Abstract
Background
Tumor board recommendations for breast cancer are mainly based on patient characteristics and prognostic tumor parameters. In the era of potential avoidance of axillary surgery we evaluate the impact of pathologic nodal status for adjuvant treatment decisions.
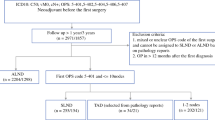
Methods
Postoperative tumor board records of 207 patients over a 1-year period were rediscussed without knowledge of pathologic nodal status. Differences were classified as major (chemotherapy and/or radiotherapy: present/absent) or minor (different chemotherapeutic protocols) discrepancies. The survival rates among subgroups were calculated using Adjuvant! Online tool.
Results
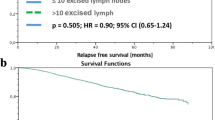
The tumor board without information of pathologic nodal status resulted in treatment changes in 72 of the 207 patients studied (34.8%). Major discrepancies were observed in 37 patients (17.9%). The survival rates were not significantly different due to a balanced overtreatment and undertreatment in this subgroup. Lymphovascular invasion (LVI) was an independent parameter used to predict the subgroup with major discrepancies (P = .001; RR = 4.9 [95% CI, 1.9–12.7]).
Conclusions
The knowledge of pathologic nodal status is important for postoperative chemotherapy and postmastectomy radiotherapy indications. There is a risk for one-third of all patients when avoiding axillary surgery to get an adjuvant therapy that differs from the current guidelines especially in carcinomas with present LVI.
Similar content being viewed by others
References
Fisher B, Jeong JH, Anderson S, Bryant J, Fisher ER, Wolmark N. Twenty-five-year follow-up of a randomized trial comparing radical mastectomy, total mastectomy, and total mastectomy followed by irradiation. N Engl J Med 2002; 347:567–75
Dees EC, Shulman LN, Souba WW, Smith BL. Does information from axillary dissection change treatment in clinically node-negative patients with breast cancer? Ann Surg 1997; 226:279–87
Orr RK. The impact of prophylactic axillary node dissection on breast cancer survival—a Bayesian meta-analysis. Ann Surg Oncol 1999; 6:109–16
Parmigiani G, Berry DA, Winer EP, Tebaldi C, Iglehart JD, Prosnitz LR. Is axillary lymph node dissection indicated for early-stage breast cancer? A decision analysis. J Clin Oncol 1999; 17:1465–73
Goldhirsch A, Coates AS, Gelber RD, Glick JH, Thürlimann B, Senn HJ. First—select the target: better choice of adjuvant treatments for breast cancer patients. Ann Oncol 2006; 17:1772–6
Engel J, Lebeau A, Sauer H, Hölzel D. Are we wasting our time with the sentinel technique? Fifteen reasons to stop axilla dissection. Breast 2006; 15:452–5
Henderson IC. Axillary surgery: clinical judgment required. J Clin Oncol 2006; 24:325–6
Kuehn T, Bembenek A, Decker T, Munz DL, Sautter-Bihl ML, Untch M, Wallwiener D. A concept for the clinical implementation of sentinel lymph node biopsy in patients with breast carcinoma with special regard to quality assurance. Cancer 2005; 103:451–61
Goldhirsch A, Glick JH, Gelber RD, Coates AS, Thürlimann B, Senn HJ. Meeting highlights: International expert consensus on the primary therapy of early breast cancer 2005. Ann Oncol 2005; 16:1569–83
Ravdin PM, Siminoff LA, Davis GJ, Mercer MB, Hewlett J, Gerson N, Parker HL. Computer program to assist in making decisions about adjuvant therapy for women with early breast cancer. J Clin Oncol 2001; 19:980–91
Chua B, Ung O, Taylor R, Boyages J. Is information from axillary dissection relevant to patients with clinically node-negative breast cancer? Breast J 2003; 9:478–84
Greco M, Gennaro M, Valagussa P, et al. Impact of nodal status on indication for adjuvant treatment in clinically node negative breast cancer. Ann Oncol 2000; 11:1137–40
Jackson JSH, Olivotto IA, Wai E, Grau C, Mates D, Ragaz J. A decision analysis of the effect of avoiding axillary lymph node dissection in low risk women with invasive breast carcinoma. Cancer 2000; 88:1852–62
Olivotto IA, Bajdik CD, Ravdin PM, et al. Population-based validation of the prognostic model ADJUVANT! for early breast cancer. J Clin Oncol 2005; 23:2716–25
Wong JS, O’Neill A, Recht A, Schnitt SJ, Connolly JL, Silver B, Harris JR. The relationship between lymphatic vessel invasion, tumor size, and pathological nodal status: can we predict who can avoid a third field in the absence of axillary dissection? Int J Radiat Oncol Biol Phys 2000; 48:133–7
Olivotto IA, Jackson JSH, Mates D, Andersen S, Davidson W, Bryce CJ, Ragaz J. Prediction of axillary lymph node involvement of women with invasive breast carcinoma. Cancer 1998; 83:948–55
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Reimer, T., Fietkau, R., Markmann, S. et al. How Important is the Axillary Nodal Status for Adjuvant Treatment Decisions at a Breast Cancer Multidisciplinary Tumor Board? A Survival Analysis. Ann Surg Oncol 15, 472–477 (2008). https://doi.org/10.1245/s10434-007-9670-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-007-9670-7