Abstract
Background
Non-functioning pituitary adenomas have been treated by gross total resection with the microscopic transsphenoidal approach being the standard for decades. Recently, the endoscope has been utilized as alternative with its possible advantages and disadvantages.
Methods
In this study, the authors retrospectively reviewed 58 cases who underwent transsphenoidal non-functioning pituitary adenomas resection, 25 via the microscopic approach (group 1) and 33 via the endoscopic approach (group 2). Different aspects of the procedures were compared, including duration of surgery, incidence of post-operative cerebrospinal fluid leak (being one of the common complications after such procedures), length of hospital stay postoperatively, and most importantly the tumor volume reduction being measured in a novel method by creating a computer-generated three-dimensional reconstruction of the tumor.
Results
The length of hospital stay for group 1 ranged from 2 to 9 days (mean 3.6 days, SD 2.141) while in group 2, it ranged from 2 to 7 days (mean 3.727 days, SD 1.008). Operative time mean was 92.7 min in group 1 and 142.79 min in group 2. Intraoperative CSF leak was encountered in 40% (n = 10) of the cases in group 1 and in five cases (15.2%) from group 2. Volume reduction percentage had a mean of 82.4% in group 1 and 89.1% in group 2. Although the mean of volume reduction percentage was higher in group 2, yet this difference was found to be statistically insignificant with a p value of 0.141.
Conclusion
Endoscopic approach showed superiority by having lower incidence of post-operative cerebrospinal fluid leak, length of hospital stay, and tumor volume reduction while the microscopic approach was only favored in having shorter mean duration of surgery.
Similar content being viewed by others
Background
Surgical gross total resection surgery is the most common treatment for non-functioning pituitary adenomas (NFPA) and has usually been achieved well via the transsphenoidal approach [1]. This has been done using a standard operating microscope and peering into the transsphenoidal space for decades, or more recently using the endoscope. Microscopic transsphenoidal surgery predates endoscopic surgery and was historically the more common technique. This has been attributed to the fact that the neurosurgeons are more familiar with the microscope as it is used in many other neurosurgical approaches compared to the endoscope which requires a new skill acquisition for most neurosurgeons, yet it provides wider and more flexible viewing angles which can be critical during the resection of some sellar and parasellar tumors [2].
For gross total resection to be achieved, thorough assessment of tumor extensions should be accomplished. The Knosp classification system assigns a grade from 0 to 4 based on the lateral extent of the tumor in relation to the intracavernous segment of the internal carotid artery on coronal magnetic resonance image (MRI) sections [3]. Tumors with grades 0–2 are contained within the lateral carotid artery tangential, while tumors that extend beyond the carotid artery tangential are grades 3–4. However, the Knosp classification is not without its limitations as several studies have shown that MRI is not sensitive enough to detect microscopic invasion of the surrounding dura and cavernous sinus wall, especially with small tumors [4].
There is no general agreement on the superiority of either surgical approach over the other in terms of the extent of achievable resection for variously sized and located tumors or in terms of possible complications [4, 5].
Starke et al. recently compared microscopic and endoscopic approaches in growth hormone-secreting tumors [4]. The results of their study suggest that there is no difference between both approaches in achieving biochemical remission or in complication rates. Previous comparisons suggest that patients who undergo the endoscopic approach have shorter operative times, less operative blood loss, shorter hospitalizations, and fewer postoperative complications [6]. However, most of these studies have compared a prior microscopic series to a more recent endoscopic series or have included only small numbers of patients. No study has addressed whether one approach is superior for moderate-sized tumors without radiographic evidence of lateral extension into the cavernous sinus or has compared the outcomes of the two surgical approaches over the same interval [5].
Aim of the study
This study was designed to compare microscopic and endoscopic approaches in treatment of non-functioning pituitary adenomas regarding the degree of achievable safe resection and the rates of possible complications.
