Abstract
Background
Ischemia/reperfusion (I/R) injury is frequently encountered during hepatic surgery. We recently showed that I/R accelerates the outgrowth of pre-established colorectal micrometastases. The aim of this study was to assess the influence of ischemia time, gender, age, and liver steatosis on the accelerated outgrowth of colorectal metastases following I/R.
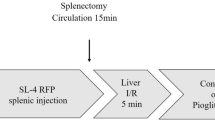
Methods
Five days after tumor cell inoculation, mice were subjected to 20, 30 or 45 min of left lobar I/R. To assess the influence of age, gender, and liver steatosis on I/R-accelerated tumor growth, we compared old with young mice, male with female mice, and mice with healthy livers with mice with steatotic livers. Endpoints were extent of tissue necrosis and tumor growth.
Results
With increasing ischemia times, tissue necrosis and I/R-accelerated tumor growth increased, with a significant stimulatory effect at 30 and 45 min of ischemia. I/R-stimulated outgrowth of micrometastases was further increased by 33% in aged mice and by 42% in steatotic livers and was associated with increased tissue necrosis. In female mice tissue necrosis had decreased by 47% and tumor growth was reduced in both control and clamped liver lobes. The stimulatory effect of I/R on metastasis outgrowth was similar in male and female mice.
Conclusions
I/R-accelerated outgrowth of colorectal micrometastases largely depends on the duration of the ischemic period, with a safe upper limit of 20 min in mice. The stimulatory effects of I/R on tumor growth are exacerbated in aged mice and in steatotic livers.


Similar content being viewed by others
References
Selzner M, Clavien PA. Resection of hepatic tumors: special emphasis on neoadjuvant and adjuvant therapy. In Clavien PA, ed. Malignant liver tumors: current and emerging therapies. Sudbury, Massachusets, USA: Jones and Bartlett, 2004:153–69
Simmonds PC, Primrose JN, Colquitt JL, et al. Surgical resection of hepatic metastases from colorectal cancer: a systematic review of published studies. Br J Cancer 2006;94:982–99
Yokoyama N, Shirai Y, Ajioka Y, et al. Immunohistochemically detected hepatic micrometastases predict a high risk of intrahepatic recurrence after resection of colorectal carcinoma liver metastases. Cancer 2002; 94:1642–7
Abdalla EK, Vauthey JN, Ellis LM, et al. Recurrence and outcomes following hepatic resection, radiofrequency ablation, and combined resection/ablation for colorectal liver metastases. Ann Surg 2004; 239:818–25
Nakajima Y, Shimamura T, Kamiyama T, et al. Control of intraoperative bleeding during liver resection: analysis of a questionnaire sent to 231 Japanese hospitals. Surg Today 2002; 32:48–52
van der Bilt JD, Livestro DP, Borren A, et al. European survey on the application of vascular occlusion in liver surgery. Dig Surg 2007; 24:423–35
van der Bilt JD, Kranenburg O, Nijkamp MW, et al. Ischemia/reperfusion accelerates the outgrowth of hepatic micrometastases in a highly standardized murine model. Hepatology 2005; 42:165–75
Nordlinger B, Douvin D, Javaudin L, et al. An experimental study of survival after two hours of normothermic hepatic ischemia. Surg Gynecol Obstet 1980; 150:859–64
Liu DL, Jeppsson B, Hakansson CH, et al. Multiple-system organ damage resulting from prolonged hepatic inflow interruption. Arch Surg 1996; 131:442–7
Hines IN, Hoffman JM, Scheerens H, et al. Regulation of postischemic liver injury following different durations of ischemia. Am J Physiol Gastrointest Liver Physiol 2003; 284:G536–45
Le Couteur DG, Rivory LP, Pond SM. The effects of aging and nutritional state on hypoxia-reoxygenation injury in the perfused rat liver. Transplantation 1994; 58:531–6
Clavien PA, Selzner M, Rudiger HA, et al. A prospective randomized study in 100 consecutive patients undergoing major liver resection with versus without ischemic preconditioning. Ann Surg 2003; 238:843–50
Okaya T, Blanchard J, Schuster R, et al. Age-dependent responses to hepatic ischemia/reperfusion injury. Shock 2005; 24:421–7
Harada H, Pavlick KP, Hines IN, et al. Selected contribution: Effects of gender on reduced-size liver ischemia and reperfusion injury. J Appl Physiol 2001; 91:2816–22
Eckhoff DE, Bilbao G, Frenette L, et al. 17-Beta-estradiol protects the liver against warm ischemia/reperfusion injury and is associated with increased serum nitric oxide and decreased tumor necrosis factor-alpha. Surgery 2002; 132:302–9
