Abstract
Background
Excessive angiogenesis can be the root cause of many pathological conditions. Various types of ion channels are found on the endothelial cells. These ion channels play a vital role in the multi-stepped process of angiogenesis. The study aims to investigate the anti-angiogenic effects of specific ion channel modulators mefloquine (volume-regulated chloride channel blocker), lubiprostone (ClC-2 channel agonist), and 4-aminopyridine (voltage-gated potassium channel blocker).
Results
The anti-angiogenic activity of ion channel modulators was screened by measuring its effects on the area of neovascularization and histopathological studies by in vivo (corneal neovascularization) method and by in vitro assays, endothelial cell proliferation assay, cell migration assay, and matrigel cord-like morphogenesis assay. The test and standard drug (bevacizumab) groups were compared with the control group using one-way ANOVA, followed by post hoc test, and Dunnett’s test to compare the mean of all the groups with the control mean. The results revealed that mefloquine at the dose of 0.6% w/v and 1.0% w/v, lubiprostone at the dose of 0.5% w/v and 1.0% w/v, and 4-aminopyridine at the dose of 2% w/v and 4% w/v showed significant anti-angiogenic property. In the studies on human umbilical vein endothelial cells, the test drugs (100 nM) showed significant inhibition of proliferation, migration, and decrease in network length of cord-like tubes.
Conclusion
The scientific findings indicate that the test drugs have potent anti-angiogenic activity by inhibiting the cell proliferation, inhibiting the cell volume increase, arresting the cell cycle progression and by causing membrane hyperpolarization. The potent anti-angiogenic drugs obtained by repurposing these ion channel modulators, in the further studies, will be able to treat the diseases due to excess angiogenesis from the root cause.
Graphical abstract

Similar content being viewed by others
Background
Tumor angiogenesis was extensively studied by Judah Folkman, the pioneer in the area of angiogenesis at the beginning of the 1970s. Angiogenic switch refers to the equilibrium between the levels of angiogenic and angiostatic factors. Alterations in this equilibrium cause either excess or reduced proliferation of vascular endothelial cells (ECs), leading to various disease conditions [1]. Neurovascularization, which is the primary cause of blindness in diabetic retinopathy, is the main feature of various eye disorders [2, 3]. Proliferative diabetic retinopathy (PDR) is primarily characterized by the excessive generation of leaky blood vessels that spread unevenly on the retinal surface, leading to hemorrhage, fibrosis, and tractional retinal detachment. Compared to other conditions, macular degeneration is said to be the key cause responsible for the formation of new choroidal vessels. This, when left untreated, leads to diabetic retinopathy (DR) and vision loss. DR refers to a clinical condition characterized by abnormal retinal vessels. Vascular endothelial growth factor (VEGF) plays a vital role in the promotion of angiogenesis in both retinal and choroidal blood vessels. High levels of VEGF in eyes were found in diabetic patients. The above discovery became the main foundation for conducting research to find the potential effect of VEGF in the pathophysiology of PDR [4, 5]. Blockade of the development of new blood vessels may be a good approach in the treatment of diseases that are caused due to excess angiogenesis [6, 7].
Corneal endothelium plays a vital role in the propagation of signals, resulting in multicellular functioning. It regulates various vascular processes like blood flow control, blood pressure, clotting of blood, blood vessel permeability, wound healing, and angiogenesis. Interestingly, various types of ion channels are expressed in the ECs. Ion channels can be defined as the pore-forming cell membrane proteins, which play a significant role in many physiological processes like cell volume, muscle constriction, neural depolarization, hormonal release, etc. Various ion channels like sodium (Na+), calcium (Ca2+), potassium (K+), and volume-regulated anion channels (VRAC), are recognized on the surface of ECs. Recently, the occurrence and functional role of vascular ion channels in angiogenesis has been investigated [8,9,10,11]. Corneal endothelial angiogenesis model is a valuable means to study neovascularization mechanism and evaluate the treatment. Anti-angiogenic agents selectively target branching blood vessels and, hence, find use in the treatment of various diseases that occur due to excess angiogenesis. This study aims at pinpointing the exact function of these specific ion channel modulators in anti-angiogenesis which can be the basis for further studies to repurpose the role of channel modulators in anti-angiogenic therapy.