Methods
This is a retrospective analysis of prospectively collected data from a series of patients that underwent microscopic and endoscopic endonasal resection of non-functioning pituitary adenomas between January 2012 and July 2017. Patients were retrospectively divided into two groups: group 1 including patients who underwent microscopic resection and group 2 for patients who underwent endoscopic resection. The study included patients who had non-functioning histopathologically confirmed pituitary adenomas with a size of more than 1 cm. Moreover, availability of digital copies of preoperative and 2–6 months postoperative MRI with gadolinium intravenous contrast was mandatory for patients’ inclusion. Patients with hormone-secreting tumors were excluded from the study as well as those with recurrent tumors and pituitary apoplexy and those undergoing redo surgery for inadequately removed tumors.
Data were collected from patients’ charts retrospectively and included patient demographics, clinical picture, laboratory workup, intraoperative findings, surgical complications, and postoperative findings. Pre-operative MRI done shortly before the surgery and 3 months post-operative MRI were reviewed and used for analysis by an independent radiologist. Tumor volumetric measurements, by creating a three-dimensional reconstruction of the tumor, depending on the T1 and T1 with gadolinium contrast coronal sequence using OsiriX Lite free software version 9.0.2 was performed by calculating the area on each 1.5 mm coronal cut and then tumor volume was calculated (Figs. 1 and 2).
Surgeries were done by two different surgeons, each with a preference for an approach. Both surgeons aimed for maximum tumor resection when possible. An otolaryngologist assisted in the sellar exposure for all the endoscopic cases, and a binostril, three-hand technique was used in all of those cases. Nasoseptal mucosal flap was harvested early during the surgery in most of the patients undergoing the endoscopic resection and used for sellar floor reconstruction as precautionary measure against post-operative cerebrospinal fluid (CSF) leakage especially towards the end of the cohort.
Statistical analysis
Collected data were expressed as mean ± standard deviation and range and compared via paired and independent student t test and the ANOVA test using SOFA statistics free software version 1.3.3.
Results
This study included 58 patients, with 25 patients in group 1 (who underwent microscopic resection of the adenoma) including 12 males and 13 females and 33 patients in group 2 (who underwent endoscopic resection) including 14 males and 19 females. Mean age was 54.6 years (ranging from 20 to 72) and 62.9 years (ranging from 30 to 89) for group 1 and 2 respectively.
The length of hospital stay for group 1 ranged from 2 to 9 days (mean 3.6 days, SD 2.141) while in group 2, it ranged from 2 to 7 days (mean 3.727 days, SD 1.008). The mean time of follow-up in group 1 was 84.75 days (ranging from 72 to 99 days), and in group 2, it was 92.78 days (ranging from 70 to 141 days).
Regarding operative time, it ranged from 40 to 156 min (mean 92.7 min) in group 1 and from 82 to 234 min (mean 142.79 min) in group 2. This difference in operative time was found to be statistically significant with a p value < 0.001.
Intraoperative CSF leak was encountered in 40% (n = 10) of the cases in group 1 with only 2 cases (8%) requiring reoperation for repair of CSF leak. On the other hand, five cases (15.2%) from group 2 had intraoperative CSF leak and none of those required reoperation.
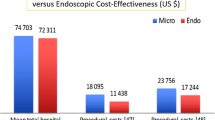
The mean preoperative tumor volume was 4.188 cm3 (ranging from 0.4 to 18.8 cm3, SD = 4.087) in group 1 and 7.164 cm3 (ranging from 0.5 to 48.7 cm3, SD = 8.797) in group 2. Postoperatively, the mean tumor volume was 1.012 cm3 (ranging from 0 to 8.2 cm3, SD = 2.101) in group 1 and 0.515 cm3 (ranging from 0 to 3.8 cm3, SD = 0.82) for group 2. Knosp grade ranged from 0 to 4 in both groups with a mean Knosp grade of 1.68 (SD 1.38) and 2.06 (SD 1.32) in groups 1 and 2 respectively.
