Abstract
Background
Hospitalization is associated with negative clinical effects that last beyond discharge. This study aimed to determine whether hospitalization in the year before major oncologic surgery is associated with adverse outcomes.
Methods
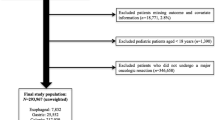
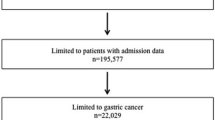
Patients 18 years of age or older with stomach, pancreas, colon, or rectal cancer who underwent resection in California and New York (2008–2010) were included in the study. Patients with hospitalization in the year prior to oncologic resection (HYPOR) were identified. Multivariable logistic regression was used to examine the association of prior hospitalization with the following adverse outcomes: inpatient mortality, complications, complex discharge needs, and 90-day readmission. Subset analysis by cancer type was performed. Outcomes based on temporal proximity of hospitalization to month of surgical admission were evaluated.
Results
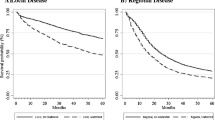
Of 32,292 patients, 16.3% (n = 5276) were HYPOR. Patients with prior hospitalization were older (median age, 72 vs 67 years; p < 0.001) and had more comorbidities (Elixhauser Index ≥3, 86.5 vs 75.3%; p < 0.001). In the multivariable analysis, HYPOR was associated with complications (odds ratio [OR], 1.28; 95% confidence interval [CI] 1.18–1.40), complex discharge (OR, 1.44; 95% CI 1.34–1.55), and 90-day readmission (OR, 1.45; 95% CI 1.35–1.56). The interval from HYPOR to resection was not associated with adverse outcomes.
Conclusions
Patients hospitalized in the year before oncologic resection are at increased risk for postoperative adverse events. Recent hospitalization is a risk factor that is easily ascertainable and should be used by clinicians to identify patients who may need additional support around the time of oncologic resection.

Similar content being viewed by others
References
Krumholz HM. Post-hospital syndrome: an acquired, transient condition of generalized risk. N Engl J Med. 2013;368:100–2.
Detsky AS, Krumholz HM. Reducing the trauma of hospitalization. JAMA. 2014;311:2169–70.
Dharmarajan K, Hsieh AF, Kulkarni VT, Lin Z, Ross JS, Horwitz LI, et al. Trajectories of risk after hospitalization for heart failure, acute myocardial infarction, or pneumonia: retrospective cohort study. BMJ. 2015;350:h411.
Brownlee SA, Blackwell RH, Blanco BA, Zapf MA, Kliethermes S, Gupta GN, et al. Impact of post-hospital syndrome on outcomes following elective, ambulatory surgery. Ann Surg. 2017;266(2):274–9.
California State Inpatient Database (SID). Healthcare Cost and Utilization Project (HCUP). Rockville, MD: Agency for Healthcare Research and Quality. Retrieved 10 April 2017 at www.hcup-us.ahrq.gov/db/state/siddbdocumentation.jsp.
Bureau of Health Informatics. Office of Quality and Health Safety. Statewide Planning and Research Cooperative System (SPARCS). Albany: New York State Department of Health; 2016. Retrieved 10 April 2017 at https://www.health.ny.gov/statistics/sparcs/.
Centers for Medicare & Medicaid Services. ICD-9-CM diagnosis and procedure codes: abbreviated and full code titles. Retrieved 10 April 2017 at http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes.html.
HCUP CCS. Healthcare Cost and Utilization Project (HCUP). Rockville, MD: Agency for Healthcare Research and Quality; 2017. Retrieved 10 June 2017 at http://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp.
Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27.
Elixhauser ASC, Kruzikas D. Elixhauser Comorbidity Software. Healthcare Cost and Utilization Project (HCUP). Rockville, MD: Agency for Healthcare Research and Quality. Retrieved 10 April 2017 at https://www.hcup-us.ahrq.gov/toolssoftware/comorbidity/comorbidity.jsp.
Royston P, Ambler G, Sauerbrei W. The use of fractional polynomials to model continuous risk variables in epidemiology. Int J Epidemiol. 1999;28:964–74.
StataCorp. Stata Statistical Software: Release 13. College Station, TX, StataCorp LP; 2013.
Dharmarajan K, Hsieh AF, Lin Z, Bueno H, Ross JS, Horwitz LI, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309:355–63.
Massarweh NN, Legner VJ, Symons RG, McCormick WC, Flum DR. Impact of advancing age on abdominal surgical outcomes. Arch Surg. 2009;144:1108–14.
