Abstract
Background
Although the outcome of hypospadias repair has much improved, repair of a small-sized phallus is still challenging. Whether preoperative hormonal therapy is beneficial remains controversial.
In this report, we prospectively conducted a clinical trial comparing two groups of patients regarding the effect of preoperative topical testosterone application on the outcome of primary hypospadias repair.
Results
The study included 40 cases of primary hypospadias with a small glans. Their age ranged from 6 months to 3 years. Patients were divided into two equal groups. Group A were treated by local application of testosterone topical gel 1% for 30–40 days and stopped one month before operation, while cases in group B did not receive preoperative hormonal treatment. Genital skin biopsies were taken for histopathological examination. For group A, penile measurements were documented before and after hormonal therapy.
There was a significant increase in all penile parameters after hormonal stimulation in group A. Interestingly, the ventral penile length proximal to the meatus showed more growth in response to hormonal stimulation compared to ventral penile length distal to meatus.
We did not find significant difference between both groups regarding the rate of postoperative complications. Also, the cosmesis and parent satisfaction were ‘more or less’ similar. On the histopathological level, we could not detect a difference between both groups regarding micro-vessel density using CD31, which is a vascular marker indicating neovascularization supposed to play a fundamental role in the healing process.
Conclusion
The use of preoperative topical testosterone significantly increases the size of the hypospadiac phallus. However, this increase in size appears to be disproportionate on the ventral penile surface and has not been reflected on improving the surgical outcome.
Level of evidence
This is a case control study (level III evidence).
Similar content being viewed by others
Background
Hypospadias is one of the most common congenital anomalies, with an incidence of about one in every 250 newborns [1]. Hypospadias represents a wide spectrum of abnormalities involving the inferior surface of the penis and having in common a urethral opening that lies on the inferior surface of the penis [2]. Repair of a small hypospadiac phallus can be technically challenging. Some reports cited that androgen therapy before genital reconstruction improves the cosmetic and surgical results of these demanding operations [3,4,5,6]. On the other hand, others concluded that preoperative testosterone was associated with a higher risk of complications [7, 8]. Whether preoperative hormonal therapy is beneficial remains controversial [9]. Although the outcome of hypospadias repair has much improved, repair of a small-sized phallus is still challenging. The lack of scientific evidence results in the use of empirical judgment when the surgeon is confronted with a small hypospadiac phallus [10].
In this report, we prospectively conducted a clinical trial comparing two groups of patients regarding the effect of preoperative topical testosterone application on the outcome of primary hypospadias repair. Also, we studied the effect of topical testosterone on the penile size and on the histopathology of genital skin biopsies.
Methods
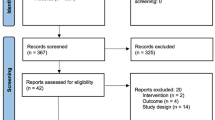
A prospective study was conducted at two tertiary centers of pediatric surgery between December 2013 through September 2015. The study included 40 cases of primary (non recurrent) hypospadias with a small glans (glanular width less than 14 mm). At one extreme end of the spectrum, we excluded scrotal and perineal hypospadias from the study. Patients were divided into two equal groups (20 patients in each group). Cases in the first group (A) were treated by local application of testosterone topical gel 1% for 30–40 days (to increase the size of their phallus) and stopped one month before operation (Fig. 1); while cases in the second group (B) did not receive preoperative hormonal treatment (Fig. 2). During the repair of hypospadias, full-thickness genital skin biopsies (from the inner foreskin) were taken from all cases and preserved in formalin for histopathological examination.
30-month-old boy with proximal hypospadias from the hormonally treated group (group A). a Preoperative appearance after hormonal stimulation. b Intraoperative view for the urethral opening after complete degloving. c, d, and e A dartos flap is prepared as a second layer from half of the dorsal prepuce to cover the urethroplasty. f The other half of the dorsal prepuce is used to reconstruct the deficient ventral penile skin. g and h Follow up 6 months after surgical repair
12-month-old boy with mid penile hypospadias from the ‘untreated’ group (group B). a Preoperative appearance demonstrating the hypospadiac position of the meatus (arrow). b Lateral view. c Catheter passing through meatus. This case was operated by one stage TIP repair without preoperative hormonal therapy. d and e Follow up 6 months after surgical repair demonstrating satisfactory outcome
For group A, penile measurements were documented before and after hormonal therapy (using Castroviejo Caliber 40 mm straight). Penile measurements included glanular width, glanular height, shaft width, ventral penile length proximal to meatus, and ventral penile length distal to meatus. The study was conducted after internal review board approval (IRB 00006379).