Methods
Chemicals
Bevacizumab, mefloquine, lubiprostone, and 4-aminopyridine were purchased from Sigma-Aldrich Pvt. Ltd. All the other chemicals (AgNO3, KNO3, ethanol, 10 % formalin, hematoxylin, eosin, methylcellulose, sodium pentobarbitone) used in the research are of AR grade.
Experimental animals
Experimental animals and maintenance
Wistar rats weighing in between 150 and 200 g were purchased from Teena Labs Pvt. Ltd., Hyderabad, India. The animals were maintained at a controlled temperature (22–25 °C, 45% humidity) on a 12:12-h dark-light cycle. All the procedures were performed according to the CPCSEA under a protocol approved by the Institutional Animal Ethics Committee (IAEC) with project license numbers (CPCSEA/1657/IAEC/CMRCP/PhD-15/42).
Selection of drugs
Endothelium expresses a huge variety of ion channels, and these ion channels regulate the crucial steps which result in angiogenesis. Thus, in the present research work, specific ion channel agonists and antagonists like mefloquine (volume-regulated chloride channel blocker), lubiprostone (ClC-2 channel agonist), and 4-aminopyridine (voltage-gated potassium channel blocker) have been selected to evaluate their anti-angiogenic effect.
Corneal neovascularization method
Corneal neovascularization (stromal neovascularization) is the ingrowths of blood vessels from the limbus in the corneal stroma. Because the normal stroma is avascular, stromal neovascularization is always considered a pathologic response. The response of the antiangiogenic drugs is evaluated based on the above principal. This technique was carried out by cauterizing the right cornea of every rat with 75% silver nitrate and 25% potassium nitrate, and the left eye served as the control for all animals in all the groups. The rats were cauterized by pressing an applicator stick with a diameter of 1.5 mm, on the center of the cornea for 5 s while the animal is deeply anesthetized with cocktail of ketamine (80 mg/kg) and xylazine (5 mg/kg). After the animals recovered from the anesthesia, the degree of burn was checked by a scoring method. To increase the reproducibility of the injuries, the same investigator cauterized all the animals. Following the procedure for determining the burn score, the rats were randomized to eliminate potential bias in the degree of injury within the different groups; six animals were used in each group. Test and standard drugs were given as eye drops from day 1 to day 13 as 20 μl drop three times a day (Table 1). To make the solution viscous to about 25–50 cps, which is the ideal viscosity range for eye drops, 1% methylcellulose was added. On the 14th day, percentage inhibition of neovascularization was seen after enucleating the animals. Rats were anesthetized and sacrificed; the eyes were removed to check for inhibitory effect [12].
Procedure for determining burn score
The applicator stick was dipped in a solution of 75% AgNO3 and 25% KNO3, and the tip of the stick was superficially touched over the cornea for about 8–10 s and the burn score was estimated.
Burn score:
- 0.
No blister on the cornea
- 1.
1 mm blister on the cornea
- 2.
2 mm blister on the cornea
- 3.
Very big blister on the cornea
The eyes showing a burn score of 0–1 were selected [13].
Calculation of drug concentrations and preparation of drug solutions
The drug concentrations were expressed as % w/v. The therapeutic human range of each drug in the topical or ocular route was obtained from the literature, and three animal doses were calculated by the formula
where
Rat surface area = 0.025 m2
Human surface area = 1.6 m2
First, the highest concentration of each drug was prepared, and then, the other concentrations were prepared from the earlier by serial dilutions. (As an example, in the case of mefloquine, 10 mg of the drug was weighed and dissolved in normal saline to obtain a concentration of 10 mg/ml or 1% w/v. And for the drug insoluble in normal saline, 100 μl of dimethyl sulfoxide (DMSO) was used to dissolve the drug, and then, the final volume was made up with normal saline) (Table 1)
Endothelial cell culture
Human umbilical vein endothelial cells (HUVECs) were grown on gelatinized dishes in M199 supplemented with 15% fetal calf serum, 50 U/ml penicillin, 50 mg/ml streptomycin, 50 mg/ml gentamycin, 2.5 mg/ml amphotericin B, 5 U/ml heparin, and 150–200 mg/ml endothelial cell growth supplement. Cells were used between passages 1 and 3. Each experiment shown derives from three independent repeats, each time using different pools (isolates) and/or passages of cells [14]. In the endothelial cell proliferation assay, Matrigel cord-like morphogenesis assay, and transwell migration assay, the concentration of the bevacizumab is 1 μM, VEGF 500 pM, and mefloquine, lubiprostone, 4-aminopyridine 100 μM each.
