Abstract
Background
The increased prevalence of hepatocellular carcinoma (HCC) in diabetic patients has focused on the need to characterize the role of altered metabolites in liver carcinogenesis. In this study, together with the serum biochemistry and histopathological observation, 1H nuclear magnetic resonance (1H-NMR)-based metabolomics was carried out to study the effect of asarone and metformin in diabetic HCC rats. Intraperitoneal administration of streptozotocin (STZ; 55 mg/kg b.w.) was used to induce diabetes in male Wistar rats. Further, 2 weeks later, after confirmation of diabetes, another group received diethylnitrosamine (DEN; 200 mg/kg b.w.) to simulate the diabetic HCC condition. The combined dose of α-and β-asarone (50 µg/kg b.w. in the ratio of 1:1) and metformin HCl (250 mg/kg b.w.) treatment was orally given to the diabetic HCC rats for 18 weeks. The serum samples were subjected to 1H-NMR-based metabolomics analysis to explore the metabolite changes at the end of the study.
Results
1H-NMR study quantitatively distinguished the metabolites, such as pyruvate, lactate, creatine, acetate, glutamine, valine, and alanine, which varied between the diabetic HCC and normal rats. Furthermore, compared to the diabetic HCC group, the administration of asarone and metformin resulted in a substantial change in metabolite levels. Histopathological examination indicated that treatment attenuates the magnitude of the toxic effect of STZ + DEN.
Conclusions
The aberrant glucose, lipid, and amino acid metabolisms were associated with developing hepatocarcinogenesis in rats during the diabetic condition. Treatment with asarone and metformin attenuated the metabolic changes due to STZ + DEN-induced diabetic HCC.
Similar content being viewed by others
Background
Human hepatocellular carcinoma (HCC) is one of the most common forms of primary liver cancer. It accounts for the world's third-leading cause of cancer-related death (El-Serag 2012). It usually results as a complication of preceding liver disease due to infection with the hepatitis virus, alcoholic consumption, non-alcoholic steatohepatitis (NASH), exposure to aflatoxin-contaminated food, and liver cirrhosis (Liu and Kao 2013; Venook et al. 2010; Simonetti et al. 1991). Further, epidemiological evidence suggests diabetes mellitus (DM) as one of the potential risk factors in the progression of HCC (Vecchia et al. 1997; Davila et al. 2005; Yuan et al. 2004). The current diagnostic investigations include the different biochemical profiling approaches (tumor markers mainly α-fetoprotein) along with hepatic arteriography, magnetic resonance imaging (MRI), and computed tomography (CT) by focusing on the genetic and protein variations of various cancers (Colli et al. 2006).
Magnetic resonance spectroscopy (MRS) and magnetic resonance imaging (MRI) are relatively new techniques, emerging as a powerful, robust analytical tool, particularly in medicine (Glunde et al. 2011). Nuclear magnetic resonance (NMR) spectroscopy is a robust technique that detects many metabolites present in a single experiment. This technique does not require a standard reference for each metabolite. It can be used over existing analytical methods like colorimetry, gas chromatography coupled to mass spectrometry (GC-MS), and other separation techniques. Due to its high noninvasive nature, the sample does not require pre- or post-processing (Emwas et al. 2019).
There are reports on using the NMR spectroscopy method to quantitatively measure the metabolites involved in the pathological and diagnostic progression of the diseases (Nicholson et al. 1999; Gowda et al. 2008; Griffin and Vidal-Puig 2008). The metabolic profile obtained from serum, urine, or tissue samples associated with the progression of the disease could provide a better understanding of the underlying molecular mechanism. Reports suggest promising response in elucidating the key metabolic pathways in the breast (Woo et al. 2009), brain (Petrik et al. 2006), lung (Cameron et al. 2016), prostate (Sreekumar et al. 2009), liver (Wang et al. 2011), ovarian (Denkert et al. 2006), oral (Yan et al. 2008), and pancreatic cancers (Bi et al. 2014). Various studies have also demonstrated a practical metabolomic approach for identifying potential biomarkers in diabetic patients (Yang et al. 2004; Van Doorn et al. 2007).
