Abstract
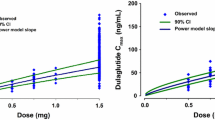
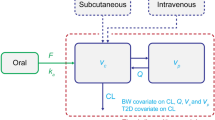
This report describes a pharmacokinetic/pharmacodynamic model for pramlintide, an amylinomimetic, in type 1 diabetes mellitus (T1DM). Plasma glucose and drug concentrations were obtained following bolus and 2-h intravenous infusions of pramlintide at three dose levels or placebo in 25 T1DM subjects during the postprandial period in a crossover study. The original clinical data were reanalyzed by mechanism-based population modeling. Pramlintide pharmacokinetics followed a two-compartment model with zero-order infusion and first-order elimination. Pramlintide lowered overall postprandial plasma glucose AUC (AUCnet) and delayed the time to peak plasma glucose after a meal (T max). The delay in glucose T max and reduction of AUCnet indicate that overall plasma glucose concentrations might be affected by differing mechanisms of action of pramlintide. The observed increase in glucose T max following pramlintide treatment was independent of dose within the studied dose range and was adequately described by a dose-independent, maximum pramlintide effect on gastric emptying of glucose in the model. The inhibition of endogenous glucose production by pramlintide was described using a sigmoidal function with capacity and sensitivity parameter estimates of 0.995 for I max and 23.8 pmol/L for IC50. The parameter estimates are in good agreement with literature values and the IC50 is well within the range of postprandial plasma amylin concentrations in healthy humans, indicating physiological relevance of the pramlintide effect on glucagon secretion in the postprandial state. This model may prove to be useful in future clinical studies of other amylinomimetics or antidiabetic drugs with similar mechanisms of action.






Similar content being viewed by others
REFERENCES
Aronoff SL, Berkowitz K, Shreiner B, Want L. Glucose metabolism and regulation: beyond insulin and glucagon. Diabetes Spectr. 2004;17(3):183–90.
Fineman MS, Koda JE, Shen LZ, Strobel SA, Maggs DG, Weyer C, et al. The human amylin analog, pramlintide, corrects postprandial hyperglucagonemia in patients with type 1 diabetes. Metab Clin Exp. 2002;51(5):636–41.
Gromada J, Franklin I, Wollheim CB. Alpha-cells of the endocrine pancreas: 35 years of research but the enigma remains. Endocr Rev. 2007;28(1):84–116.
Young A. Inhibition of glucagon secretion. Adv Pharmacol. 2005;52:151–71.
Evers F, Jeworrek C, Tiemeyer S, Weise K, Sellin D, Paulus M, et al. Elucidating the mechanism of lipid membrane-induced IAPP fibrillogenesis and its inhibition by the red wine compound resveratrol: a synchrotron X-ray reflectivity study. J Am Chem Soc. 2009;131(27):9516–21.
Konarkowska B, Aitken JF, Kistler J, Zhang S, Cooper GJ. The aggregation potential of human amylin determines its cytotoxicity towards islet beta-cells. FEBS J. 2006;273(15):3614–24.
Green J, Goldsbury C, Mini T, Sunderji S, Frey P, Kistler J, et al. Full-length rat amylin forms fibrils following substitution of single residues from human amylin. J Mol Biol. 2003;326(4):1147–56.
McQueen J. Pramlintide acetate. Am J Health Syst Pharm. 2005;62(22):2363–72.
Edelman SV, Garg S, Kolterman OG. Is pramlintide a safe and effective adjunct therapy for patients with type 1 diabetes? Nat Clin Pract. 2007;3(5):E1. discussion E2.
Hoogwerf BJ. Exenatide and pramlintide: new glucose-lowering agents for treating diabetes mellitus. Cleve Clin J Med. 2006;73(5):477–84.
Chase HP, Lutz K, Pencek R, Zhang B, Porter L. Pramlintide lowered glucose excursions and was well-tolerated in adolescents with type 1 diabetes: results from a randomized, single-blind, placebo-controlled, crossover study. J Pediatr. 2009;155(3):369–73.