Endothelial cell proliferation assay
The HUVECs were seeded in 24-well plates at a density of 6000 cells/cm2 and incubated overnight in Dulbecco’s modified Eagle’s medium. Cells were exposed to different concentrations of bevacizumab, VEGF, and vehicle or test and allowed to proliferate for 48 h. At the end of this incubation time, the cells were trypsinized, and their number was determined using a Neubauer hemocytometer [15].
Matrigel cord-like morphogenesis assay
The formation of cord-like structures by endothelial cells (HUVECs) was assessed in growth factor-reduced Matrigel. The cell groups were plated in 96-well plates precoated with 45 ml of Matrigel per well. After 8 h of incubation, cord-like structure formation was quantified. One image per well was analyzed and used for the statistical analysis [15, 16].
Transwell migration assay
The capacity of endothelial cells to migrate through a pore-bearing membrane was assessed using 6.5-mm-diameter Transwell chambers with polycarbonate membrane inserts (8 mm pore size). Control or endothelial cells were serum-starved overnight. Cells were trypsinized, and 1 × 105 cells were added to each transwell in 100 ml of serum-free medium containing 0.2% bovine serum albumin in the control and in the presence of bevacizumab, VEGF, and test drugs. Cells were allowed to migrate for 4 h, after which the non-migrated cells at the top of the Transwell filter were removed with a cotton swab. The migrated cells on the bottom side of the filter were fixed in Carson’s solution for 30 min at room temperature and then were stained with toluidine blue. Migrated cells were scored and averaged from eight random fields per transwell as previously described elsewhere [17].
Statistical analysis
The statistical analysis was carried out by using GraphPad Prism 5. Results were presented as mean ± SEM. The differences between the groups were compared by one-way ANOVA followed by post hoc Dunnett’s test. In the statistical analysis, all the groups were compared with the control group. Results were considered statistically significant at a p value ˂ 0.05. In all the groups, n = 6. ***p < 0.001, **p < 0.01, *p < 0.05 vs control, ns non-significance.
Results
The results revealed a significant anti-angiogenic effect of all the test drugs. Mefloquine-treated groups at the dose of 0.6% w/v and 1.0% w/v, lubiprostone at the dose of 0.5% w/v and 1.0% w/v, and 4-aminopyridine at the dose of 2% w/v and 4% w/v were observed in the corneal neovascularization assay. A noticeable reduction in proliferation and a very sharp reduction in migration and in network length of cord-like tubes were observed with the test drugs at 100 nM in the studies on human umbilical vein endothelial cells.
Results of corneal neovascularization
Area of neovascularization was quantified, and histopathology of the cornea was examined in the corneal neovascularization method. In the histopathology of the control group, marked corneal thickness, inflammatory cell infiltration, irregular hypertrophy of the cornea, and epithelial ulceration can be seen clearly. Bevacizumab group showed almost normal aspects of the cornea, and in the test drug treatment groups, there was a dose-dependent increase in the anti-angiogenic effect, thus decreasing the infiltration of inflammatory cells and the other aspects of the corneal injury (Table 2, Figs. 1 and 2).