Surgical technique
We start by degloving of the penile skin. Assessment of penile curvature (chordee) represents a key step, which should be carried out after complete degloving. Mild to moderate degrees of ventral penile curvature (up to 45 degrees) were managed by dorsal ‘Nesbit’ plication sutures, when a ‘plate-preserving’ technique for hypospadias repair was applied (TIP urethroplasty) [11]. A modified technique utilizing dorsal Byars’ flaps was applied to provide second layer coverage for the urethroplasty from one flap, while the other flap was used to reconstruct the ventral skin (Fig.1) [12]. More severe degrees of chordee were managed by transection of the urethral plate when a staged repair was performed: skin flaps were used to cover the ventral penile shaft in the first stage, and a Theirsh urethroplasty was performed six months later. Trying to neutralize the effect of having different surgeons performing the operations, all cases included in the study were operated by two senior surgeons (A.A.A. and O.E.) with a ‘more or less’ equal contribution in both study groups.
Measuring the outcome
Complications were documented in both groups that included early complications (bleeding, edema, infection), and late complications (glanular dehiscence, fistula, meatal stenosis, urethral stricture). Assessment of all patients was done by the same investigator (the first author I.W.) using digital photography and objective penile evaluation ‘HOPE’ score [13]. Assessment of parents` satisfaction was also performed by Likert scale questionnaires to assess four outcomes: overall penile appearance, cosmesis of meatus, penile size, and voiding stream [14].
Histopathological and immunohistochemical examination
Paraffin blocks of genital skin biopsies from both groups were prepared; Morphometric studies were performed by Olympus Soft Pro Software. Additional four-micrometer-thick sections were cut from the paraffin blocks and were immune-stained for commercially available ready to use mouse monoclonal antibody against four types of antigens: Estrogen Receptor α (Dako, Denmark, Cat.# IR657, Clone 1D5, Ready-to-Use); Estrogen Receptor β1 (Dako, Denmark, Cat.# M7292, Clone PPG5/10, dilution 1:20); Androgen (Dako, Denmark, Cat. # M3562, Clone AR441, dilution 1: 50); and CD31 (Dako, Denmark, Cat. # M0823, Clone JC70A, dilution 1: 40) [15, 16]. The latter (CD31) is a vascular marker indicating neovascularization supposed to play a fundamental role in the healing process [16]. The immune staining was performed using the avidin-biotin complex staining procedure [16]. All slides were examined and evaluated by a single pathologist in a blinded manner to the study groups. The histological findings were then compared in both groups.
Interpretation of immunostaining for Estrogen Receptor α, Estrogen Receptor β1, and androgen was performed. The density of nuclear staining was scored on a subjective grade scale as none (0), weak (+), intermediate (++) or strong (+++) [17]. For assessment of micro-vessel density by CD31 immunostaining, areas with high-density staining were recognized in low-power fields (100×). Most of the micro-vessels with CD31-positivity were identified in these areas with high-density staining, which resembled an “extended hot spot” of angiogenesis. Neovascularity was counted in 5 random high-power fields (200×) within these hot spots. The mean results were documented for analysis [18].
Results
The study included 40 boys with primary hypospadias and a small glans (glanular width less than 14 mm). Their age ranged from 6 months to 3 years (median 15 months; mean 18 months). The position of the meatus ranged from distal penile to penoscrotal. There was a significant increase in all penile parameters after hormonal stimulation in group A (Tables 1, 2). Interestingly, the ventral penile length proximal to the meatus showed more growth in response to hormonal stimulation compared to ventral penile length distal to meatus, denoting a significant disproportionate penile growth (p-value = 0.003).