Edelman S, Garg S, Frias J, Maggs D, Wang Y, Zhang B, et al. A double-blind, placebo-controlled trial assessing pramlintide treatment in the setting of intensive insulin therapy in type 1 diabetes. Diabetes Care. 2006;29(10):2189–95.
Colburn WA, Gottlieb AB, Koda J, Kolterman OG. Pharmacokinetics and pharmacodynamics of AC137 (25,28,29 tripro-amylin, human) after intravenous bolus and infusion doses in patients with insulin-dependent diabetes. J Clin Pharmacol. 1996;36(1):13–24.
Byon W, Fletcher CV, Brundage RC. Impact of censoring data below an arbitrary quantification limit on structural model misspecification. J Pharmacokinet Pharmacodyn. 2008;35(1):101–16.
Beal SL. Ways to fit a PK model with some data below the quantification limit. J Pharmacokinet Pharmacodyn. 2001;28(5):481–504.
Young A. Inhibition of gastric emptying. Adv Pharmacol. 2005;52:99–121.
Collins PJ, Horowitz M, Cook DJ, Harding PE, Shearman DJ. Gastric emptying in normal subjects—a reproducible technique using a single scintillation camera and computer system. Gut. 1983;24(12):1117–25.
Minami H, McCallum RW. The physiology and pathophysiology of gastric emptying in humans. Gastroenterology. 1984;86(6):1592–610.
Kong MF, King P, Macdonald IA, Stubbs TA, Perkins AC, Blackshaw PE, et al. Infusion of pramlintide, a human amylin analogue, delays gastric emptying in men with IDDM. Diabetologia. 1997;40(1):82–8.
Silber HE, Jauslin PM, Frey N, Gieschke R, Simonsson US, Karlsson MO. An integrated model for glucose and insulin regulation in healthy volunteers and type 2 diabetic patients following intravenous glucose provocations. J Clin Pharmacol. 2007;47(9):1159–71.
Jauslin PM, Silber HE, Frey N, Gieschke R, Simonsson US, Jorga K, et al. An integrated glucose-insulin model to describe oral glucose tolerance test data in type 2 diabetics. J Clin Pharmacol. 2007;47(10):1244–55.
Dalla Man C, Camilleri M, Cobelli C. A system model of oral glucose absorption: validation on gold standard data. IEEE Trans Biomed Eng. 2006;53(12):2472–8.
Dinneen S, Alzaid A, Turk D, Rizza R. Failure of glucagon suppression contributes to postprandial hyperglycaemia in IDDM. Diabetologia. 1995;38(3):337–43.
Bea SB, Broeckmann AJ, Sheiner LB, Group NP. NONMEM users guides. San Francisco, CA: University of California; 2007.
Karlsson MO, Jonsson EN, Wiltse CG, Wade JR. Assumption testing in population pharmacokinetic models: illustrated with an analysis of moxonidine data from congestive heart failure patients. J Pharmacokinet Biopharm. 1998;26(2):207–46.
Bergstrand M, Hooker AC, Wallin JE, Karlsson MO. Prediction-corrected visual predictive checks for diagnosing nonlinear mixed-effects models. AAPS J. 2011;13(2):143–51.
Kong MF, Stubbs TA, King P, Macdonald IA, Lambourne JE, Blackshaw PE, et al. The effect of single doses of pramlintide on gastric emptying of two meals in men with IDDM. Diabetologia. 1998;41(5):577–83.
Lima JJ, Matsushima N, Kissoon N, Wang J, Sylvester JE, Jusko WJ. Modeling the metabolic effects of terbutaline in beta2-adrenergic receptor diplotypes. Clin Pharmacol Ther. 2004;76(1):27–37.
Lee SH, Kwon KI. Pharmacokinetic-pharmacodynamic modeling for the relationship between glucose-lowering effect and plasma concentration of metformin in volunteers. Arch Pharm Res. 2004;27(7):806–10.
Gumbhir-Shah K, Kellerman DJ, DeGraw S, Koch P, Jusko WJ. Pharmacokinetics and pharmacodynamics of cumulative single doses of inhaled salbutamol enantiomers in asthmatic subjects. Pulm Pharmacol Ther. 1999;12(6):353–62.
Brener W, Hendrix TR, McHugh PR. Regulation of the gastric emptying of glucose. Gastroenterology. 1983;85(1):76–82.