The changes in the glucose metabolism pathway are known to involve the progression of HCC through disturbances in the metabolism of amino acids, lipids, and energy. However, the systemic and characteristic metabolomic changes concerned with the progression of HCC during diabetic conditions remain unexplored. Furthermore, the two main pharmacologically active phytochemicals in the Acorus calamus, alpha (α)- and beta (β)-asarone, and also the extract, have been shown to have cytotoxic and hypoglycemic activities (Das et al. 2019a, b; Liu et al. 2015). On the other hand, there are reports based on epidemiological, clinical, and experimental studies suggesting that metformin reduces the cancer risk with diabetes (Li et al. 2018; Das et al. 2019a). However, there is no evidence related to asarone and metformin in support of the changes in the metabolic profile during the diabetic HCC condition. Henceforth, in the current work, we attempt to understand the metabolic profile and evaluate the impact of asarone and metformin with the changes in the key metabolites in controlling the progression of hepatocarcinogenesis during the diabetic condition via 1H-NMR spectra. The functional significance of the analyzed metabolites for the most pertinent metabolic pathways was done based on the online Kyoto Encyclopedia of Genes and Genomes (KEGG) database and Human Metabolome Database (HMDB) (Dutta et al. 2012; Wishart et al. 2013).
Methods
Chemicals and reagents
Streptozotocin (STZ) extra pure was obtained from Sisco Research Laboratories (SRL) Pvt. Ltd., Mumbai, India. Diethylnitrosamine (DEN), deuterium oxide (D2O), alpha- and beta-asarone were procured from Sigma-Aldrich Chemical Company (USA). Metformin HCl was obtained as a gift sample from Angels Pharma India Pvt. Ltd., Hyderabad, India. All the other reagents and chemicals were analytically graded and obtained from standard commercial suppliers.
Animal experiment
Adult male Wistar rats, weighing 150–200 g, were used for the study. Under standard environmental conditions, the animals were housed in polypropylene cages, maintained at 27 ± 2 °C with a 12-h light and dark cycle. All animal experiments were performed in agreement with the guidelines after needed approval by the Institutional Animal Ethical Committee (Approval no. 07/KLEU'SCOPH/16).
Experimental induction of diabetes and hepatocellular carcinoma
Type 1 diabetes was induced by a single intraperitoneal injection of a freshly prepared solution of STZ (55 mg/kg b.w. in 0.05 M ice-cold citrate buffer solution of pH 4.5) in overnight fasted rats. However, the STZ caused fatal hypoglycemia due to massive pancreatic insulin release, so the rats were supplied with sucrose (prepared as 10% w/v water solution) for the next 24 h. In addition, the HCC was induced by a single intraperitoneal injection of the carcinogenic chemical diethylnitrosamine (DEN; 200 mg/kg b.w. prepared in 0.9% w/v NaCl solution) (Furman 2015; Das et al. 2019a).
Experimental protocol
The rats were randomly divided into five groups, with six in each group (n = 6), as given in Table 1. Following 18 weeks of study, the blood/serum was collected from the overnight fasted rats after anesthetization (under mild ether anesthesia) for carrying out the biochemical and NMR analysis. Later, the liver tissues were collected from the euthanized rats for carrying out the histopathological findings, and finally, the carcasses were disposed of by incineration.
Estimation of glucose and lipid profile levels
The study of serum fasting glucose and lipid profile levels such as triglycerides (TG), total cholesterol (TC), and high-density lipoprotein cholesterol (HDL-c) were determined according to the procedure given by the commercial kits (Erba Transasia Bio-Medicals Ltd., India) using Erba Chem 7 semi-automated analyzer (Friedewald et al. 1972).