Graph representing the effect of standard and test groups on area CNV. Results were presented as mean ± SEM. The differences between the groups were compared by one-way ANOVA followed by post hoc Dunnett’s test. In all the groups, n = 6. ***p < 0.001, **p < 0.01, *p < 0.05 vs control, ns non-significance
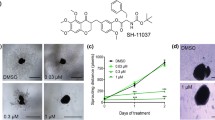
Results of endothelial cell proliferation assay, cord-like morphogenesis assay, and transwell Matrigel assay
Potassium and chloride channels are crucial for cell proliferation, migration, and cord-like network formation on endothelium. To further test the link between channel inhibition and anti-angiogenesis, endothelial cell-based assays triggering proliferation and mobilization were performed. In the cell proliferation assay, VEGF resulted in elevated proliferation (an increase of 49%), whereas bevacizumab showed significant inhibition of proliferation (inhibition by 50%) and the test drugs mefloquine, lubiprostone, and 4-aminopyridine showed inhibition respectively of 69.5, 80, and 60%. To further assess the anti-angiogenic property of the test drugs, migration and cord-like tube formation assay were performed. Significant inhibition was observed with the test doses of 65.8% (mefloquine), 79.3% (lubiprostone), and 58.3 %(4-aminopyridine) (Figs. 3 and 4).
Endothelial cell response to VEGF, bevacizumab, and ion channel modulators. a Cell proliferation was determined by cell counting with a hemocytometer. b Representative images of tube formation after being treated with ion channel modulators for 2 h following VEGF stimulation. c Quantitative data of migrated cells in HUVECs treated with the standard and test drugs for 24 h under VEGF stimulation
Graphs showing the effect of ion channel modulators on a proliferation assay, b Matrigel cord-like morphogenesis assay, and c transwell migration assay. Results were presented as mean ± SEM. The differences between the groups were compared by one-way ANOVA followed by post hoc Dunnett’s test. In all the groups, n = 6. ***p < 0.001, **p < 0.01, *p < 0.05 vs control, ns non-significance
Discussion
Cell proliferation requires an increase in cell volume, and this is accomplished with the help of membrane ion channels [18]. Chloride (Cl−) channels regulate osmolyte flux and thus affect cell volume. On this scientific basis, a VRAC blocker, mefloquine, was studied for its ability to inhibit angiogenesis.
Cell division involves an increase in cell cytoplasmic content, cell volume and Cl− channels play a vital role in cell proliferation, migration, and proteolysis. Cl− ions help in increasing the cytoplasmic volume by regulating osmosis. Action potential regulated by VRAC controls cell cycle mainly by controlling the Ca+2 driving force. This in turn regulates cell proliferation by secondary messengers [19, 20]. Cl− ions also play a significant role in cell migration which is a key step in angiogenesis. Ras, which is a small G-protein molecule, involves in the regulation of large intracellular signaling pathways which influence cell proliferation and motility. As Ras is expressed by Cl− channels, blockade of these channels result in the inhibition of cell proliferation and migration, which are the major steps in angiogenic mechanism. Free radicals mainly cause oxidative damage of endothelium of blood vessels, resulting in endothelial dysfunction which is the main cause of various disease conditions [21]. Chemical burn causes the formation of free radicals, which in turn provokes angiogenesis.
Mefloquine, which is an antioxidant and free radical scavenger, protects the endothelium from oxidative stress independent of anti-angiogenic activity [22]. So, these could be the apparent mechanisms of mefloquine in the prevention of proliferation and thus the associated angiogenesis.
Lubiprostone is an endothelial chloride ion channel opener (ClC-2), which causes increased Cl− ion entry into the lumen of the blood vessels. This results in the hyperpolarization of the endothelial membrane and shows inhibitory action, leading to anti-angiogenesis. ClC family consists of ClC-1, ClC-2, and ClC-3, which are now considered as candidates of VRACs. Only a minimum amount of research work was conducted on biophysical and therapeutic role of ClC-2 channels in mammals. ClC-2 channels are situated on the epithelium of the intestine, airways, on cardiovascular tissue, and corneal endothelium [18, 23,24,25]. They play a key role in the fluid movement in the tracheal, corneal, and intestinal epithelium. Transport of fluids and electrolytes at the epithelia which require Cl− secretion is critical for fluid and electrolyte transport at the epithelia. Biomolecular studies revealed that ClC-2 channels are located on corneal endothelium as stromal hydration maintenance which mainly depends on transendothelial anion transport with bicarbonate-chloride being the chief anions carrying the current [26]. When compared to ClC-1 and ClC-3, ClC-2 is majorly volume-regulated with different therapeutic properties. It was investigated that lubiprostone causes a considerable dose-dependent blockade of both corneal neovascularization and branching. Based on our investigations, the opening of ClC-2 opposes angiogenesis. This is because the chloride secretion due to the ClC-2 opening prevents depolarization. In many mammalian cells, including the endothelial cells, chloride secretion arrests the cell cycle in the G1 phase. Thus, activation of ClC-2 inhibits cell proliferation, which is a major step in angiogenesis.
