Abstract
Background
The use of nonsteroidal anti-inflammatory drugs is an effective adjunct in managing perioperative pain. We sought to determine if the use of intraoperative ketorolac as part of a multimodal ERAS protocol increased the risk of bleeding complications in breast surgery.
Methods
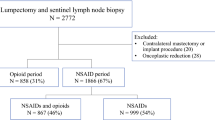
A subset analysis of a prospective cohort study including patients undergoing lumpectomy and mastectomy compared two groups: those who received intraoperative ketorolac and those who did not. Bleeding complications were compared using Fisher’s exact test or t test, and analyzed with respect to surgical modality. Patients undergoing immediate reconstruction were excluded.
Results
Seven hundred and fifty-eight breast surgeries were performed in a 13-month period: 157 lumpectomy patients and 57 mastectomy patients met inclusion criteria between July 2017 and August 2018. Two hundred and fourteen patients were included in the analysis: 115 received ketorolac and 99 did not. The two groups were similar with regards to sex, age, race, tobacco use, and comorbidities. When analyzed together, there was no difference in bleeding complications between the group that received intraoperative ketorolac and those who did not (2% vs. 2.6%, p = 1.00). No hematomas occurred in the lumpectomy patients, and three occurred in mastectomy patients: one of which received ketorolac, and two did not (5.9% vs. 5.0%, p = 0.575). The rates of seroma, infection, or dehiscence were not significantly different between the two groups, regardless of surgical modality.
Conclusions
The use of intraoperative ketorolac is a useful adjunct in perioperative pain management in breast surgery and does not increase the risk of bleeding.

Similar content being viewed by others
References
Nimmo SM, Foo ITH, Paterson HM. Enhanced recovery after surgery: pain management. J Surg Oncol. 2017;116:583–91.
Rojas K, Manasseh DM, Flom PL, Agbroko S, Bilbro N, Andaz C, Borgen PI. A pilot study of a breast surgery Enhanced Recovery After Surgery (ERAS) protocol to eliminate narcotic prescription at discharge. Breast Cancer Res Treat. 2018;171(3):621–6.
Gobbe RM, Hoang HL, Kachniarz B, Orgill DP. Ketorolac does not increase perioperative bleeding: a meta-analysis of randomized controlled trials. Plast Reconstr Surg. 2014;133(3):741–55.
Duttchen KM, Lo A, Walker A, McLuckie D, De Guzman C, Roman-Smith H, Davis M. Intraoperative ketorolac dose of 15 mg versus the standard 30 mg on early postoperative pain after spine surgery: a randomized, blinded, non-inferiority trial. J Clin Anesth. 2017;41:11–5.
Motov S, Yasavolian M, Likourezos A, et al. Comparison of intravenous ketorolac at three single-dose regimens for treating acute pain in the emergency department: a randomized controlled trial. Ann Emerg Med. 2017;70(2):177–84.
Liang X, Liu R, Chen C, Ji F, Li T. Opioid system modulates the immune function: a review. Transl Perioper Pain Med. 2016;1(1):5–13.
Afsharimani B, Cabot P, Parat MO. Morphine and tumor growth metastasis. Cancer Metastasis Rev. 2011;30(2):225–38.
Gupta K, Kshirsagar S, Chang L, Schwartz R, Law PY, Yee D, Hebbel RP. Morphine stimulates angiogenesis by activating proangiogenic and survival-promoting signaling and promotes breast tumor growth. Cancer Res. 2002;62(15):4491–8.
Nestler EJ, Hyman SE, Holtzman DM, Malenka RC. Molecular neuropharmacology: a foundation for clinical neuroscience, 2nd edn. New York: McGraw-Hill Medical, 2009.
Cummings KC, Xu F, Cummings LC, Cooper GS. A comparison of epidural analgesia and traditional pain management effects on survival and cancer recurrence after colectomy: a population-based study. Anesthesiology. 2012;116(4):797–806.
Cata JP, Keerty V, Keerty D, et al. A retrospective analysis of the effect of intraoperative opioid dose on cancer recurrence after non-small cell lung cancer resection. Cancer Med. 2014;3:900–8.
