Abstract
Background
Most melanoma patients present with thin (≤1.0 mm) lesions. Indications for sentinel lymph node (SLN) biopsy are not well defined for this group. Previously, we reported an association between mitotic rate (MR) and SLN positivity in these patients. The study was limited by a relatively small sample size and low statistical power. In this study, we evaluated a large population of patients with thin melanoma from the pre-SLN era to identify predictors of regional nodal disease (RND) that may serve as a surrogate for SLN positivity.
Methods
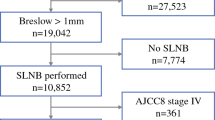
Eight hundred eighty-two patients evaluated between 1972 and 1991 were included in the study. Univariate and multivariate regression analyses were performed by using clinical and histological data to identify factors associated with RND. A multivariate logistic regression model was developed and applied to the previously reported group of patients with thin melanomas who underwent SLN biopsy between 1996 and 2004 for validation.
Results
Thirty-eight patients (4.3%) had evidence of RND. In the multivariate analysis, a MR >0, vertical growth phase (VGP), male sex, and ulceration were statistically significant predictors of RND. Patients at the highest risk according to a classification tree analysis (VGP and MR >0) had an RND rate of 11.9%. The regression model developed predicted well the SLN status in the validation sample.
Conclusions
Investigation of a large pre-SLN population identified MR >0, ulceration, VGP, and male sex as independently predictive of RND in patients with thin melanomas. These factors may help to identify subgroups of these patients that have clinically significant risks of SLN positivity.



Similar content being viewed by others
References
Surveillance, Epidemiology, and End Results (SEER) Program. Public-use data (1973–2000), National Cancer Institute, DCCPS, Surveillance Research Program, Cancer Statistics Branch. Released April 2004. Based on the November 2003 submission. Available at: http://www.seer.cancer.gov/publicdata
Reintgen D, Balch CM, Kirkwood J, Ross M. Recent advances in the care of the patient with malignant melanoma. Ann Surg 1997;225:1–14
Woods JE, Soule EH, Creagan ET. Metastasis and death in patients with thin melanomas (less than 0.76 mm). Ann Surg 1983;198:63–4
Gimotty PA, Guerry D, Ming ME, et al. Thin primary cutaneous malignant melanoma: a prognostic tree for 10-year metastasis is more accurate than American Joint Committee on Cancer staging. J Clin Oncol 2004;22:3668–76
Morton DL, Wen DR, Wong JH, et al. Technical details of intraoperative lymphatic mapping for early stage melanoma. Arch Surg 1992; 127: 392–9
Morton DL, Thompson JF, Essner R, et al. Validation of the accuracy of intraoperative lymphatic mapping and sentinel lymphadenectomy for early-stage melanoma: a multicenter trial. Multicenter Selective Lymphadenectomy Trial Group. Ann Surg 1999;230:453–63; discussion 463–5
Gershenwald JE, Thompson W, Mansfield PF, et al. Multi-institutional melanoma lymphatic mapping experience: the prognostic value of sentinel lymph node status in 612 stage I or II melanoma patients. J Clin Oncol 1999;17:976–83
Bleicher RJ, Essner R, Foshag LJ, et al. Role of sentinel lymphadenectomy in thin invasive cutaneous melanomas. J Clin Oncol 2003;21:1326–31
Jacobs IA, Chang CK, DasGupta TK, Salti GI. Role of sentinel lymph node biopsy in patients with thin (<1 mm) primary melanoma. Ann Surg Oncol 2003;10:558–61
Bedrosian I, Faries MB, Guerry DT, et al. Incidence of sentinel node metastasis in patients with thin primary melanoma (< or = 1 mm) with vertical growth phase. Ann Surg Oncol 2000;7:262–7
Kesmodel SB, Karakousis GC, Botbyl JB, al. Mitotic rate as a predictor of sentinel lymph node positivity in patients with thin melanomas. Ann Surg Oncol 2005; 12:449–58
Agnese DM, Abdessalam SF, Burak WE Jr, et al. Cost-effectiveness of sentinel lymph node biopsy in thin melanomas. Surgery 2003;134:542–7; discussion 547–8
Balch CM, Soong SJ, Gershenwald JE, et al. Prognostic factors analysis of 17,600 melanoma patients: validation of the American Joint Committee on Cancer melanoma staging system. J Clin Oncol 2001;19:3622–34
Steinberg D, Colla P. CART: Tree-Structured Non-Parametric Data Analysis. San Diego: Salford Systems, 1995