The four structurally different K+ channel subfamilies involved in cancer pathophysiology are voltage-gated (Kv), calcium-activated (KCa), inwardly rectifying (Kir), and two-pore-domain (background (K2P) “leak”) channels. Compared to other types, Kv channels are extensively involved in tumor mechanisms. K+ channels consist of 77 genes encoding it [27, 28], and they are the most frequently upregulated channels in malignant cells [29, 30]. Kv channels are not located in organs other than the central nerves but are expressed in about 70% of tumors. Hence, 4-aminopyridine, a specific Kv blocker, can target the tumor cells without affecting the normal cells, reducing the side effects.
- 4-
Aminopyridine causes anti-angiogenesis by blocking the Kv channels, which play a major role in the progression of the cell cycle. Ca+2 signaling is mainly required for G1 phase progression and G1/S and G2/N transition in various cells. K+ channels, Ca+2 influx, and action potential are related in such a way that the membrane hyperpolarization produced by K+ channel activation stimulates Ca+2 entry leading to the activation of Ca+2-dependent factors resulting in the expression of cell cycle-regulated proteins, like cyclins, leading to cell proliferation [31,32,33]. Hence, blockade of Kv channel inhibits Ca+2 entries. 4-Aminopyridine, at the doses of 2% w/v and 4% w/v showed significant results in the corneal neovascularization method [21, 34].
Mefloquine is a volume regulatory anion (Cl−) channel blocker, while lubiprostone is a chloride channel opener (ClC-2). The anti-angiogenic potential of both the ion channel modulators has been screened. Interestingly, both the modulators have shown good anti-angiogenic potential. Specific voltage-gated potassium channel blocker like 4-aminopyridine can be used to treat such diseases where Kv channels are upregulated.
In our earlier study on mefloquine and 4-aminopyridine, anti-angiogenic property was proved by various other models such as in vivo (sponge implantation method), in vitro (aortic ring assay), and in ovo (CAM, chick chorioallantoic membrane) methods as described by Kamili et al. [35]. The evaluating parameters described the negative regulation of cell volume, cell migration, and proliferation of blood vessels. Based on these scientific findings, further very specific antiangiogenic models were selected in this study to reconfirm their anti-angiogenic activity.
Therefore, the drugs selected can be considered as good chemical templates that can be modified structurally for more site-specific actions in anti-angiogenic therapy.
Conclusion
The ion channel modulators used in the study have shown good anti-angiogenic action. The results of the study will be very useful in developing cost-effective anti-angiogenic compounds when compared with bevacizumab. Molecular modifications of the ion channel modulators used in the present study will evolve endothelial cell-targeted chemical moieties, and this enables treating the disease from the root cause. Furthermore, these endothelial targeted chemical moieties can be formulated suitably to achieve a site-specific action which minimizes the side effects.
Availability of data and materials
The authors are ready with all the supporting data and materials to support the results of the research.