Preparation of serum samples and acquisition of 1H-NMR spectra
The 1H-NMR spectra for all serum samples were obtained on the JEOL advanced ECZ 400S spectrometer operating at 400 MHz proton frequency using a 5-mm TH5 direct broadband probe. Briefly, 300 µL of serum and 200 µL of deuterium oxide (D2O) was taken in a cleaned dried 5-mm NMR tube. A reusable sealed capillary tube containing 30 µL of 0.375% of the sodium salt of trimethylsilyl 2,2,3,3-tetradeuteropropionic acid (TSP) in D2O was inserted into the NMR tube before recording the spectra. The TSP served as a chemical shift reference and an external standard for quantitative estimation, whereas D2O served as the field-frequency lock. Further, a one-dimensional Carr-Purcell Meiboom-Gill (CPMG) pulse sequence acquired 1H-NMR spectra. The CPMG eliminates broad signals from protein, lipids, and macromolecules, and significantly altered metabolites were identified and discussed. All the spectra were recorded with 16-time domain data points, 15 ppm spectral width, 256 number of scans, 4 dummy scans, relaxation delay of 5 s, constant receiver gain value of 60, and tau interval of 0.172 ms. The NMR software version delta 5.0.5.1. was used for phase and baseline correction and for getting integral (area under the curve) value.
Quantification of the metabolites
The concentration of the metabolites was determined using integral values of the unambiguous signals for a known concentration of TSP, which was taken in a capillary tube and been calculated using the following formula:
where Ax and Nx are the integral area and number of protons of the metabolites; Mr and Mx are the molecular weight of TSP and metabolite; Wr is the weight of TSP taken in the capillary tube; Ar represents an integral area of TSP; and Nr represents the number of protons of TSP which serves as an external reference calibrated at 0.0 ppm for assignment of metabolites.
Histopathological findings of the liver (H and E staining)
The formalin-fixed liver tissues were dehydrated with 60 to 100% isopropyl alcohol solution and fixed in paraffin wax. Liver section slides stained with hematoxylin–eosin (H&E) were captured with a light microscope (Olympus Microsystem, Model-CKX41, Japan).
Statistical analysis
The obtained data from the various experimental groups were expressed as mean ± SEM using the statistical software package 'GraphPad Prism version 6.0.' The results were analyzed using a one-way ANOVA test. Further, Bonferroni multiple comparison tests were followed, considering p values of ˂ 0.05 as significant.
Results
Serum biochemical parameters
The effect of asarone and metformin on serum glucose and lipid profile levels is illustrated in Table 2. The STZ- and STZ + DEN-induced rats showed significant elevation (p < 0.001) of serum glucose and lipid profile levels (TG, TC, and LDL-c) along with a decrease (p < 0.001) in HDL-c compared to the normal control group. Further, the treated groups significantly controlled the glucose and lipid profile levels compared to the STZ + DEN group. However, the variation of LDL-c and HDL-c levels in the asarone-treated group was not statistically significant.
1H-NMR spectral analysis of serum samples
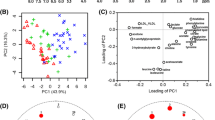
Figure 1 illustrates the typical representative 1H-NMR spectra of serum samples obtained from different experimental groups. The 1H-NMR spectral region from 0.0 to 5.3 ppm shows strong resonances from the serum samples and permits the measurements of the number of metabolites that are not overlapped by any other metabolites. They are pyruvate, lactate, creatine, acetate, valine, alanine, and glutamine, as given in Table 3.
Changes in metabolite concentrations
Figure 2 shows the dynamic changes of the metabolites (denoted in the green boxes) and their relevant pathways at the end of 18 weeks obtained from the KEGG and HMDB databases. To extract more details and the changes associated with the metabolic pathways with the progression of the disease, serum NMR spectra of metabolites were quantified (Table 3). The STZ-treated rats alone have significant metabolic modifications compared with the normal rats, including (1) decreased levels of pyruvate, alanine, and glutamine, although reduced levels of lactate, creatine, and valine were observed, but not statistically significant and; (2) increased levels of acetate. Further, the diabetic HCC (STZ + DEN) group reveals several metabolic alterations compared with the normal rats, (1) increased levels of pyruvate, lactate, creatine, and acetate; and (2) decreased levels of alanine and glutamine, with no significant alteration in the levels of valine. Following treatment with asarone and metformin in the diabetic HCC group, a substantial alteration was observed in the levels of metabolites compared with the STZ + DEN rats, (1) decreased levels of pyruvate, lactate, creatine, and acetate; (2) increased levels of alanine and glutamine, except no changes for creatine in metformin-treated, alanine in asarone-treated and valine for both the treatment groups.