In group A, 16 cases underwent TIP urethroplasty, while a two-stage repair was performed in four. In group B, 15 cases underwent TIP urethroplasty, and a two-stage repair was performed in five. Patients were instructed to attend follow up after 1 week, 1 month, 6 months, and then yearly until puberty. The follow up period in the study ranged from 6 months to 2 years. Postoperative edema (which may be considered an early postoperative complication) was more evident in group A (7 cases) compared to 2 cases in group B (p = 0.058). There were 4 cases of urethrocutaneous fistula in group A, compared to 5 cases in group B (p = 0.7), one case of glanular dehiscence in each group, and 3 cases of meatal stenosis in group A compared to 2 cases in group B (Table 3). Meatal stenosis showed good response to dilatation in all except one case that required ventral meatotomy. The mean overall HOPE score was 40.75 in group (A) compared to 40.95 in group (B) representing an insignificant difference. Also, parents` satisfaction based on Likert scale satisfaction questionnaire was almost equal in both groups.
Histopatholological evaluation of genital skin biopsies revealed vascularized connective tissue covered by healthy appearing surface epithelium. The subepithelial tissues was formed of connective tissue stroma, collagen, and blood vessels (Fig. 3). Immunohistochemical expression of Estrogen Receptor β was strongly expressed (+++) in the treated group (A) compared to moderate expression (++) in group B; whereas Estrogen Receptor α was weakly expressed (+) in the treated group (A) compared to no expression (0) in group (B) (Fig. 4). On the other hand, androgen immunohistochemical expression was not detected in the treated group (A) compared to weak expression (+) in group (B) (Fig. 5). Regarding CD31 (the vascular marker indicating neovascularization), there was no detectable difference in the micro-vessel density in both groups (Fig. 6).
Genital skin biopsies of hypospadic patients: (a&b) testosterone treated group, (c&d) untreated group. Biopsies showed surface epithelium overlying vascularized connective tissue with mild to moderate increase in the number of the blood vessels in biopsies of treated group as compared to the other untreated group (a&c: Hematoxylin and eosin;original magnification × 100, b&d: Masson’s trichrome stain;original magnification × 100)
Histo-patholological evaluation of genital skin biopsies: immune-staining for commercially available ready to use mouse monoclonal antibody against Estrogen Receptor (ER) α and β. Upper row (a and b): Hormonally treated group (a) showed weak ERα expression (+) that was localized to the stratum basale, in contrast to the ‘untreated’ group (b) that showed no detectable expression (0). (original magnification × 400). Lower row (c and d): ERβ immunoreactivity was strongly expressed in the keratinocytes of the stratum basale and stratum spinosum (+++) in the treated group (c); while in untreated group (d), there was moderate expression (++). (A&B: ERβ, immunoperoxidase; original magnification × 400)
Histo-patholological evaluation of genital skin biopsies: immune-staining for commercially available ready to use mouse monoclonal antibody against CD31 which is a vascular marker indicating neovascularization supposed to play a fundamental role in the healing process. There was an equal mild to moderate expression in both groups: (a) hormonally treated group; (b) the ‘untreated’ group (original magnification × 200)
Discussion
Hypospadias surgery was always regarded as a nonrewarding surgical reconstruction, due to the reported high complication rate and repeated failures. For decades, the use of hormonal stimulation before surgical repair of a small sized phallus has been accepted as a relatively common practice among pediatric urologists and surgeons [3]. The local application of testosterone cream for the prepubertal phallus was first reported in 1971 by Immergut et al., and it was the hormone of choice for many other investigators as well [19].
In this report, we studied the effect of preoperative hormonal treatment on the outcome of hypospadias repair while considering comparison to a control group. In the study group, testosterone gel 1% was applied to the hypospadiac phallus once daily for 30–40 days and stopped 4–5 weeks preoperatively. Topical application of testosterone may be criticized for the less predictable drug dosage and distribution on the penis. However, this protocol was chosen because of easy applicability. Moreover, we were worried about the complications of parenteral testosterone which were unclear while reviewing the literature [20]. Till now, there is no consensus on the protocol for preoperative hormonal stimulation in hypospadias surgery regarding the appropriate dose, frequency, concentration, and route of application.
