Abstract
Background
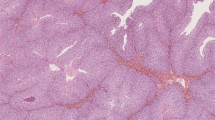
To determine the prognosis and prognostic factors in a large series of mucinous borderline tumors of the ovary (MBOT).
Materials and Methods
A retrospective review of patients with MBOT treated or referred to our institution. Three inclusion criteria were defined: (1) centralized histological review by our expert pathologist, (2) exclusion of peritoneal pseudomyxoma and any synchronous malignant tumor in the abdominal cavity, and (3) available data on the management and outcomes of patients.
Results
From 1997 to 2004, 97 patients fulfilled inclusion criteria (95 stage I and 2 stage II disease). Of these, 9 patients had endocervical-like subtypes, 8 patients had stromal microinvasion, and 24 had intraepithelial carcinoma. Radical and conservative surgeries were performed, respectively, in 28 and 69 patients. After a median follow-up of 48 months, 13 patients had developed 14 recurrences: 7 were borderline and 7 were invasive lesions. The probability of recurrence in the form of carcinoma 5 and 10 years after the diagnosis was, respectively, 9 and 13%. The only prognostic factor for recurrence attaining statistical significance was the use of a cystectomy (compared with other surgeries relative risk [RR] = 5.6; P = 0.003; compared with salpingo-oophorectomy RR = 5.5; P = 0.012).
Conclusions
In the present series of 97 MBOT, mainly early-stage disease and excluding peritoneal pseudomyxoma, the cumulative risk of recurrence in the form of invasive carcinoma at 10 years was 13%. MBOT do not appear to be such a “safe” disease. The only prognostic factor for recurrence was the use of a cystectomy, suggesting that a salpingo-oophorectomy should be preferred in cases of conservative treatment.


Similar content being viewed by others
References
Hart WR. Mucinous tumors of the ovary: a review. Int J Gynecol Pathol. 2005;24:4–25.
Ronnett BM, Kajdacsy-Balla A, Gilks CB, Merion MJ, Silva E, Werness BA, et al. Mucinous borderline ovarian tumors: points of general agreement and persistent controversies regarding nomenclature, diagnostic criteria, and behavior. Hum Pathol. 2004;35:949–60.
Tavassoli FA, Devilee P, editors.World Health Organization: Tumours of the Breast and Female Genital Organs (WHO/IARC Classification of Tumours). IARC Press: Lyon; 2003.
International Federation of Gynecology and Obstetrics. Changes in definitions of clinical staging for carcinoma of the cervix and ovary. Am J Obstet Gynecol. 1987;156:263–4.
Sumithran E, Susil BJ, Looi LM. The prognostic significance of grading in borderline mucinous tumors of the ovary. Hum Pathol. 1988;19:15–8.
Ji H, Yliskoski M, Anttila M, Syrjanen K, Saarikoski S. Management of stage-I borderline ovarian tumors. Int J Gynecol Obstet. 1996;54:37–44.
Gotlieb W, Flikker S, Davidson B, Korach Y, Kopolovic J, Ben-Baruch G. Borderline tumors of the ovary: fertility treatment, conservative management, and pregnancy outcome. Cancer. 1998;82:141–6.
Zanetta G, Rota S, Chiari S, Bonazzi C, Bratina G, Mangioni C. Behavior of borderline tumors with particular interest to persistence, recurrence, and progression to invasive carcinoma: a prospective study. J Clin Oncol. 2001;19:2656–64.
Suh-Burgmann E. Long-term outcomes following conservative surgery for borderline tumor of the ovary: a large population-based study. Gynecol Oncol. 2006;103:841–7.
Yokoyama Y, Moriya T, Takano T, Shoji T, Takahashi O, Nakahara K, et al. Clinical outcome and risks factors for recurrence in borderline ovarian tumours. Br J Cancer. 2006;94:1586–91.
Cho YH, Kim DY, Kim JH, Kim YM, Kim KR, Kim YT, et al. Is complete surgical staging necessary in patients with stage I mucinous epithelial ovarian tumors? Gynecol Oncol. 2006;103:878–82.
Wong HF, Low JJ, Chua Y, Busmanis I, Tay EH, Ho TH. Ovarian tumors of borderline malignancy: a review of 247 patients from 1991 to 2004. Int J Gynecol Cancer. 2007;17:342–9.
Park JY, Kim DY, Kim JH, Kim YM, Kim YT, Nam JH. Surgical management of borderline ovarian tumors: the role of fertility-sparing surgery. Gynecol Oncol. 2009;113:75–82.
Hart WR, Norris HJ. Borderline and malignant mucinous tumors of the ovary. Cancer. 1973;31:1031–44.
Siriaunkgul S, Robbins KM, McGowan L, Silverberg SG. Ovarian mucinous tumors of low malignant potential: a clinicopathologic study of 54 tumors of intestinal and müllerian type. Int J Gynecol Pathol. 1995;14:198–208.