Abbreviations
- EC:
-
Endothelial cells
- CNV:
-
Corneal neovascularization
- DMSO:
-
Dimethyl sulfoxide
- PDR:
-
Proliferative diabetic retinopathy
- DR:
-
Diabetic retinopathy
- VEGF:
-
Vascular endothelial growth factor
- VRAC:
-
Volume-regulated anion channels
- HUVECs:
-
Human umbilical vein endothelial cells
References
Adair TH, Montani JP (2010) Angiogenesis. In colloquium series on integrated systems physiology: from molecule to function Oct 2 (Vol. 2, No. 1, pp. 1-84). Morgan & Claypool Life Sciences
Tahergorabi Z, Khazaei M (2012) A review on angiogenesis and its assays. Iran J Basic Med Sci 15(6):1110–1126
Deryugina EI, Quigley JP (2015) Tumor angiogenesis: MMP-mediated induction of intravasation-and metastasis-sustaining neovasculature. Matrix Biol 44:94–112
Yadav UC, Srivastava SK, Ramana KV (2012) Prevention of VEGF-induced growth and tube formation in human retinal endothelial cells by aldose reductase inhibition. J Diabetes Complicat 26(5):369–377
Stephenson JA, Goddard JC, Al-Taan O, Dennison AR, Morgan B (2013) Tumour angiogenesis: a growth area—from John Hunter to Judah Folkman and beyond. J Cancer Res 2013
Wang Z, Dabrosin C, Yin X, Fuster MM, Arreola A, Rathmell WK, Generali D, Nagaraju GP, El-Rayes B, Ribatti D, Chen YC (2015) Broad targeting of angiogenesis for cancer prevention and therapy. Semin Cancer Biol 35:S224–S243 Academic Press
Cao Y (2010) Adipose tissue angiogenesis as a therapeutic target for obesity and metabolic diseases. Nat Rev Drug Discov 9(2):107–115
Munaron L (2015) Systems biology of ion channels and transporters in tumor angiogenesis: an omics view. Biochim Biophys Acta Biomembr 1848(10):2647–2656
Nilius B, Droogmans G (2001) Ion channels and their functional role in vascular endothelium. Physiol Rev 81(4):1415–1459
Arcangeli A, Becchetti A (2010) New trends in cancer therapy: targeting ion channels and transporters. Pharmaceuticals 3(4):1202–1224
Laschke MW, van Oijen AE, Scheuer C, Menger MD (2011) In vitro and in vivo evaluation of the anti-angiogenic actions of 4-hydroxybenzyl alcohol. Br J Pharmacol 163(4):835–844
Gupta P, Arumugam M, Azad RV, Saxena R, Ghose S, Biswas NR, Velpandian T (2014) Screening of antiangiogenic potential of twenty two marine invertebrate extracts of phylum Mollusca from South East Coast of India. Asian Pac J Trop Biomed 4:S129–S138
Geer JJ, Dooley DJ, Adams ME (1993) K+-stimulated Ca+ flux into rat neocortical mini-slices is blocked by ω-Aga-IVA and the dual Na+/Ca+ channel blockers lidoflazine and flunarizine. Neurosci Lett 158:97–100
Su M, Huang J, Liu S, Xiao Y, Qin X, Liu J, Pi C, Luo T, Li J, Chen X, Luo Z (2016) The anti-angiogenic effect and novel mechanisms of action of combretastatin A-4. Sci Rep 6:28139
Pyriochou A, Tsigkos S, Vassilakopoulos T, Cottin T, Zhou Z, Gourzoulidou E, Roussos C, Waldmann H, Giannis A, Papapetropoulos A (2007) Anti-angiogenic properties of a sulindac analogue. Br J Pharmacol 152(8):1207–1214
Papapetropoulos A, Pyriochou A, Altaany Z, Yang G, Marazioti A, Zhou Z, Jeschke MG, Branski LK, Herndon DN, Wang R, Szabó C (2009) Hydrogen sulfide is an endogenous stimulator of angiogenesis. Proc Natl Acad Sci 106(51):21972–21977
Umaru B, Pyriochou A, Kotsikoris V, Papapetropoulos A, Topouzis S (2015) ATP-sensitive potassium channel activation induces angiogenesis in vitro and in vivo. J Pharmacol Exp Ther 354(1):79–87
Hollenhorst MI, Richter K, Fronius M (2011) Ion transport by pulmonary epithelia. Biomed Res Int 2011
Pedersen SF, Hoffmann EK, Novak I (2013) Cell volume regulation in epithelial physiology and cancer. Front Physiol 4:233