Volume reduction percentage had a mean of 82.4% in group 1 and 89.1% in group 2. Although the mean of volume reduction percentage was higher in group 2, yet this difference was found to be statistically insignificant with a p value of 0.141. The volume of resected tumor ranged from 0.3 to 12.2 cm3 (mean 3.18 cm3) in the microscopic group compared to 0.4 to 48.5 cm3 (mean 6.67 cm3) in the endoscopic group.
It was also noted that there was no direct relation between the volume reduction percentage and the Knosp classification of the tumor neither in group 1 nor in group 2 in this study (Table 1).
Discussion
With the introduction of any new surgical technique, there is always a challenge to be met. In this study, the authors analyze the use of endoscopic resection of NFPA as a relatively new alternative to microscopic resection. The main targets to achieve in the new technique would be equal tumor resection, less incidence of complications, especially CSF leak, shorter duration of surgery, and shorter hospital stay. The proposed advantages of the new technique are better visualization and less violation of the nasal cavity and mucosa.
In the current study, the authors studied 58 cases of NFPA retrospectively, divided into endoscopic and microscopic groups. Comparing the surgical time between the two groups, it was found that the microscopic surgery took significantly shorter duration, on average, when compared with the average of endoscopic surgery (92.7 min and 142.8 min respectively). This result contradicts what was previously published by Cho and Liau in 2002 [7] who stated that the operative time ranged 1.5–4.0 h in the microscopic patients’ group and 1.0–3.0 h in the endoscopic patients’ group. Moreover, Higgins et al. in 2008 [8] had a mean operative time for microscopic and endoscopic approaches of 152 min and 117 min respectively. Yet, other studies found no significant difference between the two techniques regarding this parameter including Casler et al. [9] and Jain et al. [10].
Regarding the length of stay in the hospital, the current study found out that there was no statistically significant difference between the two groups although the cases from group 1 (microscopic resection) had longer range for duration of stay, 9 days, compared to 7 days for the endoscopic resection group. This matches the significantly shorter hospital stay for endoscopic resection of NFPA in multiple studies including Higgins et al. [8], Casler et al. [9], and Cappabianca et al. [11].
In the current series, the microscopic group showed significantly higher incidence of intraoperative CSF leak, with two patients requiring reoperation for control of CSF leak. None of the endoscopic patients required reoperation, and only one patient required placement of lumbar drain, while in the microscopic group, two patients required reoperation and six required lumbar drain placement. In our opinion, this finding can be attributed to better visualization of the sellar contents during surgery and the lower incidence of need for lumbar drain and absence of any cases requiring reoperation in the endoscopic group can be attributed the routing nasoseptal flap done in all endoscopic cases routinely. These findings are conformal to the findings reported by Higgins et al. [8] and White et al. [12]; they both found a significantly lower incidence of the need for lumbar drain placement postoperatively in the endoscopic group. Neal et al. [13] also found less need for lumbar drain after surgery in endoscopic cases, despite that they did not comment on the significance of this finding. Duz et al. [14] also found a significant difference in the incidence of CSF leak in favor of the endoscopic approach (33% vs 11%) which is comparable to the current results. However, Higgins et al. [8], Casler et al. [9], Choe et al. [15], Jain et al. [10], and White et al. [12] found no significant difference in CSF leak between the two groups.