The schematic metabolic pathways of hepatocarcinogenesis during diabetic conditions obtained from the KEGG and HMDB databases. The dynamic changes of the metabolites (denoted in the green boxes) detected by 1H-NMR serum analysis display the link with the metabolic pathways (represented in the red dotted boxes). KEGG, Kyoto Encyclopedia of Genes and Genomes (https://www.genome.jp/kegg/pathway.html); HMDB, Human Metabolome Database (https://hmdb.ca/metabolites)
Histopathological features
The typical histopathological features of rat livers for all the groups by hematoxylin–eosin (H and E) staining are represented in Fig. 3. The STZ-treated liver at the end of 18 weeks showed the features of congestion in the central vein (CV), portal triad (PT), and sinusoids (S) with severe inflammation in between the hepatocytes compared to normal livers where the hepatic lobules remain intact. In contrast, the structural disorganization in the livers of STZ + DEN rats could be observed with the development of all the characteristic features of HCC. Following treatment with asarone and metformin, the extent of the toxic effect was reduced compared to STZ + DEN rats.
Representative histological features of liver sections stained with hematoxylin–eosin (H and E) obtained from normal rats a, STZ-induced diabetic rats b, STZ + DEN-induced diabetic HCC rats c, STZ + DEN + Asarone d, and STZ + DEN + Metformin e, respectively. Black arrowheads indicate congestion in CV and PS. (a, b, d, e, magnification: 200; c, magnification: 100). STZ, streptozotocin; DEN, diethylnitrosamine; CV, central vein; PS, portal system
Discussion
Evidence in both experimental and clinical-based studies suggested a link between diabetes and cancer (Das and Gadad 2021; Das et al. 2021; Sciacca et al. 2013; Szablewski 2014). There is a higher risk of the prevalence of pancreatic, liver, colorectal, kidney, and endometrial cancers in persons with diabetes (Rahman et al. 2021). Hepatocellular carcinoma (HCC) is a multistep process involving genetic, DNA changes and alterations in metabolites throughout the disease’s initiation, promotion, and development (Hlady and Robertson 2018). Although numerous studies have elucidated the systemic abnormalities in several metabolites involving the difference between HCC and normal tissues (Wang et al. 2011; Tan et al. 2012), little is known about the characteristic metabolomic changes concerned with the progression of HCC during diabetic conditions. Henceforth, in this study, the 1H-NMR-based metabolomics was used to characterize the metabolic changes in experimentally induced diabetic HCC conditions. Furthermore, we evaluated the effect of asarone and metformin with the changes in the key metabolites in controlling the progression of the disease.
It is a well-known fact that the liver plays an essential role in maintaining the homeostasis of glucose, lipid, and energy metabolism. Dysregulation of this system is a significant aspect of the development of diabetes. The STZ selectively targets and destroys the insulin-secreting beta-cells of the pancreas leading to degressive glucose uptake and utilization and resulting in hyperglycemia (Hatting et al. 2018; Szkudelski 2001). The metabolites related to glucose metabolism pathways, such as pyruvate and lactate, are involved in the development of diabetes. In the NMR spectra of diabetic rats, we found lower levels of pyruvate and lactate, which is consistent with earlier findings (Zhao et al. 2010; Amaral et al. 2006). This decline in pyruvate and lactate levels suggests that the glycolysis pathway is impaired and may cause less production of ATP, which is involved in the synthesis of energy needed for the body. Further, the progression of hepato-carcinoma has also been linked with the alteration in plasma lipid and lipoprotein metabolism. As a source of energy and support for cell division and fatty acid derivatives, the tumor cells are highly dependent on the metabolism of the lipids, thereby directly linking to cell survival and growth (Beloribi et al. 2016). In this study, the STZ- and STZ + DEN-treated rats showed significantly altered lipid profile levels as TC, TG, LDL-c, and HDL-c. During diabetes, STZ-induced animals rely on other fuels for energy, such as lipids or free fatty acids, due to impaired glucose metabolism. This suggests the breakdown of lipids and further mobilization of free fatty acid from the peripheral fat repository. Henceforth, this results in triglycerides, cholesterol, and other lipids, as indicated in the study. Our results agree with a previous study that suggests that the rise in the acetate level is due to an increase in the beta-oxidation pathway of fatty acids during the diabetic condition (Chengfeng et al. 2014). Moreover, consistent with previous studies, the levels of amino acids were also reduced, indicating enhancement of gluconeogenesis during the diabetic state (Wijekoon et al. 2004; Atherton et al. 2006). These amino acid concentration alterations are comparable to those reported in type 1 diabetes. This implies that the changed glutamine and alanine levels in diabetic rats indicate the maintenance of fasting hyperglycemia (Chengfeng et al. 2014).
