGPS). Surgery. 2014; 156(3): 591-600.
Disclosures
Jin-Zhi Xu, Wen-Quan Wang, Shi-Rong Zhang, Hua-Xiang Xu, Chun-Tao Wu, Zi-Hao Qi, He-Li Gao, Quan-Xing Ni, Liang Liu, and Xian-Jun Yu declare no conflicts of interest.
Funding
This research was supported by the National Natural Science Foundation of China (81402397, 81472670, 81402398, and 81172005), the National Natural Science Foundation of Shanghai (14ZR1407600), and the “Yang-Fan” Plan for Young Scientists of Shanghai (14YF1401100).
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Xu, JZ., Wang, WQ., Zhang, SR. et al. Intrinsic Contact Between T and N Classifications in Resected Well–Moderately Differentiated Locoregional Pancreatic Neuroendocrine Neoplasms. Ann Surg Oncol 25, 647–654 (2018). https://doi.org/10.1245/s10434-017-6289-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-017-6289-1