Abstract
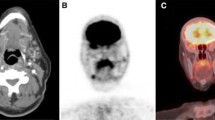
Background: Conventional imaging such as with 99mTc(V)dimercaptosunnic acid (DMSA), 111In-octreotide scintigraphy, computed tomography (CT), and magnetic resonance imaging (MRI) rarely localizes occult medullary thyroid cancer (MTC). The role of 18F-fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET) is not well defined. The aim of this study was to examine the usefulness of postoperative FDG-PET in localizing MTC metastases.
Methods: FDG-PET was performed in 26 patients with elevated serum tumor markers after total thyroidectomy with central compartment dissection and additional neck dissection on indication. Patient- and lesion-based results were compared with the findings of conventional nuclear imaging and validated by morphological imaging (CT, MRI, ultrasonography), including bone scintigraphy and pathology when possible. Clinical impact was evaluated.
Results: FDG-PET detected foci in 50% of patients with lesion-based sensitivity of 96%. 111In-octreotide detected foci in 19% with sensitivity of 41%, and 99mTc(V)DMSA scintigraphy and morphological imaging detected foci in 21% and 40%, respectively, with sensitivity of 57% and 87%. No lesions were found in 11 patients (42%). Positive FDG-PET findings led to surgical intervention in nine patients (35%). They all underwent surgery for removal of residual tumor or metastases. One patient achieved disease-free status. In all patients who underwent surgery, serum calcitonin levels were reduced by an average of 58 ± 31%.
Conclusions: For detection of occult MTC lesions, FDG-PET is superior to conventional nuclear imaging and is the best detection method yet available. FDG-PET in postoperative follow-up has clinical value and may be used for guiding reoperation and additional morphological imaging preoperatively.
Similar content being viewed by others
REFERENCES
Saad MF, Ordonez NG, Rashid RK, et al. Medullary carcinoma of the thyroid: study of the clinical features and prognostic factors in 161 patients. Medicine 1984; 63: 319–42.
Kebebew E, Ituarte PH, Siperstein AE, Duh QY, Klark OH. Medullary thyroid carcinoma: clinical characteristics, treatment, prognostic factors, and a comparison of staging systems. Cancer 2000; 88: 1139–48.
Brierley J, Tsang R, Simpson WJ, Gospodarowicz M, Sutcliffe S, Panzarella T. Medullary thyroid cancer: analysis of survival and prognostic factors and the role of radiation therapy in local control. Thyroid 1996; 6: 305–10.
Lairmore TC, Wells SA Jr. Medullary carcinoma of the thyroid: current diagnosis and management. Seminin Surg Oncol 1991; 7: 92–9.
Orlandi F, Caraci P, Mussa A, Saggiorato E, Pancani G, Angeli A. Treatment of medullary thyroid carcinoma: an update. Endocr Relat Cancer 2001; 8: 135–47.
Heshmati HM, Gharib H, van Heerden JA. Advances and controversies in the diagnosis and management of medullary thyroid carcinoma. Am J Med 1997; 103: 60–9.
Hoefnagel CA, Delprat CC, Marcuse HR, de Vijlder JJM. Role of thallium-201 total-body scintigraphy in follow-up of thyroid carcinoma. J Nucl Med 1986; 27: 1854–7.
Amstein NB, Juni JE, Sisson JC, Lloyd RV, Thompson NW. Recurrent medullary carcinoma of the thyroid demonstrated by thallium-201 scintigraphy. J Nucl Med 1986; 27: 1564–8.
Adalet I, Kocak M, Oguz H, Alagol F, Cantez S. Determination of medullary thyroid carcinoma metastases by 201Tl, 99Tcm(V)DMSA, 99Tcm-MIBI and 99Tcm-tetrofosmin. Nucl Med Commun 1999; 20: 353–9.
Baulieu J, Guilloteau D, Delisle M, et al. Radioiodinated metaiodobenzylguanidine uptake in medullary thyroid cancer. Cancer 1987; 60: 2189–94.
Ugur O, Kostakglu L, Guler N, et al. Comparison of 99mTc(V)-DMSA, 201Tl and 99mTc-MIBI imaging in the follow-up of patients with medullary carcinoma of the thyroid. Eur J Nucl Med 1996; 23: 1367–71.
Guerra U, Pizzocaro C, Terzi A, Giubbini R, Bestagno M. The use of 99m Tc(V)DMSA as imaging for the medullary thyroid carcinoma (MTC). J Nucl Med Allied Sci 1988; 32: 242–7.
Mojiminiyi OA, Udelsman R, Soper ND, Shepstone BJ, Dudley NE. Pentavalent Tc-99m DMSA scintigraphy. Prospective evaluation of its role in the management of patients with medullary carcinoma of the thyroid. Clin Nucl Med 1991; 16: 259–62.
Berna L, Cabezas R, Mora J, Torres G, Estorch M, Carrio I. 111In-octreotide and 99mTc(V)-dimercaptosuccinic acid studies in the imaging of recurrent medullary thyroid carcinoma. J Endocrinol 1995; 144: 339–345.