The aberrant glucose, lipid, and amino acid metabolites throughout the progression of hepatocarcinogenesis induced by DEN during STZ-induced diabetic conditions confirmed that energy supply is vital for tumor cells (Boroughs and Deberardinis 2015). As observed, the energy supply provided via the glycolysis pathway yields a more considerable amount of pyruvate and lactate during the diabetic HCC condition. This indicates an increase in energy demand through glycolysis during the process of hepatocarcinogenesis and is considered one of the hallmarks of cancer (Pavlova and Thompson 2016). Creatine is another metabolite participating in the energy metabolism for the maintenance of fluctuating energy demands. In our study, elevated creatine levels were observed compared to normal rats, suggesting the difference related to the energy demand in diabetic HCC conditions (Barcelos et al. 2016). Further, a significant increase in the acetate content of diabetic HCC reflects the metabolism of hepatic lipids, which agrees with the serum lipid profile showing increased levels of different lipids. This directs the supplement of energy source for the proliferation of tumor cells besides glucose metabolism and could be used as a potential biomarker for diabetic HCC. Glutamine, the non-essential amino acid in cancer, is highly heterogeneous, and it depends on a variety of factors that collectively impact its role in cancer cell metabolism (Cluntun et al. 2017). The abnormal alterations in glutamine levels during diabetic HCC conditions influence its role in metabolism by the fast-proliferating hepatocytes for meeting the need for energy supply.
Furthermore, the alterations seen in the STZ + DEN-induced group compared to normal rats were validated by serum biochemical results consisting of several liver function enzymes and biomarkers as confirmed in our previous studies. This model has also been used to explore the histo-morphological signatures starting from inflammation to HCC in STZ + DEN-treated rats to replicate the clinical evidence for the diabetic HCC condition. Here, we have confirmed the induction of diabetes and HCC in rats with the help of biochemical markers such as glycosylated hemoglobin (HbA1c), insulin, gamma-glutamyl transferase (GGT), and α-fetoprotein (AFP) (Das et al. 2019a; Das and Gadad 2020).
Epidemiological, clinical, and experimental studies suggest that metformin reduces the cancer risk with diabetes (Li et al. 2018). Our study also observed that metformin either decreased or altered the severity of hepatocarcinogenesis in diabetic conditions as confirmed by 1H-NMR-based metabolomics and histopathological evidence. The results are based on the lipid profile Furthermore, the test compound asarone also attenuated the characteristic metabolic changes in the pathological process of diabetic HCC conditions.
Conclusions
In conclusion, 1H-NMR-based metabolomics approach was used to elucidate the small molecular metabolites in the serum samples for studying the pathological progress of diabetic HCC. We primarily outlined the peculiarity in glucose, lipid, and amino acid metabolisms over the development of hepatocarcinogenesis in rats during the diabetic condition, which provided us with a better understanding of the metabolite changes. Furthermore, asarone and metformin successfully improved the metabolic changes caused by STZ and DEN in diabetic HCC rats, indicating altered energy metabolism with metabolite changes. However, a further detailed investigation is needed to know about the possibility of involvement of pivotal metabolic pathways shared between both the diseases. Also, there is a need to identify and quantify the larger metabolites linked to diabetic HCC conditions.
Availability of data and materials
Data sharing does not apply to this article as no datasets were generated or analyzed during the current study.