Although some studies have favored hormonal administration before hypospadias repair [3,4,5,6, 21], other studies addressed increasing rate of healing complications with androgen stimulation [22]. In our study, we did not find significant difference between the hormonally treated and the untreated groups regarding the rate of postoperative complications (urethrocutaneous fistula, glanular dehiscence, meatal stenosis). Also, the cosmesis and parent satisfaction were ‘more or less’ similar among both groups. In other words, the increase in penile size induced by preoperative hormonal stimulation in our study group was not reflected on improving the surgical outcome. The small number of cases and low incidence of complications will make it difficult to obtain a definitive conclusion from a single study. Perhaps a meta-analysis may be a more appropriate solution to overcome this common limitation in all similar studies on hypospadias.
On the histopathological level, we could not detect a difference between the hormonally treated and the untreated groups regarding the micro-vessel density using CD31 immunohistochemical stain. In their report on a larger number of cases (94 patients with distal hypospadias), Menon and colleagues similarly found no significant difference between hormonally treated and untreated groups while using the same vascular marker (CD31). However, they have noticed increased proliferating blood vessels and lymphocytic infiltrates in the treated group on hematoxylin and eosin (H&E) stain [20]. The discrepancy between the results of hematoxylin and eosin (H&E) stain and that obtained by CD31 immunostaining can be explained in view of the different ways of assessment and scoring. In CD31 immunostaining, we only score preputial micro-vessels with CD31-positivity while excluding other vessels. The micro-vessels indicate for neovascularization supposed to play a fundamental role in the healing process [16]. In another study, Bastos and colleagues reported a significant increase in vascular density in the hormonally treated group by using a different vascular marker (von Willebrand’s factor) [6]. The contradicting results between different studies may be attributed to the different methodology and different use of monoclonal antibodies.
In our study, both groups were cases of hypospadias with small glans size. As both groups were matched according to the severity of hypospadias, we would expect similar histopathological results under normal circumstances (no hormonal treatment). However, even when one group was hormonally treated, still we could not detect a difference regarding the micro-vessel immunostaining [20]. Although the increased penile vascularity after hormonal treatment was quite evident at operation (and with conventional H&E staining) [20], yet it appears that this increase may be mainly congestion at the level of larger vessels with no actual increase of the micro-vessels as seen by immunohistochemical staining (CD31) [20]. The biopsies were taken at time of operation one month after stopping testosterone; this might have resulted in regression of the hormonal effect on micro-vessels. However, most surgeons would not operate directly after cessation of hormonal treatment, but rather would wait for a similar period.
It is worth mentioning that androgen and estrogen hormones play an important role in the prenatal and postnatal development of urogenital tract specifically the external genitalia [23]. Therefore, immunohistochemical expression of Estrogen and androgen receptors was investigated in our study. A difference between both studied groups was detected regarding the androgen and estrogen receptor immunohistochemical expression. However, the significance and interpretation of this effect remains unclear. As it might be expected, preoperative testosterone treatment has caused an up-regulation effect on the estrogen receptors that showed higher expression in specimens from hormonally treated group, while a down-regulation effect was detected on the androgen receptors. Dominant expression of estrogen receptors in the tissues of hypospadiac phallus has been previously reported by Celayir and colleagues [23]. The disrupted interactions between estrogen and androgen receptors during the intrauterine development of external genitalia might be related to the etiology of hypospadias [23]. However, further studies on a wider scale on patients with hypospadias are needed to clarify and confirm these observations.
The increase in the size of the phallus in response to preoperative hormonal stimulation is a well-known fact among surgeons who practice hypospadias repair. In our study, we tried to provide a quantitative description for this increase in size. Interestingly, we could identify a disproportionate response to hormonal stimulation on the ventral aspect of the hypospadiac phallus. The ventral penile length proximal to the hypospadiac meatus increased by a greater proportionate compared to the ventral penile length distal to the meatus. This was found to be statistically significant. Although this might be interpreted as a beneficial effect for the hormonal treatment by inducing a relative distal displacement of the hypospadiac meatus, yet we may have a different interpretation. It seems that the urethral plate and spongiosum distal to the meatus are keeping some degree of hypoplasia that is manifested by a poorer response to hormonal stimulation compared to normal urethra and spongiosum proximal to meatus. Baskin reported a normal anatomy of the hypospadiac penis except on its ventral aspect with the possibility of biological and structural defects [24]. In proximal hypospadias, a greater proportion of the penile ventrum is formed by the open urethral plate and hypoplastic spongiosum. In such cases, a suboptimal growth of the penile ventrum may be expected to accompany the increase in hormone levels at puberty. This can explain the recurrence of ventral penile curvature that is noticed among some of these cases who were treated by a plate preserving technique during childhood.