Tumor volume preoperatively was found to be 7.2 cm3 in the endoscopic group compared to 4.2 cm3 in the microscopic group; this cannot be attributed to selection bias since the surgical team was different for each group. Volume reduction in the microscopic group had a mean of 82.4% which was not significantly different from the endoscopic group volume reduction that had a mean of 89.1%. However, it is to be noticed that in Knosp grade 3 and 4 tumors, the volume reduction was significantly higher in the endoscopic group compared to microscopic group (89% versus 77.4% for grade 3 and 98% versus 82.4% for grade 4). Although both techniques allow excellent visualization of the midline structures, the lateral and suprasellar compartments visualization can be limited with the microscope; in contrast, the endoscopic approach allowed excellent views of the lateral blind spots and the suprasellar areas. Karppinen et al. had similar findings in their study in 2015 [1]; they found that the endoscopic cases achieved a higher volume reduction rate in comparison to the microscopic cases (86% versus 82%), and they also noted a higher incidence of gross total resection in the endoscopic group (56% versus 45%). Despite the fact that both differences were statistically insignificant, yet those volumes indicated the trend towards achieving better results with the endoscopic technique compared to the microscope in terms of the degree of tumor resection. Yu et al. [16] also had similar results in their systematic review of 19 articles in 2017; they reviewed 3847 patients in the two groups. They concluded that there was a statistically significant difference in the rate of gross total resection between the two groups favoring endoscopic approach at 73% versus 60% for the microscopic group. There was no comment on the tumor volume reduction though.
In Rotenberg et al. systematic review of 11 studies, they mentioned the results from Cappabianca et al. to support the more favorable outcome of the endoscopic resection in achieving gross total resection in 90% of cases compared to 60% for the microscopic cases; there was no mention of statistical significance of the results. Yet, some articles in the same review did not find any statistically significant supremacy of either approaches [8, 10, 15]. Eseonu et al. [17] also found statistically insignificant difference in volume reduction in their study on 384 patients in 2017.
Conclusions
Endoscopic transsphenoidal approach to sellar tumors is a relatively new technique, yet it was noted in our study among other to have an easy learning curve, with a rapid acquire of experience among surgeons. It proved supremacy in various aspects when compared to the microscopic approach on our series, although some of these results did not prove to be statistically significant, yet the general trend was towards favoring volume reduction, especially in higher Knosp grade tumors, mean of hospital stay, and in the incidence of CSF leak, especially those requiring reoperation. The only parameter favoring microscopic approach was the surgery duration, yet this can be attributed to the time taken for the nasoseptal flap which was done routinely in almost all cases of the endoscopic surgeries. Also, the longer mean duration taken in the endoscopic cases can be attributed to the fact that those cases were done in the early transition to endoscope by the surgical team.
Abbreviations
- CSF:
-
Cerebrospinal fluid
- MRI:
-
Magnetic resonance images
- NFPA:
-
Non-functioning pituitary adenomas
References
Karppinen A, Kivipelto L, Vehkavaara S, Ritvonen E, Tikkanen E, Kivisaari R, et al. Transition from microscopic to endoscopic transsphenoidal surgery for nonfunctional pituitary adenomas. World Neurosurg. 2015;84(1):48–57.
Rolston JD, Han SJ, Aghi MK. Nationwide shift from microscopic to endoscopic transsphenoidal pituitary surgery. Pituitary. 2016;19(3):248–50.
Knosp E, Steiner E, Kitz K, Matula C. Pituitary adenomas with invasion of the cavernous sinus space: a magnetic resonance imaging classification compared with surgical findings. Neurosurgery. 1993;33(4):610–7 discussion 617–8.
Starke RM, Raper DMS, Payne SC, Vance ML, Oldfield EH, Jane JA. Endoscopic vs microsurgical transsphenoidal surgery for acromegaly: outcomes in a concurrent series of patients using modern criteria for remission. J Clin Endocrinol Metab. 2013;98(8):3190–8.
Dallapiazza R, Bond AE, Grober Y, Louis RG, Payne SC, Oldfield EH, et al. Retrospective analysis of a concurrent series of microscopic versus endoscopic transsphenoidal surgeries for Knosp Grades 0–2 nonfunctioning pituitary macroadenomas at a single institution: clinical article. J Neurosurg. 2014;121(3):511–7.
O’Malley BW, Grady MS, Gabel BC, Cohen MA, Heuer GG, Pisapia J, et al. Comparison of endoscopic and microscopic removal of pituitary adenomas: single-surgeon experience and the learning curve. Neurosurg Focus. 2008;25(6):E10.