Jiang W, Wang L, Zhang J, et al. Effects of postoperative non-steroidal anti-inflammatory drugs on long-term survival and recurrence of patients with non-small cell lung cancer. Medicine (Baltimore). 2018;97(39):e12442.
Forget P, Vandenhende J, Berliere M, Machiels JP, Nussbaum B, Legrand C, De Kock M. Do intraoperative analgesics influence breast cancer recurrence after mastectomy? A retrospective analysis. Anesth Analg. 2010;110(6):1630–5.
Forget P, Bentin C, Machiels JP, Berliere M, Coulie PG, De Kock M. Intraoperative use of ketorolac or diclofenac is associated with improved disease-free survival and overall survival in conservative breast cancer surgery. Br J Anesth. 2014;113:i82–7.
Retsky M, Demicheli R, Hrushesky W, et al. Reduction of breast cancer relapses with perioperative non-steroidal anti-inflammatory drugs: new findings and review. Curr Med Chem. 2013;20(33):4163–76.
Zhao X, Xu Z, Li H. NSAIDs Use and reduced metastasis in cancer patients: results from a meta-analysis. Sci Rep. 2017;7(1):1875.
Walter ND, Rice PL, Redente EF. Wound healing after trauma may predispose to lung cancer metastasis: review of potential mechanisms. Am J Respir Cell Mol Biol. 2011;44(5):591–6.
Tsujii M, Kawano S, Tsuji S, Sawaoka H, Hori M, DuBois RN. Cyclooxygenase regulates angiogenesis induced by colon cancer cells. Cell. 1998; 93(5):705–16.
Baek SJ, Okazaki R, Lee SH, et al. Nonsteroidal anti-inflammatory drug-activated gene-1 over expression in transgenic mice suppresses intestinal neoplasia. Gastroenterology. 2006;131:1553–60.
Cekanova M, Lee SH, Donnell RL, Sukhthankar M, Eling TE, Fischer SM, Baek SJ. Nonsteroidal anti-inflammatory drug-activated gene-1 expression inhibits urethane-induced pulmonary tumorigenesis in transgenic mice. Cancer Prev Res. 2009;2:450–8.
Sharma S, Chang DW, Koutz C, Evans GR, Robb GL, Langstein HN, Kroll SS. Incidence of hematoma associated with ketorolac after TRAM flap breast reconstruction. Plast Reconstr Surg. 2001;107(2):352–5.
Batdorf NJ, Lemaine V, Lovely JK, et al. Enhanced recovery after surgery in microvascular breast reconstruction. J Plast Reconstr Aesthet Surg. 2015;68(3):395–402.
Mikhaylov Y, Weinstein B, Schrannk TP, Swartz JD, Ulm JP, Armstrong MB, Delaney KO. Ketorolac and hematoma incidence in postmastectomy implant-based breast reconstruction. Ann Plast Surg. 2018; 80(5):472–4.
Acknowledgment
The authors acknowledge the Maimonides Medical Center anesthesiologists and perioperative staff, residents in the Departments of Surgery and Anesthesiology, pharmacists, and the administrative staff of the Brooklyn Breast Center of Maimonides Medical Center. They especially thank Johanna Yu, BSN, RN, Mohamad Hashim MD, Carin Zelkowitz PA-C, Jeffey Jacobs PA-C, and Mary-Ann Myrthil PA-C, whose cooperation and flexibility in implementing and promoting the ERAS protocol was not only beneficial to our study but to our patients.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Dr. P. Borgen and Dr. K. Rojas have received speaker’s honoraria from Pacira Pharmaceuticals, Inc. All other authors report no relevant commercial, financial, consultant, or institutional conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rojas, K.E., Fortes, T.A., Flom, P. et al. Intraoperative Ketorolac Use Does Not Increase the Risk of Bleeding in Breast Surgery. Ann Surg Oncol 26, 3368–3373 (2019). https://doi.org/10.1245/s10434-019-07557-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-07557-8