Abstract
Background
The American College of Surgeons Oncology Group (ACOSOG) Z0011 trial established the safety of omitting axillary lymph node dissection (ALND) for early-stage breast cancer patients with limited nodal disease undergoing lumpectomy. We examined the extent of axillary surgery among women eligible for Z0011 based on patient age and tumor subtype.
Methods
Patients with cT1–2, cN0 breast cancers and one or two positive nodes diagnosed from 2009 to 2014 and treated with lumpectomy were identified in the National Cancer Data Base. Sentinel lymph node biopsy (SLNB) was defined as the removal of 1–5 nodes and ALND as the removal of 10 nodes or more. Tumor subtype was categorized as luminal, human epidermal growth factor 2-positive (HER2+), or triple-negative. Logistic regression was used to estimate the odds of receiving SLNB alone versus ALND.
Results
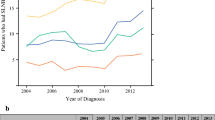
The inclusion criteria were met by 28,631 patients (21,029 SLNB-alone and 7602 ALND patients). Patients 70 years of age or older were more likely to undergo SLNB alone than ALND (27.0% vs 20.1%; p < 0.001). The radiation therapy use rate was 89.4% after SLNB alone and 89.7% after ALND. In the multivariate analysis, the uptake of Z0011 recommendations increased over time (2014 vs 2009: odds ratio [OR] 13.02; p < 0.001). Younger patients were less likely to undergo SLNB alone than older patients (age <40 vs ≥70: OR 0.59; p < 0.001). Patients with HER2+ (OR 0.89) or triple-negative disease (OR 0.79) (p < 0.001) were less likely to undergo SLNB alone than those with luminal subtypes.
Conclusions
Among women potentially eligible for ACOSOG Z0011, the use of SLNB alone increased over time in all groups, but the extent of axillary surgery differed by patient age and tumor subtype.

Similar content being viewed by others
References
Giuliano AE, Kirgan DM, Guenther JM, et al. Lymphatic mapping and sentinel lymphadenectomy for breast cancer. Ann Surg. 1994;220:391–8 (Discussion 398–401).
Krag DN, Anderson SJ, Julian TB, et al. Sentinel lymph node resection compared with conventional axillary lymph node dissection in clinically node-negative patients with breast cancer: overall survival findings from the NSABP B-32 randomised phase 3 trial. Lancet Oncol. 2010;11:927–33.
Purushotham AD, Upponi S, Klevesath MB, et al. Morbidity after sentinel lymph node biopsy in primary breast cancer: results from a randomized controlled trial. J Clin Oncol. 2005;23:4312–21.
Giuliano AE, McCall L, Beitsch P, et al. Locoregional recurrence after sentinel lymph node dissection with or without axillary dissection in patients with sentinel lymph node metastases: the American College of Surgeons Oncology Group Z0011 randomized trial. Ann Surg. 2010;252:426–32 (Discussion 432–3).
Giuliano AE, Ballman K, McCall L, et al. Locoregional recurrence after sentinel lymph node dissection with or without axillary dissection in patients with sentinel lymph node metastases: long-term follow-up from the American College of Surgeons Oncology Group (Alliance) ACOSOG Z0011 Randomized Trial. Ann Surg. 2016;264:413–20.
NCCN. NCCN Clinical Practice Guidelines in Oncology: Breast Cancer Version 2, 2016. http://www.nccn.org/professionals/physician_gls/pdf/breast.pdf. Accessed May 2017.
Lyman GH, Temin S, Edge SB, et al. Sentinel lymph node biopsy for patients with early-stage breast cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2014;32:1365–83.
Surgeons ASoB. Performance and Practice Guidelines for Axillary Lymph Node Dissection in Breast Cancer Patients. https://www.breastsurgeons.org/statements/guidelines/PerformancePracticeGuidelines_ALND.pdf. Accessed May 2017.
Bilimoria KY, Bentrem DJ, Hansen NM, et al. Comparison of sentinel lymph node biopsy alone and completion axillary lymph node dissection for node-positive breast cancer. J Clin Oncol. 2009;27:2946–53.
Caudle AS, Hunt KK, Tucker SL, et al. American College of Surgeons Oncology Group (ACOSOG) Z0011: impact on surgeon practice patterns. Ann Surg Oncol. 2012;19:3144–51.
Mamtani A, Patil S, Van Zee KJ, et al. Age and receptor status do not indicate the need for axillary dissection in patients with sentinel lymph node metastases. Ann Surg Oncol. 2016;23:3481–6.
Bland KI, Scott-Conner, C. E., Menck, H., et al. Axillary dissection in breast-conserving surgery for stage I and II breast cancer: a National Cancer Data Base study of patterns of omission and implications for survival. J Am Coll Surg. 1999;188:586–95 (Discussion 595–6).
Enger SM, Thwin SS, Buist DS, et al. Breast cancer treatment of older women in integrated health care settings. J Clin Oncol. 2006;24:4377–83.
Freedman RA, Partridge AH. Management of breast cancer in very young women. Breast. 2013;22(Suppl 2):S176–9.
Lee HB, Han W. Unique features of young age breast cancer and its management. J Breast Cancer. 2014;17:301–7.
Chollet-Hinton L, Anders CK, Tse CK, et al. Breast cancer biologic and etiologic heterogeneity by young age and menopausal status in the Carolina Breast Cancer Study: a case-control study. Breast Cancer Res. 2016;18:79.
Gartner R, Jensen MB, Kronborg L, et al. Self-reported arm-lymphedema and functional impairment after breast cancer treatment: a nationwide study of prevalence and associated factors. Breast. 2010;19:506–15.
Chung A, Gangi A, Mirocha J, et al. Applicability of the ACOSOG Z0011 criteria in women with high-risk node-positive breast cancer undergoing breast conserving surgery. Ann Surg Oncol. 2015;22:1128–32.
King TA, Morrow M. Surgical issues in patients with breast cancer receiving neoadjuvant chemotherapy. Nat Rev Clin Oncol. 2015;12:335–43.
Mohiuddin JJ, Deal AM, Carey LA, et al. Neoadjuvant systemic therapy use for younger patients with breast cancer treated in different types of cancer centers across the United States. J Am Coll Surg. 2016;223:717–728 e4.
Disclosure
There are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ong, C.T., Thomas, S.M., Blitzblau, R.C. et al. Patient Age and Tumor Subtype Predict the Extent of Axillary Surgery Among Breast Cancer Patients Eligible for the American College of Surgeons Oncology Group Trial Z0011. Ann Surg Oncol 24, 3559–3566 (2017). https://doi.org/10.1245/s10434-017-6075-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-017-6075-0