Persistence or recurrence of chordee after hypospadias repair may present an under-reported complication in the literature that can cause significant functional problems [25]. This complication is more common after the repair of proximal hypospadias with a plate preserving technique [25]. Recent reports have raised more attention to the importance of proper management of chordee during hypospadias repair. Authors are being more liberal to sacrifice the urethral plate in favor of correction of ventral penile curvature. Recent recommendations highlighted that only mild degrees of ventral penile curvature (less than 30°) can be managed by a plate preserving technique [26].
The study is limited by the small sample size as well as presence of different grades of hypospadias; however, we have tried as much as we can to decrease the multiple confounding factors that may affect the results of any study on hypospadias. This was achieved through including a relatively homogenous group of hypospadias cases (small glans) and unifying the operators’ experience and techniques as much as possible. Another limitation was the lack of research through the etiology of small glans. Some cases might have been partial androgen insensitivity syndrome or 5-alpha reductase deficiency that may constitute a bias in the homogeneity of the sample. Lastly, although the preoperative hormonal stimulation has generally increased the size of the phallus, yet this was not reflected on improving the outcome.
Conclusion
The use of preoperative topical testosterone significantly increases the size of the hypospadiac phallus; however, this increase in size appears to be disproportionate on the ventral penile surface. Although we did not detect a significant difference regarding the surgical outcome among the hormonally treated group, yet the small sample size and the low incidence of complications would make it difficult to reach a definitive conclusion in this respect.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- MRI:
-
Magnetic resonance imaging
- CAH:
-
Congenital adrenal hyperplasia
- PACS:
-
Picture Archiving and Communication System
- H&E:
-
Hematoxylin and eosin
References
Paulozzi LJ. International trends in rates of hypospadias and cryptorchidism. Environ Health Perspect. 1999;107:297.
Hadidi AT. Principles of hypospadias surgery. In: Hadidi AT, Azmy AF. Hypospadias surgery: an illustrated guide, 1st ed. Springer Verlag, 2004, 541.
Snodgrass W, Macedo A, Hoebeke P, et al. Hypospadias dilemmas: a round table. J Pediatr Urol. 2011;7:145–57.
Asgari SA, Safarinejad MR, Poorreza F, et al. The effect of parenteral testosterone administration prior to hypospadias surgery: a prospective, randomized and controlled study. J Pediatr Urol. 2015;11:143 e1-e6.
Koff SA, Jayanthi VR. Preoperative treatment with human chorionic gonadotropin in infancy decreases the severity of proximal hypospadias and chordee. J Urol. 1999;162:1435–9.
Bastos AN, Oliveira LR, Ferrarez CE, et al. Structural study of prepuce in hypospadias: does topical treatment with testosterone produces alterations in prepuce vascularization? J Urol. 2011;185:2474e8.
Gorduza DB, Gay CL, de Mattos SE, et al. Does androgen stimulation prior to hypospadias surgery increase the rate of healing complications? A preliminary report. J Pediatr Urol. 2011;7:158e61.
Baskin LS. Hypospadias and urethral development. J Urol. 2000;163:951.
Douglas A. Editorial: microphallic hypospadias- the use of human chorionic gonadotropin and testosterone before surgical repair. J Urol. 1999;162:1440–1.
Baskin L, Duckett J. Hypospadias: long term outcomes. In: Mouriquand PED, editor. Pediatric surgery and urology, long-term outcome. London: WB Saunders; 1998. p. 559.
Snodgrass W, Koyle M, Manzoni G, et al. Tubularized incised plate hypospadias repair for proximal hypospadias. J Urol. 1998;159:2129–31.