Fraser SP, Grimes JA, Djamgoz MB (2000) Effects of voltage-gated ion channel modulators on rat prostatic cancer cell proliferation: comparison of strongly and weakly metastatic cell lines. Prostate 44(1):61–76
Lam CF, Liu YC, Tseng FL, Sung YH, Huang CC, Jiang MJ, Tsai YC (2007) High-dose morphine impairs vascular endothelial function by increased production of superoxide anions. J Am Soc Anesthesiol 106(3):532–537
Fahmy SR, Rabia I, Mansour EM (2014) The potential role of mefloquine against Schistosoma mansoni infection by prohibition of hepatic oxidative stress in mice. J Basic Appl Zool 67(2):40–47
Mergler S, Pleyer U (2007) The human corneal endothelium: new insights into electrophysiology and ion channels. Prog Retin Eye Res 26(4):359–378
Murek M, Kopic S, Geibel J (2010) Evidence for intestinal chloride secretion. Exp Physiol 95(4):471–478
Duan DD (2013) Phenomics of cardiac chloride channels. Compr Physiol
Davies N, Akhtar S, Turner HC, Candia OA, To CH, Guggenheim JA (2004) Chloride channel gene expression in the rabbit cornea. Mol Vis 10(122-23):1028–1037
Pardo LA (2004) Voltage-gated potassium channels in cell proliferation. Physiology 19(5):285–292
Ouadid-Ahidouch H, Ahidouch A (2013) K+ channels and cell cycle progression in tumor cells. Front Physiol 4:220
Kale VP, Amin SG, Pandey MK (2015) Targeting ion channels for cancer therapy by repurposing the approved drugs. Biochim Biophys Acta Biomembr 1848(10):2747–2755
Kim CD, Kim HH, Kim YK, Kwak YK, Kim SO, Yoo SE, Hong KW (2001) Antiangiogenic effect of KR31372 in rat sponge implant model. J Pharmacol Exp Ther 296(3):1085–1090
Jean-Yves LG, Halima OA, Olivier S, Pierre B, Ahmed A, Christophe V (2007) Voltage-gated ion channels, new targets in anti-cancer research. Recent Pat Anticancer Drug Discov 2(3):189–202
El-Kenawi AE, El-Remessy AB (2013) Angiogenesis inhibitors in cancer therapy: mechanistic perspective on classification and treatment rationales. Br J Pharmacol 170(4):712–729
Urrego D, Tomczak AP, Zahed F, Stühmer W, Pardo LA (2014) Potassium channels in cell cycle and cell proliferation. Philos Trans R Soc B 369(1638):20130094
Santoni G, Santoni M, Nabissi M (2012) Functional role of T-type calcium channels in tumour growth and progression: prospective in cancer therapy. Br J Pharmacol 166(4):1244–1246
Kamili C, Kakataparthy RS, Vattikutti UM, Chidrawar V, Ammineni S. Anti-proliferative and anti-angiogenic activities of ion-channel modulators: in-ovo, in-vitro and in-vivo study. Asian Pac J Trop Biomed. 2017;7(6):555–62.
Acknowledgments
We thank the management of CMR College of Pharmacy for allowing us to perform the research in the institution.
Funding
The research was supported by the university grants commission and minor research project grant (Proposal Number: 3228; ROMRP-SERO-PHAR-2015-16-68663). They provided partial financial support for the research.
Author information
Authors and Affiliations
Contributions
CK and HSK majorly contributed in the research work. SR, AK, and UMRV contributed in writing the manuscript. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval
CPCSEA guidelines were strictly followed and the studies were approved by the Institutional animal ethical committee (IAEC) (Ref: CPCSEA /1657/ IAEC /CMRCP/PhD-14/30), CMR College of Pharmacy, Hyderabad, India.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kamili, C., Kandoti, H.S., Radhakrishnan, S. et al. Anti-angiogenic activity of chloride and potassium channel modulators: repurposing ion channel modulators. Futur J Pharm Sci 6, 24 (2020). https://doi.org/10.1186/s43094-020-00041-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43094-020-00041-1