Abbreviations
- 1H-NMR:
-
1H nuclear magnetic resonance
- DEN:
-
Diethylnitrosamine
- HMDB:
-
Human Metabolome Database
- HCC:
-
Hepatocellular carcinoma
- KEGG:
-
Kyoto encyclopedia of genes and genomes
- STZ:
-
Streptozotocin
References
Amaral S, Moreno AJ, Santos MS, Seica R, Ramalho-Santos J (2006) Effects of hyperglycemia on sperm and testicular cells of Goto-Kakizaki and streptozotocin-treated rat models for diabetes. Theriogenology 66:2056–2067
Atherton HJ, Bailey NJ, Zhang W, Taylor J, Major H, Shockcor J (2006) A combined 1H-NMR spectroscopy- and mass spectrometry-based metabolomic study of the PPAR-alpha null mutant mouse defines profound systemic changes in metabolism linked to the metabolic syndrome. Physiol Genomics 27:178–186
Barcelos RP, Stefanello ST, Mauriz JL, Gonzalez-Gallego J, Soares FAA (2016) Creatine and the liver: metabolism and possible interactions. Mini Rev Med Chem 16:12–18
Beloribi DS, Vasseur S, Guillaumond F (2016) Lipid metabolic reprogramming in cancer cells. Oncogene 5:e189
Bi HC, Pan YZ, Qiu JX, Krausz KW, Li F, Johnson CH et al (2014) N-methylnicotinamide and nicotinamide N-methyltransferase are associated with microRNA-1291-altered pancreatic carcinoma cell metabolome and suppressed tumorigenesis. Carcinogenesis 35:2264–2272
Boroughs LK, Deberardinis R (2015) Metabolic pathways promoting cancer cell survival and growth. Nat Cell Biol 17:351–359
Cameron SJS, Lewis KE, Beckmann M, Allison GG, Ghosal R, Lewis PD et al (2016) The metabolomic detection of lung cancer biomarkers in sputum. Lung Cancer 94:88–95
Chellian R, Pandy V, Mohamed Z (2017) Pharmacology and toxicology of α- and β-asarone: a review of preclinical evidence. Phytomedicine 32:41–58
Chengfeng D, Liangcai Z, Mimi G, Yongquan Z, Minjiang C, Yunjun Y (2014) Systemic and characteristic metabolites in the serum of streptozotocin-induced diabetic rats at different stages as revealed by a 1H-NMR based metabonomic approach. Mol Biosyst 10:686–693
Cluntun AA, Lukey MJ, Cerione RA, Locasale JW (2017) Glutamine metabolism in cancer: understanding the heterogeneity. Trends Cancer 3:169–180
Colli A, Fraquelli M, Casazza G, Massironi S, Colucci A, Conte D et al (2006) Accuracy of ultrasonography, spiral CT, magnetic resonance and alpha-fetoprotein in diagnosing hepatocellular carcinoma: a systematic review. Am J Gastroenterol 101:513–523
Das BK, Gadad PC (2020) Asarone and metformin modulates the oxidant-antioxidant imbalance on experimentally induced hepatocellular carcinoma during diabetic condition. Int J Pharm Edu Res 54:1039–1045
Das BK, Gadad PC (2021) Impact of diabetes on the increased risk of hepatic cancer: an updated review of biological aspects. Diabetes Epidemiol Manag 4:100025
Das BK, Swamy AHMV, Koti BC, Gadad PC (2019a) Experimental evidence for use of Acorus calamus (asarone) for cancer chemoprevention. Heliyon 5:e01585
Das BK, Choukimath SM, Gadad PC (2019b) Asarone and metformin delays experimentally induced hepatocellular carcinoma in diabetic milieu. Life Sci 230:10–18
Das BK, Knot R, Gadad PC (2021) Metformin and asarone inhibit HepG2 cell proliferation in a high glucose environment by regulating AMPK and Akt signaling pathway. Futur J Pharm Sci 7:43
Davila JA, Morgan RO, Shaib Y, McGlynn KA, El-Serag HB (2005) Diabetes increases the risk of hepatocellular carcinoma in the United States: a population-based case-control study. Gut 54:533–539
Denkert C, Budczies J, Kind T, Weichert W, Tablack P, Sehouli J et al (2006) Mass spectrometry-based metabolic profiling reveals different metabolite patterns in invasive ovarian carcinomas and ovarian borderline tumors. Cancer Res 66:10795–10804