AbouZeid AA. Modified Byars’ flaps for securing skin closure in proximal and mid-penile hypospadias. Ther Adv Urol. 2011;3(6):251–6.
van der Toorn F, de Jong TPVM, de Gier RPE, et al. Introducing the HOPE (hypospadias objective penile evaluation)-score: a validation study of an objective scoring system for evaluating cosmetic appearance in hypospadias patients. J of Pediatr Urol. 2013;9:1006–16.
Snodgrass W, Ziada A, Yucel S, Gupta A. Comparison of outcomes of tubularized incised plate hypospadias repair and circumcision: a questionnaire-based survey of parents and surgeon. J of Pediatr Urol. 2008;4:250–4.
Hsu SM, Raine L, Fanger H. Use of avidin-biotin-peroxidase complex (ABC) in immunoperoxidase techniques: a comparison between ABC and unlabeled antibody (PAP) procedures. J Histochem Cytochem. 1981;29:577–80.
Savas MC, Kapucuoglu N, Gursoy K, Baspinar S. The microvessel density of the hypospadiac prepuce in children. J Pediatr Urol. 2011;7:162–5.
Qiao L, Rodriguez E, Weiss DA, et al. Expression of estrogen receptor alpha and Beta is decreased in hypospadias. J Urol. 2012;187:1427–33.
Savas MC, Baspinar S, Duman L, Kapucuoglu FN. The efficacy of topical testosterone treatment on preputial microvessel density in distal hypospadias. Turk J Med Sci. 2012;42:1454–7.
Immergut M, Boldus R, Yannone E, Bunge R, Flocks R. The local application of testosterone cream to the prepubertal phallus. J Urol. 1971;105:905–6.
Menon P, Rao KLN, Handu A, et al. Outcome of urethroplasty after parenteral testosterone in children with distal hypospadias. J Pediatr Urol. 2017;13:292 e1-292.e7.
Kaya C, Bektic J, Radmayr C, et al. The Efficacy of Dihydrotestosterone Transdermal Gel Before Primary Hypospadias Surgery: A Prospective, Controlled, Randomized Study. J Urol. 2008;179:684–8.
Gorduza DB, Gay CL, Silva E, et al. Does androgen stimulation prior to hypospadias surgery increase the rate of healing complications? E a preliminary report. J Pediatr Urol. 2011;7:158–61.
Celayir S, Elic¸evik M, Tireli G, et al. Expression of estrogen and androgen receptors in children with hypospadias: preliminary report. Arch Androl 2007; 53: 83–85.
Baskin LS, Ebbers MB. Hypospadias: anatomy, etiology, and technique. J Pediatr Surg. 2006;41:463–72.
AbouZeid AA. Tubularized incised plate Urethroplasty for primary hypospadias repair: versatility versus limitations. Journal of Genital Surgery, 2019; 1(Ready articles): 1–9. doi: https://doi.org/10.21608/jgs.2017.1114.1000.
Castagnetti M, El-Ghoneimi A. Surgical management of primary severe hypospadias in children: systematic 20-year review. J Urol. 2010;184:1469–75.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors have read and approved the manuscript. Study conception and design: Wali IM, Radwan NA, El-Naggar O. Data acquisition Wali IM, Radwan NA, GadAllah MA, Ghanem WA. Analysis and data interpretation: AbouZeid AA, Wali IM, GadAllah MA, Ghanem WA. Drafting of the manuscript: Wali IM, Radwan NA. Critical revision: AbouZeid AA, El-Nagger O.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
A written parental consent was taken before operation in all cases. The study was conducted after internal review board approval (IRB 00006379)(Surgery department; Faculty of medicine; Ain-Shams University).
Consent for publication
Patient identity did not appear in any part of the manuscript; therefore, consent for publication was not required.
Competing interests
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wali, I.M., AbouZeid, A.A., Radwan, N.A. et al. Preoperative topical testosterone for penile hypospadias repair `a comparative study`. Ann Pediatr Surg 16, 38 (2020). https://doi.org/10.1186/s43159-020-00050-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43159-020-00050-y