Abstract
Background
The value of splenic vessels invasion (which identified T3 tumors) in prognosis after resection for pancreatic ductal adenocarcinoma (PDA) of the body and tail has not been extensively investigated. The goal of this study was to evaluate prognostic factors in PDA of the body/tail, emphasizing the role of splenic vessels infiltration.
Methods
Between 1990 and 2008, 87 patients who underwent distal pancreatectomy (DP) for histologically proven PDA of the body and tail were analyzed. Clinicopathological prognostic factors for survival were evaluated. Univariate and multivariable analyses were performed.
Results
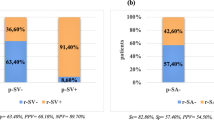
Postoperative morbidity was 31% with no mortality. The 1-, 3-, and 5-year overall survival rates were 77%, 48%, and 24.5%, respectively. Invasion of the splenic artery (SA) was observed in 19 patients (22%). Patients with SA invasion had a significantly poorer prognosis compared with those without SA invasion (median survival: 15 vs. 39 months, P = 0.014). On multivariable analysis, adjuvant therapy, poor differentiation (G3/G4), R2 resection, the presence of lymph node metastases, and SA invasion were independent predictors of survival.
Conclusions
Along with other well-known prognostic factors, invasion of SA is an independent predictor of poor survival in PDA of the body/tail. In case of the presence of SA infiltration, neoadjuvant treatment should be considered. SA infiltration might be reclassified from a T3 to T4 tumor.

Similar content being viewed by others
References
Brennan MF, Moccia RD, Klimstra D. Management of adenocarcinoma of the body and tail of the pancreas. Ann Surg. 1996;223:506–11.
Nordback IH, Hruban RH, Boitnott JK, et al. Carcinoma of the body and tail of the pancreas. Am J Surg. 1992;164:26–31.
Johnson CD, Schwall G, Flechtenmacher J, et al. Resection for adenocarcinoma of the body and tail of the pancreas. Br J Surg. 1993;80(9):1177–9.
Nakao A, Harada A, Nonami T, et al. Lymph node metastasis in carcinoma of the body and tail of the pancreas. Br J Surg. 1997;84(8):1090–2.
Schwarz RE, Harrison LE, Conlon KC, et al. The impact of splenectomy on outcomes after resection of pancreatic adenocarcinoma. J Am Coll Surg. 1999;188(5):516–21.
Sperti C, Pasquali C, Pedrazzoli S, et al. Ductal adenocarcinoma of the body and tail of the pancreas. J Am Coll Surg. 1997;185(3):255–9.
Shoup M, Conlon KC, Klimstra D, et al. Is extended resection for adenocarcinoma of the body of the pancreas justified? J Gastrointest Surg. 2003;7(8):946–52.
Strasberg SM, Linehan DC, Hawkins WG, et al. Radical anterograde modular pancreatosplenectomy procedure for adenocarcinoma of the body and tail of the pancreas: ability to obtain negative tangential margins. J Am Coll Surg. 2007;204(2):244–9.
Christein JD, Kendrick ML, Corey WI, et al. Distal pancreatectomy for resectable adenocarcinoma of the body and tail of the pancreas. J Gastrointest Surg. 2005;9(7):922–7.
Fujita T, Nakagohri T, Gotohda N, et al. Evaluation of the prognostic factors and significance of lymph node status in invasive ductal carcinoma of the body or tail of the pancreas. Pancreas. 2010;39(1):e48–54.
Wu X, Tao R, Lei R, et al. Distal pancreatectomy combined with celiac axis resection in treatment of carcinoma of the body/tail of the pancreas: a single-center experience. Ann Surg Oncol. 2010;17(5):1359–66.
Konishi M, Kinoshita T, Nakagori T, et al. Distal pancreatectomy with resection of the celiac axis and reconstruction of the hepatic artery for carcinoma of the body and tail of the pancreas. Hepatobiliary Pancreat Surg. 2000;7(2):183–7.
Yekebas EF, Bogoevski D, Cataldegirmen G, et al. En bloc vascular resection for locally advanced pancreatic malignancies infiltrating major blood vessels: perioperative outcome and long-term survival in 136 patients. Ann Surg. 2008;247(2):300–9.
Hirano S, Kondo S, Hara T, et al. Distal pancreatectomy with en bloc celiac axis resection for locally advanced pancreatic body cancer: long-term results. Ann Surg. 2007;246(1):46–51.
Sobin LH, Gospodarowicz MK, Wittekind C. UICC: TNM classification of malignant tumors, 7th edn. Oxford: Wiley-Blackwell; 2009.
Kanda M, Fujii T, Sahin TT, et al. Invasion of the splenic artery is a crucial prognostic factor in carcinoma of the body and tail of the pancreas. Ann Surg. 2010;251(3):483–7.
Lu DS, Reber HA, Krasny RM, Kadell BM, Sayre J. Local staging of pancreatic cancer: criteria for unresectability of major vessels as revealed by pancreatic-phase, thin-section helical CT. Am J Roentgenol. 1997;168(6):1439–43.
Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, Neoptolemos J, Sarr M, Traverso W, Buchler M; International Study Group on Pancreatic Fistola Definition. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005;138(1):8–13.
Neoptolemos JP, Stocken DD, Friess H, et al. A randomized trial of chemoradiotherapy and chemotherapy after resection of pancreatic cancer. N Engl J Med. 2004;350(12):1200–10.
Kennedy EP, Yeo CJ. The case for routine use of adjuvant therapy in pancreatic cancer. J Surg Oncol. 2007;95:597–603.
Picozzi VJ, Pisters PWT, et al. Strength of the evidence: adjuvant therapy for resected pancreatic cancer. J Gastrointest Surg. 2008;12:657–61.
Barugola G, Partelli S, Marcucci S, et al. Resectable pancreatic cancer: who really benefits from resection? Ann Surg Oncol. 2009;16(12):3316–22.
Nakao A, Harada A, Nonami T, et al. Clinical significance of carcinoma invasion of the extrapancreatic nerve plexus in pancreatic cancer. Pancreas. 1996;12:357–61.
Japan Pancreatic Society. Classification of pancreatic carcinoma, 6th edn. Tokyo: Kanehara; 2009.
Varadhachary GR, Tamm EP, Abbruzzese JL, et al. Borderline resectable pancreatic cancer: definitions, management, and the role of preoperative therapy. Ann Surg Oncol. 2006;13:1035–46.
Springett GM, Hoffe SE. Borderline resectable pancreatic cancer: on the edge of survival. Cancer Control. 2008;15(4):295–307.
Acknowledgment
The authors thank Ms. Deborah McGrath for help with revising the manuscript.
Conflicts of interest
There are no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Partelli, S., Crippa, S., Barugola, G. et al. Splenic Artery Invasion in Pancreatic Adenocarcinoma of the Body and Tail: A Novel Prognostic Parameter for Patient Selection. Ann Surg Oncol 18, 3608–3614 (2011). https://doi.org/10.1245/s10434-011-1769-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-011-1769-1