DePeralta DK, Wei L, Ghoshal S, Schmidt B, Lauwers GY, Lanuti M et al (2016) Metformin prevents hepatocellular carcinoma development by suppressing hepatic progenitor cell activation in a rat model of cirrhosis. Cancer 122:1216–1227
Dutta M, Joshi M, Srivastava S, Lodh I, Chakravarty B, Chaudhury K (2012) A metabonomics approach as a means for identification of potential biomarkers for early diagnosis of endometriosis. Mol Biosyst 8:3281–3287
El-Serag HB (2012) Epidemiology of viral hepatitis and hepatocellular carcinoma. Gastroenterol 142:1264–1273
Emwas AH, Roy R, McKay RT, Tenori L, Saccenti E, Gowda GAN et al (2019) NMR spectroscopy for metabolomics research. Metabolites 9:123
Friedewald WT, Levy RI, Fredrickson DS (1972) Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 18:499–502
Furman BL (2015) Streptozotocin-induced diabetic models in mice and rats. Curr Protoc Pharmacol 70:5.47.1–5.47.20
Glunde K, Jiang L, Moestue SA, Gribbestad IS (2011) MRS and MRSI guidance in molecular medicine: targeting and monitoring of choline and glucose metabolism in cancer. NMR Biomed 24:673–690
Gowda GA, Zhang S, Gu H, Asiago V, Shanaiah N, Raftery D (2008) Metabolomics-based methods for early disease diagnostics. Expert Rev Mol Diagn 8:617–633
Griffin JL, Vidal-Puig A (2008) Current challenges in metabolomics for diabetes research: a vital functional genomic tool or just a ploy for gaining funding? Physiol Genomics 34:1–5
Hatting M, Tavares CDJ, Sharabi K, Rines AK, Puigserver P (2018) Insulin regulation of gluconeogenesis. Ann N Y Acad Sci 1411:21–35
Hlady RA, Robertson KD (2018) Genetic and epigenetic heterogeneity in normal liver homeostasis and its implications for liver disease and hepatocellular cancer. Semin Liver Dis 38:41–50
Li M, Li X, Zhang H, Lu Y (2018) Molecular mechanisms of metformin for diabetes and cancer treatment. Front Physiol 9:1039
Liu CJ, Kao JH (2013) Global perspective on the natural history of chronic hepatitis B: role of hepatitis B virus genotypes A to J. Semin Liver Dis 33:97–102
Liu YX, Si MM, Lu W, Zhang LX, Zhou CX, Deng SL et al (2015) Effects and molecular mechanisms of the antidiabetic fraction of Acorus calamus L. on GLP-1 expression and secretion in vivo and in vitro. J Ethnopharmacol 166:168–175
Nicholson JK, Lindon JC, Holmes E (1999) Metabonomics: Understanding the metabolic responses of living systems to pathophysiological stimuli via multivariate statistical analysis of biological NMR spectroscopic data. Xenobiotica 29:1181–1189
Pavlova NN, Thompson CB (2016) The emerging hallmarks of cancer metabolism. Cell Metab 23:27–47
Petrik V, Loosemore A, Howe FA, Bell BA, Papadopoulos MC (2006) OMICS and brain tumour biomarkers. Br J Neurosurg 20:275–280
Rahman I, Athar MT, Islam M (2021) Type 2 diabetes, obesity, and cancer share some common and critical pathways. Front Oncol 10:600824
Sciacca L, Vigneri R, Tumminia A, Frasca F, Squatrito S, Frittitta L et al (2013) Clinical and molecular mechanisms favoring cancer initiation and progression in diabetic patients. Nutr Metab Cardiovasc Dis 23:808–815
Simonetti RG, Camma C, Fiorello F, Politi F, D’Amico G, Pagliaro L (1991) Hepatocellular carcinoma. A worldwide problem and the major risk factors. Dig Dis Sci 36:962–972
Sreekumar A, Poisson LM, Rajendiran TM, Khan AP, Cao Q, Yu J et al (2009) Metabolomic profiles delineate potential role for sarcosine in prostate cancer progression. Nature 457:910–914
Szablewski L (2014) Diabetes mellitus: influences on cancer risk. Diabetes Metab Res Rev 30:543–553
Szkudelski T (2001) The mechanism of alloxan and streptozotocin action in B cells of the rat pancreas. Physiol Res 50:537–546