Wagner JD, Gordon MS, Chuang TY, et al. Predicting sentinel and residual lymph node basin disease after sentinel lymph node biopsy for melanoma. Cancer 2000;89:453–62
Slingluff CL Jr, Vollmer RT, Reintgen DS, Seigler HF. Lethal “thin” malignant melanoma. Identifying patients at risk. Ann Surg 1988;208:150–61
Leiter U, Buettner PG, Eigentler TK, Garbe C. Prognostic factors of thin cutaneous melanoma: an analysis of the central malignant melanoma registry of the German Dermatological Society. J Clin Oncol 2004;22:3660–7
McKinnon JG, Yu XQ, McCarthy WH, Thompson JF. Prognosis for patients with thin cutaneous melanoma: long-term survival data from New South Wales Central Cancer Registry and the Sydney Melanoma Unit. Cancer 2003;98:1223–31
Mansson-Brahme E, Carstensen J, Erhardt K, et al. Prognostic factors in thin cutaneous malignant melanoma. Cancer 1994;73:2324–32
Azzola MF, Shaw HM, Thompson JF, et al. Tumor mitotic rate is a more powerful prognostic indicator than ulceration in patients with primary cutaneous melanoma: an analysis of 3661 patients from a single center. Cancer 2003;97:1488–98
Corsetti RL, Allen HM, Wanebo HJ. Thin < or = 1 mm level III and IV melanomas are higher risk lesions for regional failure and warrant sentinel lymph node biopsy. Ann Surg Oncol 2000;7:456–60
Sondak VK, Taylor JM, Sabel MS, et al. Mitotic rate and younger age are predictors of sentinel lymph node positivity: lessons learned from the generation of a probabilistic model. Ann Surg Oncol 2004;11:247–58
Nguyen CL, McClay EF, Cole DJ, et al. Melanoma thickness and histology predict sentinel lymph node status. Am J Surg 2001;181:8–11
McMasters KM, Wong SL, Edwards MJ, et al. Factors that predict the presence of sentinel lymph node metastasis in patients with melanoma. Surgery 2001;130:151–6
Rousseau DL Jr, Ross MI, Johnson MM, et al. Revised American Joint Committee on Cancer staging criteria accurately predict sentinel lymph node positivity in clinically node-negative melanoma patients. Ann Surg Oncol 2003;10:569–74
Mraz-Gernhard S, Sagebiel RW, Kashani-Sabet M, et al. Prediction of sentinel lymph node micrometastasis by histological features in primary cutaneous malignant melanoma. Arch Dermatol 1998;134:983–7
Oliveira Filho RS, Ferreira LM, Biasi LJ, et al. Vertical growth phase and positive sentinel node in thin melanoma. Braz J Med Biol Res 2003;36:347–50
Olah J, Gyulai R, Korom I, et al. Tumour regression predicts higher risk of sentinel node involvement in thin cutaneous melanomas. Br J Dermatol 2003;149:662–3
Stitzenberg KB, Groben PA, Stern SL, et al. Indications for lymphatic mapping and sentinel lymphadenectomy in patients with thin melanoma (Breslow thickness < or =1.0 mm). Ann Surg Oncol 2004;11:900–6
Thompson JF, Shaw HM. Should tumor mitotic rate and patient age, as well as tumor thickness, be used to select melanoma patients for sentinel node biopsy? Ann Surg Oncol 2004;11:233–5
Cascinelli N, Belli F, Santinami M, et al. Sentinel lymph node biopsy in cutaneous melanoma: the WHO Melanoma Program experience. Ann Surg Oncol 2000;7:469–74
Joseph E, Brobeil A, Glass F, et al. Results of complete lymph node dissection in 83 melanoma patients with positive sentinel nodes. Ann Surg Oncol 1998;5:119–25
Acknowledgments
This study was supported in part by the SPORE on Skin Cancer (CA-093372; M. Herlyn, principal investigator). The authors thank all of the patients who were seen at the Pigmented Lesion Clinic (PLC) and gave their consent for use of their data for research studies, as well as the investigators (W. H. Clark, Jr, MD [deceased], E. E. Bondi, MD, L. P. Bucky, MD, L. S. Callans, MD, B. Chang, MD, K. T. Flaherty, MD, A. C. Halpern, MD, R. Hamilton, MD, D. Hershock, MD, D. D. Larossa, MD, S. R. Lessin, MD, D. Low, MD, P. Van Belle, MD, and J. Wolfe, MD) and staff (R. Holmes, S. Hotz, N. Lowden, I. Matozzo, M. Price, M. Synnestvedt, and J. Thompson) of the PLC for their contributions over the last three decades to the Melanoma Core Database on which this report is based.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Karakousis, G.C., Gimotty, P.A., Botbyl, J.D. et al. Predictors of Regional Nodal Disease in Patients With Thin Melanomas. Ann Surg Oncol 13, 533–541 (2006). https://doi.org/10.1245/ASO.2006.05.011
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/ASO.2006.05.011