Cho D-Y, Liau W-R. Comparison of endonasal endoscopic surgery and sublabial microsurgery for prolactinomas. Surg Neurol. 2002;58(6):371–5.
Higgins TS, Courtemanche C, Karakla D, Strasnick B, Singh RV, Koen JL, et al. Analysis of transnasal endoscopic versus transseptal microscopic approach for excision of pituitary tumors. Am J Rhinol. 2008;22(6):649–52.
Casler JD, Doolittle AM, Mair EA. Endoscopic surgery of the anterior skull base. Laryngoscope. 2005;115(1):16–24.
Jain AK, Gupta AK, Pathak A, Bhansali A, Bapuraj JR. Excision of pituitary adenomas: randomized comparison of surgical modalities. Br J Neurosurg. 2007;21(4):328–31.
Cappabianca P, Alfieri A, Colao A, Ferone D, Lombardi G, de Divitiis E. Endoscopic endonasal transsphenoidal approach. Skull Base Surg. 1999;9(2):109–17.
White DR, Sonnenburg RE, Ewend MG, Senior BA. Safety of minimally invasive pituitary surgery (MIPS) compared with a traditional approach. Laryngoscope. 2004;114(11):1945–8.
Neal JG, Patel SJ, Kulbersh JS, Osguthorpe JD, Schlosser RJ. Comparison of techniques for transsphenoidal pituitary surgery. Am J Rhinol. 2007;21(2):203–6.
Duz B, Harman F, Secer HI, Bolu E, Gonul E. Transsphenoidal approaches to the pituitary: a progression in experience in a single centre. Acta Neurochir. 2008;150(11):1133–8 discussion 1138-1139.
Choe J-H, Lee K-S, Jeun S-S, Cho J-H, Hong Y-K. Endocrine outcome of endoscopic endonasal transsphenoidal surgery in functioning pituitary adenomas. J Korean Neurosurg Soc. 2008;44(3):151–5.
Yu S-Y, Du Q, Yao S-Y, Zhang K-N, Wang J, Zhu Z, et al. Outcomes of endoscopic and microscopic transsphenoidal surgery on non-functioning pituitary adenomas: a systematic review and meta-analysis. J Cell Mol Med. 2018;22:2023–7.
Eseonu CI, ReFaey K, Rincon-Torroella J, Garcia O, Wand GS, Salvatori R, et al. Endoscopic versus microscopic transsphenoidal approach for pituitary adenomas: comparison of outcomes during the transition of methods of a single surgeon. World Neurosurg. 2017;97:317–25.
Availability of data and materials
The dataset supporting the conclusions of this article is included within the article (and its additional file).
Author information
Authors and Affiliations
Contributions
The first author (HAS) had a substantial role in the study design, data acquisition, and interpretation. In addition, the first co-author (AEDE) actively participated in the data acquisition and interpretation, statistical work, and revision of the manuscript while the second co-author (HAM) was involved critically in the study design, data acquisition, and drafting of the manuscript. The third co-author (AAE) participated in the data collection and interpretation and in drafting of the manuscript. The forth co-author (AY) carried out the task of measuring radiological data and documentation of the findings, and she participated in manuscript revision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
An approval from the research ethics committee of the faculty of medicine at Ain Shams University (reference number: FWA 00006444) was obtained on 14/2/2018. Being a retrospective study, patients’ consents for participation were not applicable.
Consent for publication
As the manuscript contains no identifiable human data, such consent was not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Sabry, H.A., Elayouty, A.E.D., Mashaly, H.A. et al. Surgical outcome of non-functioning pituitary adenomas: a comparative study between microscopic and endoscopic techniques. Egypt J Neurosurg 33, 18 (2018). https://doi.org/10.1186/s41984-018-0019-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41984-018-0019-2