Lu P, Liu F, Wang CY, et al. Gender differences in hepatic ischemic reperfusion injury in rats are associated with endothelial cell nitric oxide synthase-derived nitric oxide. World J Gastroenterol 2005; 11:3441–5
Behrns KE, Tsiotos GG, DeSouza NF, et al. Hepatic steatosis as a potential risk factor for major hepatic resection. J Gastrointest Surg 1998; 2:292–8
Belghiti J, Noun R, Malafosse R, et al. Continuous versus intermittent portal triad clamping for liver resection: a controlled study. Ann Surg 1999; 229:369–75
Ijaz S, Yang W, Winslet MC, et al. Impairment of hepatic microcirculation in fatty liver. Microcirculation 2003; 10:447–56
Selzner N, Selzner M, Jochum W, et al. Mouse livers with macrosteatosis are more susceptible to normothermic ischemic injury than those with microsteatosis. J Hepatol 2006; 44:694–701
van der Bilt JD, Kranenburg O, Verheem A, et al. Selective portal clamping to minimize hepatic ischaemia-reperfusion damage and avoid accelerated outgrowth of experimental colorectal liver metastases. Br J Surg 2006; 93:1015–22
Kahn D, Hickman R, Dent DM, et al. For how long can the liver tolerate ischaemia? Eur Surg Res 1986; 18:277–82
Delva E, Camus Y, Nordlinger B, et al. Vascular occlusions for liver resections. Operative management and tolerance to hepatic ischemia: 142 cases. Ann Surg 1989; 209:211–8
Quan D, Wall WJ. The safety of continuous hepatic inflow occlusion during major liver resection. Liver Transpl Surg 1996; 2:99–104
Elias D, Desruennes E, Lasser P. Prolonged intermittent clamping of the portal triad during hepatectomy. Br J Surg 1991; 78:42–4
Huguet C, Gavelli A, Bona S. Hepatic resection with ischemia of the liver exceeding one hour. J Am Coll Surg 1994; 178:454–8
Sakamoto Y, Makuuchi M, Takayama T, et al. Pringle’s maneuver lasting 322 min. Hepatogastroenterology 1999; 46:457–8
Fong Y, Brennan MF, Cohen AM, et al. Liver resection in the elderly. Br J Surg 1997; 84:1386–90
Cescon M, Grazi GL, Del Gaudio M, et al. Outcome of right hepatectomies in patients older than 70 years. Arch Surg 2003; 138:547–52
Menon KV, Al Mukhtar A, Aldouri A, et al. Outcomes after major hepatectomy in elderly patients. J Am Coll Surg 2006; 203:677–83
Brand MI, Saclarides TJ, Dobson HD, et al. Liver resection for colorectal cancer: liver metastases in the aged. Am Surg 2000; 66:412–5
Leporrier J, Maurel J, Chiche L, et al. A population-based study of the incidence, management and prognosis of hepatic metastases from colorectal cancer. Br J Surg 2006; 93:465–74
Gasbarrini A, Simoncini M, Di Campli C, et al. Ageing affects anoxia/reoxygenation injury in rat hepatocytes. Scand J Gastroenterol 1998; 33:1107–12
Ratto C, Sofo L, Ippoliti M, et al. Prognostic factors in colorectal cancer. Literature review for clinical application. Dis Colon Rectum 1998; 41:1033–49
Wang JY, Chiang JM, Jeng LB, et al. Resection of liver metastases from colorectal cancer: are there any truly significant clinical prognosticators? Dis Colon Rectum 1996; 39:847–51
Scheele J, Altendorf-Hofmann A. Resection of colorectal liver metastases. Langenbecks Arch Surg 1999; 384:313–27
Brahimi-Horn C, Berra E, Pouyssegur J. Hypoxia: the tumor’s gateway to progression along the angiogenic pathway. Trends Cell Biol 2001; 11:S32–6
Harris AL. Hypoxia-a key regulatory factor in tumour growth. Nat Rev Cancer 2002; 2:38–47
van der Bilt JD, Soeters ME, Duijverman AM, et al. Perinecrotic hypoxia contributes to ischemia/reperfusion-accelerated outgrowth of colorectal micrometastases. Am J Pathol 2007; 170:1379–88
Vauthey JN, Pawlik TM, Ribero D, et al. Chemotherapy regimen predicts steatohepatitis and an increase in 90-day mortality after surgery for hepatic colorectal metastases. J Clin Oncol 2006; 24:2065–72
Karoui M, Penna C, Amin-Hashem M, et al. Influence of preoperative chemotherapy on the risk of major hepatectomy for colorectal liver metastases. Ann Surg 2006; 243:1–7
Benoist S, Salabert AS, Penna C, et al. Portal triad clamping (TC) or hepatic vascular exclusion (VE) for major liver resection after prolonged neoadjuvant chemotherapy? A case-matched study in 60 patients. Surgery 2006; 140:396–403
Acknowledgements
This work was supported by The Netherlands Organization for Health Research and Development (Grant no. 920-03-313).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
van der Bilt, J.D.W., Kranenburg, O., Borren, A. et al. Ageing and Hepatic Steatosis Exacerbate Ischemia/Reperfusion-Accelerated Outgrowth of Colorectal Micrometastases. Ann Surg Oncol 15, 1392–1398 (2008). https://doi.org/10.1245/s10434-007-9758-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-007-9758-0