Sogaard M, Thomsen RW, Bossen KS, Sorensen HT, Norgaard M. The impact of comorbidity on cancer survival: a review. Clin Epidemiol. 2013;5:3–29.
Lin HS, Watts JN, Peel NM, Hubbard RE. Frailty and postoperative outcomes in older surgical patients: a systematic review. BMC Geriatr. 2016;16:157.
Ommundsen N, Wyller TB, Nesbakken A, Jordhoy MS, Bakka A, Skovlund E, et al. Frailty is an independent predictor of survival in older patients with colorectal cancer. Oncologist. 2014;19:1268–75.
Mogal H, Vermilion SA, Dodson R, Hsu FC, Howerton R, Shen P, et al. Modified frailty index predicts morbidity and mortality after pancreaticoduodenectomy. Ann Surg Oncol. 2017;24(6):1714–1721.
Perna S, Francis MD, Bologna C, Moncaglieri F, Riva A, Morazzoni P, et al. Performance of Edmonton Frail Scale on frailty assessment: its association with multi-dimensional geriatric conditions assessed with specific screening tools. BMC Geriatr. 2017;17:2.
Jones DM, Song X, Rockwood K. Operationalizing a frailty index from a standardized comprehensive geriatric assessment. J Am Geriatr Soc. 2004;52:1929–33.
Soong JT, Poots AJ, Bell D. Finding consensus on frailty assessment in acute care through Delphi method. BMJ Open. 2016;6:e012904.
Hoogendijk EO, van der Horst HE, Deeg DJ, Frijters DH, Prins BA, Jansen AP, et al. The identification of frail older adults in primary care: comparing the accuracy of five simple instruments. Age Ageing. 2013;42:262–5.
Caillet P, Laurent M, Bastuji-Garin S, Liuu E, Culine S, Lagrange JL, et al. Optimal management of elderly cancer patients: usefulness of the Comprehensive Geriatric Assessment. Clin Interv Aging. 2014;9:1645–60.
Hulzebos EHJ, Smit Y, Helders PPJM, van Meeteren NLU. Preoperative physical therapy for elective cardiac surgery patients. Cochrane Database Syst Rev. 2012. doi:10.1002/14651858.CD010118.pub2.
Tegels JJW, De Maat MFG, Hulsewe KWE, Hoofwijk AGM, Stoot JHMB. Improving the outcomes in gastric cancer surgery. World J Gastroenterol. 2014;20:13692–704.
Gillis C, Li C, Lee L, Awasthi R, Augustin B, Gamsa A, et al. Prehabilitation versus rehabilitation: a randomized control trial in patients undergoing colorectal resection for cancer. Anesthesiology. 2014;121:937–47.
Li C, Carli F, Lee L, Charlebois P, Stein B, Liberman AS, et al. Impact of a trimodal prehabilitation program on functional recovery after colorectal cancer surgery: a pilot study. Surg Endosc. 2013;27:1072–82.
Lai Y, Huang J, Yang M, Su J, Liu J, Che G. Seven-day intensive preoperative rehabilitation for elderly patients with lung cancer: a randomized controlled trial. J Surg Res. 2016;209:30–6.
Kassin MT, Owen RM, Perez SD, Leeds I, Cox JC, Schnier K, et al. Risk factors for 30-day hospital readmission among general surgery patients. J Am Coll Surg. 2012;215:322–30.
Silver JK, Baima J. Cancer prehabilitation: an opportunity to decrease treatment-related morbidity, increase cancer treatment options, and improve physical and psychological health outcomes. Am J Phys Med Rehabil. 2013;92:715–27.
Soares SMdTP, Nucci LB, da Silva MMdC, Campacci TC. Pulmonary function and physical performance outcomes with preoperative physical therapy in upper abdominal surgery: a randomized controlled trial. Clin Rehab. 2013;27:616–27.
Timmerman H, de Groot J, Hulzebos H, de Knikker R, Kerkkamp H, Van Meeteren N. Feasibility and preliminary effectiveness of preoperative therapeutic exercise in patients with cancer: a pragmatic study. Physiother Theory Pract. 2011;27:117–24.
American College of Surgeons. Strong for Surgery. Retrieved 16 June 2017 at https://www.facs.org/quality-programs/strong-for-surgery.
Conflict of interest
There are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sharoky, C.E., Collier, K.T., Wirtalla, C.J. et al. Hospitalization in the Year Preceding Major Oncologic Surgery Increases Risk for Adverse Postoperative Events. Ann Surg Oncol 24, 3477–3485 (2017). https://doi.org/10.1245/s10434-017-6032-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-017-6032-y