Abstract
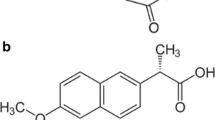
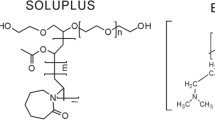
Developing amorphous solid dispersions of water-insoluble molecules using polymeric materials is a well-defined approach to improve the dissolution rate and bioavailability. While the selected polymer plays a vital role in stabilizing the amorphous solid dispersion physically, it is equally important to improve the dissolution profile by inhibiting crystallization from the supersaturated solution generated by dissolution of the amorphous material. Furthermore, understanding the mechanism of dissolution rate enhancement is of vital importance. In this work, wetting kinetics was taken up as an alternative approach for understanding the enhanced dissolution rate for amorphous solid dispersion of a poorly soluble drug. While cilostazol (CIL) was selected as the model drug, povidone (PVP), copovidone, and hypromellose (HPMC) were the polymers of choice. The concentrations against time profiles were evaluated for the supersaturated solutions of CIL in the presence and absence of the selected polymers. The degree of supersaturation increased significantly with increase in polymer content within the solid dispersion. While povidone was found to maintain the highest level of supersaturation for the greatest length of time both in dissolution and solution crystallization experiments, copovidone and hypromellose were found to be the less effective as crystallization inhibitor. The ability of polymers to generate and maintain supersaturated drug solutions was assessed by dissolution studies. The wetting kinetics was compared against the solid dispersion composition to establish a correlation with enhanced dissolution rate.





Similar content being viewed by others
References
Horter D, Dressman JB. Influence of physicochemical properties on dissolution of drugs in the gastrointestinal tract. Adv Drug Deliv Rev. 1997;25:3–14.
Kaushal AM, Gupta P, Bansal AK. Amorphous drug delivery systems: molecular aspects, design and performance. Crit Rev Ther Drug Carrier Syst. 2004;21:133–93.
Chiou WL, Riegelman S. Pharmaceutical applications of solid dispersion systems. J Pharm Sci. 1971;60:1281–302.
Hancock BC, Zografi G. Characteristics and significance of the amorphous state in pharmaceutical systems. J Pharm Sci. 1997;86:1–12.
Serajuddin AM. Solid dispersion of poorly water-soluble drugs: early promises subsequent problems, and recent breakthroughs. J Pharm Sci. 1999;88(10):1058–66.
Leuner C, Dressman J. Improving drug solubility for oral delivery using solid dispersions. Eur J Pharm Biopharm. 2000;50:47–60.
Vo CL, Park C, Lee BJ. Current trends and future perspectives of solid dispersions containing poorly water-soluble drugs. Eur J Pharm Biopharm. 2013;85:799–813.
Craig DQM. Review: the mechanism of drug release from solid dispersions in water-soluble polymers. Int J Pharm. 2002;231:131–44.
Sekiguchi K, Obi N. Studies on absorption of eutectic mixture. I. A comparison of the behaviour of eutectic mixture of sulfathiazole and that of ordinary sulfathiazole in man. Chem Pharm Bull. 1961;9:866–72.
Sekiguchi K, Obi N, Ueda Y. Studies on absorption of eutectic mixtures. II: absorption of fused conglomerates of chloramphenicol and urea in rabbits. Chem Pharm Bull. 1964;12:134–9.
Lakshman JP et al. Application of melt extrusion in the development of a physically and chemically stable high-energy amorphous solid dispersion of a poorly water-soluble drug. Mol Pharm. 2008;5(6):994–1002.
Riikka Laitinen R et al. Emerging trends in the stabilization of amorphous drugs. Int J Pharm. 2013;453:65–79.
Shah S et al. Melt extrusion with poorly soluble drugs. Int J Pharm. 2013;453:233–52.
Paudel A et al. Manufacturing of solid dispersions of poorly water soluble drugs by spray drying: formulation and process considerations. Int J Pharm. 2013;453:253–84.
Baird JA, Taylor LS. Evaluation of amorphous solid dispersion properties using thermal analysis techniques. Adv Drug Deliv Rev. 2012;64:396–421.
Bugay DE. Characterization of the solid-state: spectroscopic techniques. Adv Drug Deliv Rev. 2001;48:43–65.
Tanno F, Nishiyama Y, Kokubo H, Obara S. Evaluation of hypromellose acetate succinate (HPMCAS) as a carrier in solid dispersions. Drug Dev Ind Pharm. 2004;30:9–17.
Huang J, Wigent RJ, Schwartz JB. Drug–polymer interaction and its significance on the physical stability of nifedipine amorphous dispersion in microparticles of an ammonio methacrylate copolymer and ethylcellulose binary blend. J Pharm Sci. 2008;97(1):251–62.
Andrews GP, Abu-Diak O, Jones DS. Physicochemical characterization of hot-melt extruded bicalutamide-polyvinylpyrrolidone solid dispersions. J Pharm Sci. 2010;99(3):1322–35.
Van den Mooter G et al. Physical stabilization of amorphous ketoconazole in solid dispersions with polyvinylpyrrolidone K25. Eur J Pharm Sci. 2001;12:261–9.