Tan Y, Yin P, Tang L, Wenbin X, Qiang H, Dan C et al (2012) Metabolomics study of stepwise hepatocarcinogenesis from the model rats to patients: potential biomarkers effective for small hepatocellular carcinoma diagnosis. Mol Cell Proteomics 11(M111):010694
Van Doorn M, Vogels J, Tas A, van Hoogdalem EJ, Burggraaf J, Cohen A et al (2007) Evaluation of metabolite profiles as biomarkers for the pharmacological effects of thiazolidinediones in Type 2 diabetes mellitus patients and healthy volunteers. Br J Clin Pharmacol 63:562–567
Vecchia CA, Negri E, Decarli A, Franceschi S (1997) Diabetes mellitus and the risk of primary liver cancer. Int J Cancer 73:204–207
Venook AP, Papandreou C, Furuse J, de Guevara LL (2010) The incidence and epidemiology of hepatocellular carcinoma: a global and regional perspective. Oncologist 15:5–13
Wang J, Zhang S, Li Z, Yang J, Huang C, Liang R et al (2011) 1H-NMR-based metabolomics of tumor tissue for the metabolic characterization of rat hepatocellular carcinoma formation and metastasis. Tumor Biol 32:223–231
Wijekoon EP, Skinner C, Brosnan ME, Brosnan JT (2004) Amino acid metabolism in the zucker diabetic fatty rat: Effects of insulin resistance and type 2 diabetes. Can J Physiol Pharmacol 82:506–514
Wishart DS, Jewison T, Guo AC, Wilson M, Knox C, Liu Y et al (2013) HMDB 3.0—the human metabolome database in 2013. Nucleic Acids Res 41:D801–D807
Woo HM, Kim KM, Choi MH, Jung BH, Lee J, Kong G et al (2009) Mass spectrometry based metabolomic approaches in urinary biomarker study of women’s cancers. Clin Chim Acta 400:63–69
Yan SK, Wei BJ, Lin ZY, Yang Y, Zhou ZT, Zhang WD (2008) A metabonomic approach to the diagnosis of oral squamous cell carcinoma, oral lichen planus and oral leukoplakia. Oral Oncol 44:477–483
Yang J, Xu G, Hong Q, Liebich HM, Lutz K, Schmulling RM et al (2004) Discrimination of type 2 diabetic patients from healthy controls by using metabonomics method based on their serum fatty acid profiles. J Chromatogr B Anal Technol Biomed Life Sci 813:53–58
Yuan JM, Govindarajan S, Arakawa K, Yu MC (2004) Synergism of alcohol, diabetes and viral hepatitis on the risk of hepatocellular carcinoma in blacks and whites in the U.S. Cancer 101:1009–1017
Zhao LC, Zhang XD, Liao SX, Gao HC, Wang HY, Lin DH (2010) A metabonomic comparison of urinary changes in Zucker and GK rats. J Biomed Biotechnol 2010:431894
Acknowledgements
We thank the Principal, KLE College of Pharmacy, Hubballi, for providing the facilities to carry out the research work. We also thank the Sophisticated Analytical Instrument Facilities (SAIF) of Karnatak University, Dharwad, for providing the instrumentation facilities.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
BKD and PCG designed and conceived the research; BKD performed the animal studies; BKD and JK performed the NMR experiments; BKD and JK processed the analyzed data; BKD and JK wrote the manuscript. PCG was associated with supervising, advising, reviewing, and editing the final version of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was reviewed and approved by the Institutional Animal Ethics Committee, KLE College of Pharmacy, Hubballi, and Approval no. 07/KLEU'SCOPH/16. The animal experiments were carried out in accordance with the CPCSEA guidelines.
Consent for publication
Not applicable.
Competing interests
The authors do not have any competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Das, B.K., K, J. & Gadad, P.C. 1H-NMR-based serum metabolomic study to evaluate the effect of asarone and metformin on experimentally induced diabetic hepatocellular carcinoma in rats. Bull Natl Res Cent 46, 164 (2022). https://doi.org/10.1186/s42269-022-00849-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42269-022-00849-2