Bradley RF, Stewart JH 4th, Russell GB, Levine EA, Geisinger KR. Pseudomyxoma peritonei of appendiceal origin: a clinicopathologic analysis of 101 patients uniformly treated at a single institution, with literature review. Am J Surg Pathol. 2006;30:551–9.
Ronnett BM, Shmookler BM, Sugarbaker PH, Kurman RJ. Pseudomyxoma peritonei: new concepts in diagnosis, origin, nomenclature, and relationship to mucinous borderline (low malignant potential) tumors of the ovary. Anat Pathol. 1997;2:197–226.
Shappell HW, Riopel MA, Smith Sehdev AE, Ronnett BM, Kurman RJ. Diagnostic criteria and behavior of ovarian seromucinous (endocervical-type mucinous and mixed cell-type) tumors: atypical proliferative (borderline) tumors, intraepithelial, microinvasive, and invasive carcinomas. Am J Surg Pathol. 2002;26:1529–41.
Rodriguez IM, Irving JA, Prat J. Endocervical-like mucinous borderline tumors of the ovary: a clinicopathologic analysis of 31 cases. Am J Surg Pathol. 2004;28:1311–8.
Rutgers JL, Scully RE. Ovarian mullerian mucinous papillary cystadenomas of borderline malignancy. A clinicopathologic analysis. Cancer. 1988;61:340–8.
Riopel MA, Ronnett BM, Kurman RJ. Evaluation of diagnostic criteria and behavior of ovarian intestinal-type mucinous tumors: atypical proliferative (borderline) tumors and intraepithelial, microinvasive, invasive, and metastatic carcinomas. Am J Surg Pathol. 1999;23:617–35.
Nomura K, Aizawa S. Noninvasive, microinvasive and invasive mucinous carcinomas of the ovary: a clinicopathologic analysis of 40 cases. Cancer. 2000;89:1541–6.
Lee KR, Scully RE. Mucinous tumors of the ovary: a clinicopathologic study of 196 borderline tumors (of intestinal type) and carcinomas, including an evaluation of 11 cases with “pseudomyxoma peritonei”. Am J Surg Pathol. 2000;24:1447–64.
De Nictolis M, Montironi R, Tommasoni S, Valli M, Pisani E, Fabris G, et al. Benign, borderline, and well-differentiated malignant intestinal mucinous tumors of the ovary: a clinicopathologic, histochemical, immunohistochemical, and nuclear quantitative study of 57 cases. Int J Gynecol Pathol. 1994;13:10–21.
Salomon LJ, Lhommé C, Pautier P, Duvillard P, Morice P. Safety of simple cystectomy in patients with unilateral mucinous borderline tumors. Fertil Steril. 2006;85:1–4.
Ramirez PT, Slomovitz BM, McQuinn L, Levenback C, Coleman RL, et al. Role of appendectomy at the time of primary surgery in patients with early-stage ovarian cancer. Gynecol Oncol. 2006;103:888–90.
Morice P. Borderline tumours of the ovary and fertility. Eur J Cancer. 2006;42:149–58.
Acknowledgment
We thank Lorna Saint Ange for editing. Acknowledgments to the following colleagues for updating the follow-up and outcomes of patients: Dr. Heurtin, Dr. Regal, Dr. Legent, Dr. Marti, Dr. Le Corre, Dr. Rouzier, Dr. Stoeckle, Dr. Floquet, Dr. Patrier Sallebert, Dr. Rossi, Dr. Quentin, Dr. Geraud, Dr. Jouatte, Dr. Baron, Dr. Collet, Dr. Auriault, Dr. Metzger, Dr. Foulques, Dr. Chabanne, Dr. Cayol, Dr. Hoock, Dr. Blanchot, Dr. Mercier, Dr. Sfairi, Dr. Fetissof, Dr. Khoudayer, Dr. Pichereau, Dr. Anger, Dr. Abbara, Dr. Henry, Dr. Cailliez, Dr. Houareau, Dr. Kessler, Dr. Aubert, Dr. Batt, Dr. Lupo, Dr. Guarnieri, Dr. Beaumont, Dr. Maes, Dr. Botti, Dr. Collin Barres, Dr. Hamdan, Dr. Le Vaguers, Dr. Barres, Dr. Deffieux, Dr. Loridon, Dr. Roy Bouzonnet, Dr. Sobole, Dr. Majer, Dr. Baillet, Dr. Tranbaloc, Dr. Jacquot, Dr. Munz Beaugrand, Dr. Truc, Dr. Jarlaud, Dr. Chevallier, Dr. Zago, Dr. Zogliani, Dr. Cohen-Aloro, Dr. Signon, Dr. Le Vagueres, Dr. De Tayrac, Dr. Pinteaux, Dr. Lelarge, Dr. Sambor, Dr. Treilleux, Dr. Marceau, and Dr. Rousseau.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Koskas, M., Uzan, C., Gouy, S. et al. Prognostic Factors of a Large Retrospective Series of Mucinous Borderline Tumors of the Ovary (Excluding Peritoneal Pseudomyxoma). Ann Surg Oncol 18, 40–48 (2011). https://doi.org/10.1245/s10434-010-1293-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-010-1293-8