Manias E et al. Intercalation kinetics of long polymers in 2 nm confinements. Macromolecules. 2000;33:7955–66.
Park SJ, Jin JS. Effect of silane coupling agent on interphase and performance of glass fibers/unsaturated polyester composites. J Colloid Interface Sci. 2001;242:174–9.
Matteucci et al. Highly supersaturated solutions of amorphous drugs approaching predictions from configurational thermodynamic properties. J Phys Chem B. 2008;112:16675–81.
Shimizu T, Osumi T, Niimi K, Nakagawa K. Physico-chemical properties and stability of cilostazol. Arzneimittelforschung. 1985;35:1117–23.
Toyobuku H, Tamai I, Ueno K, Tsuji A. Limited influence of P-glycoprotein on small-intestinal absorption of cilostazol, a high absorptive permeability drug. J Pharm Sci. 2003;92:2249–59.
Jinno JJ et al. Effect of particle size reduction on dissolution and oral absorption of a poorly water-soluble drug, cilostazol, in beagle dogs. J Control Release. 2006;111:56–64.
Dawson DL. Comparative effects of cilostazol and other therapies for intermittent claudication. Am J Cardiol. 2001;87:19D–27D.
Money SR et al. Effect of cilostazol on walking distances in patients with intermittent claudication caused by peripheral vascular disease. J Vasc Surg. 1998;27:267–75.
Pinnamaneni S, Das NG, Das SK. Formulation approaches for orally administered poorly soluble drugs. Pharmazie. 2002;57:291–300.
Jinno JJ et al. In vitro–in vivo correlation for wet-milled tablet of poorly water-soluble cilostazol. J Control Release. 2008;130:29–37.
Kim MS, Lee S, Park JS, Woo JS, Hwang JS. Micronization of cilostazol using supercritical antisolvent (SAS) process: effect of process parameters. Powder Technol. 2007;177:64–70.
Whittall LB, Whittle RR, Stowell GW. Polymorphic forms of cilostazol. Acta Crystallogr. 2002;C58:525–7.
Stowell GW et al. Thermally-prepared polymorphic forms of cilostazol. J Pharm Sci. 2002;9:2481–8.
Verma S, Rudraraju VS. A systematic approach to design and prepare solid dispersion of poorly water soluble drug. AAPS Pharm Sci Tech. doi:10.1208/s12249-014-0093-z).
Bley H, Fussneggerb B, Roland BR. Characterization and stability of solid dispersions based on PEG/polymer blends. Int J Pharm. 2010;390:165–73.
Eerdenbrugh BV et al. Itraconazole/TPGS/Aerosil®200 solid dispersions: characterization, physical stability and in vivo performance. Eur J Pharm Sci. 2009;38:270–8.
Hancock BC, Parks M. What is the true solubility advantage for amorphous pharmaceuticals? Pharm Res. 2000;17:397–404.
Parks GS, Huffman HM, Cattor FR. Studies on glass. II: the transition between the glassy and liquid states in the case of glucose. J Phys Chem. 1928;32:1366–79.
Parks GS, Snyder LJ, Cattoir FR. Studies on glass. XI: some thermodynamic relations of glassy and alpha-crystalline glucose. J Chem Phys. 1934;2:595–8.
Cirri M et al. Characterization of ibuproxam binary and ternary dispersions with hydrophilic carriers. Drug Dev Ind Pharm. 2004;30(1):65–74.
Ahuja N, Katare OP, Singh B. Studies on dissolution enhancement and mathematical modelling of drug release of a poorly water-soluble drug using water-soluble carriers. Eur J Pharm Biopharm. 2007;65:26–38.
Usui F et al. Inhibitory effects of water-soluble polymers on precipitation of RS-8359. Int J Pharm. 1997;154:59–66.
Gupta P, Kakumanu KV, Bansal AK. Stability and solubility of celecoxib:PVP amorphous dispersions: a molecular perspective. Pharm Res. 2004;21(10):1762–9.
Osama A et al. An investigation into the dissolution properties of celecoxib melt extrudates: understanding the role of polymer type and concentration in stabilizing supersaturated drug concentrations. Mol Pharm. 2011;8:1362–71.
Buckton G. Interfacial phenomena in drug delivery and targeting. Switzerland: Harwood Academic Publishers; 1995.
Ahfat NM et al. An exploration of interrelationships between contact angle, inverse phase gas chromatography and triboelectric charging data. Eur J Pharm Sci. 2000;9:271–6.
Tian et al. Influence of polymorphic form, morphology, and excipient interactions on the dissolution of carbamazepine compacts. J Pharm Sci. 2007;96:584–94.
Buckton G, Beezer AE. A microcalorimetric study of powder surface energetics. Int J Pharm. 1988;41:139–45.
Young SA, Buckton G. Particle growth in aqueous suspensions: the influence of surface energy and polarity. Int J Pharm. 1990;60:235–41.
Conflict of Interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Verma, S., Rudraraju, V.S. Wetting Kinetics: an Alternative Approach Towards Understanding the Enhanced Dissolution Rate for Amorphous Solid Dispersion of a Poorly Soluble Drug. AAPS PharmSciTech 16, 1079–1090 (2015). https://doi.org/10.1208/s12249-014-0281-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1208/s12249-014-0281-x