Horowitz M, Edelbroek MA, Wishart JM, Straathof JW. Relationship between oral glucose tolerance and gastric emptying in normal healthy subjects. Diabetologia. 1993;36(9):857–62.
Gedulin BR, Rink TJ, Young AA. Dose–response for glucagonostatic effect of amylin in rats. Metab Clin Exp. 1997;46(1):67–70.
Schvarcz E, Palmer M, Aman J, Horowitz M, Stridsberg M, Berne C. Physiological hyperglycemia slows gastric emptying in normal subjects and patients with insulin-dependent diabetes mellitus. Gastroenterology. 1997;113(1):60–6.
Ludvik B, Kautzky-Willer A, Prager R, Thomaseth K, Pacini G. Amylin: history and overview. Diabet Med. 1997;14 Suppl 2:S9–S13.
Singh-Franco D, Robles G, Gazze D. Pramlintide acetate injection for the treatment of type 1 and type 2 diabetes mellitus. Clin Ther. 2007;29(4):535–62.
Landersdorfer CB, He YL, Jusko WJ. Mechanism-based population modelling of the effects of vildagliptin on GLP-1, glucose and insulin in patients with type 2 diabetes. Br J Clin Pharmacol. 2012;73(3):373–90.
Nowak TV, Johnson CP, Kalbfleisch JH, Roza AM, Wood CM, Weisbruch JP, et al. Highly variable gastric emptying in patients with insulin dependent diabetes mellitus. Gut. 1995;37(1):23–9.
Young AA, Gedulin BR, Rink TJ. Dose-responses for the slowing of gastric emptying in a rodent model by glucagon-like peptide (7–36) NH2, amylin, cholecystokinin, and other possible regulators of nutrient uptake. Metab Clin Exp. 1996;45(1):1–3.
Ryan GJ, Jobe LJ, Martin R. Pramlintide in the treatment of type 1 and type 2 diabetes mellitus. Clin Ther. 2005;27(10):1500–12.
Buse JB, Weyer C, Maggs DG. Amylin replacement with pramlintide in type 1 and type 2 diabetes: a physiological approach to overcome barriers with insulin therapy. Clin Diabetes. 2002;20(3):137–44.
Fineman M, Weyer C, Maggs DG, Strobel S, Kolterman OG. The human amylin analog, pramlintide, reduces postprandial hyperglucagonemia in patients with type 2 diabetes mellitus. Horm Metab Res Hormon- und Stoffwechselforschung. 2002;34(9):504–8.
Porksen S, Nielsen LB, Kaas A, Kocova M, Chiarelli F, Orskov C, et al. Meal-stimulated glucagon release is associated with postprandial blood glucose level and does not interfere with glycemic control in children and adolescents with new-onset type 1 diabetes. J Clin Endocrinol Metab. 2007;92(8):2910–6.
Landersdorfer CB, Jusko WJ. Pharmacokinetic/pharmacodynamic modelling in diabetes mellitus. Clin Pharmacokinet. 2008;47(7):417–48.
ACKNOWLEDGMENTS
This work was supported in part by Amylin Pharmaceutical Inc., the UB-Pfizer Strategic Alliance, and NIH Grant GM 57980. We appreciate the seminal PKPD contributions of the late University of Buffalo alumnus, Dr. Wayne Colburn, who initiated modeling of pramlintide PKPD.
Financial Disclosure
Ms. Cirincione is an employee of Amylin Pharmaceuticals, Inc.
Author information
Authors and Affiliations
Corresponding author
Appendices
APPENDIX: NONMEM MODEL FILE FOR THE PRAMLINTIDE PK MODEL

NONMEM MODEL FILE FOR THE PRAMLINTIDE PD MODEL



Rights and permissions
About this article
Cite this article
Fang, J., Landersdorfer, C.B., Cirincione, B. et al. Study Reanalysis Using a Mechanism-Based Pharmacokinetic/Pharmacodynamic Model of Pramlintide in Subjects with Type 1 Diabetes. AAPS J 15, 15–29 (2013). https://doi.org/10.1208/s12248-012-9409-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1208/s12248-012-9409-7