Adams S, Baum RP, Hertel A, Schumm-Dräger PM, Usadel KH, Hor G. Comparison of metabolic and receptor imaging in recurrent medullary thyroid carcinoma with histopathological findings. Eur J Nucl Med 1998; 25: 1277–1283.
Berna L, Chico A, Matias-Guiu X, et al. Use of somatostatin analogue scintigraphy in the localization of recurrent medullary thyroid carcinoma. Eur J Nucl Med 1998; 25: 1482–8.
Krausz Y, Rosler A, Guttmann H, et al. Somatostatin receptor scintigraphy for early detection of regional and distant metastases of medullary carcinoma of the thyroid. Clin Nucl Med 1999; 24: 256–60.
Gasparoni P, Rubello D, Ferlin G. Potential role of fluorine-18-deoxyglucose (FDG) positron emission tomography (PET) in the staging of primitive and recurrent medullary thyroid carcinoma. J Endocrinol Invest 1997; 20: 527–30.
Musholt TJ, Musholt PB, Dehdashti F, Moley JF. Evaluation of fluorodeoxyglucose-positron emission tomographic scanning and its association with glucose transporter expression in medullary thyroid carcinoma and pheochromocytoma: a clinical and molecular study. Surgery. 1997; 122: 1049–60;discussion 1060–1.
Brandt-Mainz K, Muller SP, Gorges R, Saller B, Bockisch A. The value of fluorine-18 fluorodeoxyglucose PET in patients with medullary thyroid cancer. Eur J Nucl Med 2000; 27: 490–6.
Diehl M, Risse JH, Brandt-Mainz K, et al. Fluorine-18 fluorodeoxyglucose positron emission tomography in medullary thyroid cancer: results of a multicentre study. Eur J Nucl Med 2001; 28: 1671–6.
Szakall S Jr., Esik O, Bajzik G, et al. 18F-FDG PET detection of lymph node metastases in medullary thyroid carcinoma. J Nucl Med 2002; 43: 66–71.
Kebebew E, Kikuchi S, Duh QY, Clark OH. Long-term results of reoperation and localizing studies in patients with persistent or recurrent medullary thyroid cancer. Arch Surg 2000; 135: 895–901.
Chen H, Roberts JR, Ball DW, et al. Effective long-term palliation of symptomatic, incurable metastatic medullary thyroid cancer by operative resection. Ann Surg 1998; 227: 887–95.
van Heerden JA, Grant CS, Gharib H, Hay ID, Ilstrup DM. Long-term course of patients with persistent hypercalcitoninemia after apparent curative primary surgery for medullary thyroid carcinoma. Ann Surg 1990; 212: 395–400.
Hoegerle S, Altehoefer C, Ghanem N, Brink I, Moser E, Nitzsche E. 18F-DOPA positron emission tomography for tumour detection in patients with medullary thyroid carcinoma and elevated calcitonin levels. Eur J Nucl Med 2001; 28: 64–71.
Nakamoto Y, Osman M, Wahl RL. Prevalence and patterns of bone metastases detected with positron emission tomography using F-18 FDG. Clin Nucl Med 2003; 28: 302–7.
Reubi JC, Chayvialle JA, Franc B, Cohen R, Calmettes C, Modigliani E. Somatostatin receptors and somatostatin content in medullary thyroid carcinomas. Lab Invest 1991; 64: 567–73.
Wang Q, Takashima S, Fukuda H, Takayama F, Kobayashi S, Sone S. Detection of medullary thyroid carcinoma and regional lymph node metastases by magnetic resonance imaging. Arch Otolaryngol Head Neck Surg 1999; 125: 842–8.
Van den Brekel MW. Lymph node metastases: CT and MRI. Eur J Radiol 2000; 33: 230–8.
James C, Starks M, MacGillivray DC, White J. The use of imaging studies in the diagnosis and management of thyroid cancer and hyperparathyroidism. Surg Oncol Clin N Am 1999; 8: 145–69.
Adams S, Baum R, Rink T, Schumm-Dräger PM, Usadel KH, Hör G. Limited value of fluorine-18 fluorodeoxyglucose positron emission tomography for the imaging of neuroendocrine tumors. Eur J Nucl Med 1998; 25: 79–83.
Tung WS, Vesely TM, Moley JF. Laparoscopic detection of hepatic metastases in patients with residual or recurrent medullary thyroid cancer. Surgery 1995; 118: 1024–9.
Ésik O, Szavcsur P, Szakall S Jr., et al. Angiography effectively supports the diagnosis of hepatic metastases in medullary thyroid carcinoma. Cancer 2001; 91: 2084–95.
Shreve PD, Anzai Y, Wahl RL. Pitfalls in oncologic diagnosis with FDG PET imaging: physiologic and benign variants. Radiographics 1999; 19: 61–77.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
de Groot, J.W.B., Links, T.P., Jager, P.L. et al. Impact of 18F-Fluoro-2-Deoxy-D-Glucose Positron Emission Tomography (FDG-PET) in Patients with Biochemical Evidence of Recurrent or Residual Medullary Thyroid Cancer. Ann Surg Oncol 11, 786–794 (2004). https://doi.org/10.1245/ASO.2004.10.015
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1245/ASO.2004.10.015