Abstract
Disorders of Arousal (DOA) are mental and motor behaviors arising from NREM sleep. They comprise a spectrum of manifestations of increasing intensity from confusional arousals to sleep terrors to sleepwalking.
Although DOA in childhood are usually harmless, in adulthood they are often associated with injurious or violent behaviors to the patient or others. Driving motor vehicles, suspected suicide, and even homicide or attempted homicide have been described during sleepwalking in adults. Furthermore, adult DOA need to be differentiated from other sleep disorders such as Sleep-related Hypermotor Epilepsy or REM Sleep Behavior Disorder.
Although many aspects of DOA have been clarified in the last two decades there is still a lack of objective and quantitative diagnostic criteria for DOA.
Recent advances in EEG analysis and in the semiological characterization of DOA motor patterns have provided a better definition of DOA diagnosis.
Our article focuses on the DOA diagnostic process describing accurately the newest DOA clinical, EEG and video-polysomnographic tools in order to aid clinicians in DOA assessment.
Similar content being viewed by others
Background
Disorders of Arousal (DOA) are NREM parasomnias characterized by partial awakening from deep sleep in which the subjects are partially or totally unconscious, with inappropriate or absent responsiveness to the efforts of others to intervene or redirect them. Partial or complete amnesia for the episode is frequent (American Academy of Sleep Medicine 2014).
According to the Third Edition of the International Classification of Sleep Disorders (ICSD-3), DOA include confusional arousals (CA), sleepwalking (SW) and sleep terrors (ST). These manifestations share a similar genetic and familial transmission, pathophysiology linked to incomplete arousal from slow-wave sleep and trigger priming due to factors that deepen or fragment sleep (Table 1).
DOA typically have onset in childhood with a prevalence ranging from 13 to 39% (probably related to the abundance of slow-wave sleep at this age) and tend to decrease with age (Petit et al. 2007). However, recent studies have reported that DOA prevalence in adulthood, ranging from 1.6 to 2.4%, is not a rare condition (Ohayon et al. 1999).
DOA, and in particular somnambulism, are usually harmless in childhood but often associated with injurious or violent behaviors to the patient or others in adulthood (Guilleminault et al. 1995; Schenck et al. 1989; Lopez et al. 2013).
Driving motor vehicles, suspected suicide, and even homicide or attempted homicide have been described during somnambulism in adults, raising fundamental medico-forensic implications (Cartwright 2004; Siclari et al. 2010). Furthermore, especially in adulthood, DOA need to be differentiated from other sleep motor disorders such as Sleep-related Hypermotor Epilepsy (SHE) and REM Sleep Behavior Disorder (RBD). SHE is sleep-related focal epilepsy characterized by complex, often bizarre motor behaviors, including asymmetrical tonic or dystonic posture. Differential diagnosis between DOA and SHE is not always easy due to the possible presence of violent behaviors, complex automatisms, ambulation, and vocalizations in both conditions (Provini et al. 1999; Tinuper et al. 2007; Bisulli et al. 2012; Licchetta et al. 2017). The occurrence in the first part of the night, the absence of stereotypical and abnormal movements, such as dystonic and dyskinetic postures, the long duration of the episodes, and the low rate of same-night recurrence are DOA key features (Provini et al. 1999, 2011; Tinuper et al. 2007) (Table 2). RBD is characterized by episodes of motor agitation of varying intensity arising during REM sleep because the absence of the physiological muscle atonia of REM sleep permits the “acting out” of dreams. Unlike DOA, RBD is characterized by late onset (over 50 years of age), a male predominance, an occurrence of episodes in the last third of the night, and a frequent memory of dream mentation (Schenck et al. 1986; Dauvilliers et al. 2018) (Table 2).
Although many aspects of DOA have been clarified in the last two decades, objective and quantitative diagnostic criteria for DOA are lacking (Castelnovo et al. 2018). Description of DOA episode semiology and EEG markers through video-polysomnography (VPSG) have been recently reassessed in detail (Derry et al. 2009; Loddo et al. 2018; Lopez et al. 2018). This article focuses on new DOA diagnostic tools in order to aid clinicians and researchers in DOA assessment.
Diagnosis
Clinical presentation
DOA can usually be diagnosed based on careful history-taking alone (Mason and Pack 2007). Evaluation should include a comprehensive medical history, a physical, neurological, and developmental examination, and a sleep-wake schedule, including a detailed description of the nocturnal events, ideally provided by bed partners or parents. Clinical diagnosis of DOA is mainly based on the criteria established in the ICSD-3 (American Academy of Sleep Medicine 2014).
Confusional arousals
CA are episodes during which the subject sits on the bed and looks around as if confused (American Academy of Sleep Medicine 2014). CA often begin with automatic movements, vocalizations or moaning and can progress to thrashing about in bed or violent behaviors towards oneself or others. Individuals usually appear with slow mentation and have poor reactivity to environmental stimuli; attempts to awaken the person are often unsuccessful and may be met with vigorous resistance. CA need to be differentiated from sleep inertia, a transitional state of lowered arousal occurring immediately after awakening from sleep and producing a temporary decrement in subsequent performances (Roth et al. 1972; Tassi and Muzet 2000; Trotti 2017). However, it is not clear whether sleep drunkenness, a severe phenotype of sleep inertia should be classified as CA. Sleep drunkenness is frequently observed in idiopathic hypersomnia and characterized by confusion, slurred speech, slowness, incoordination, and amnesia lasting up to several minutes following awakening from sleep in the morning (Trotti 2017).
Sleep terrors
ST are the most extreme and dramatic form of DOA. Episodes typically start with a cry or a piercing scream associated with intense neurovegetative symptoms such as mydriasis, tachycardia, tachypnea, sweating, flushing of the skin, increased muscle tone. Subjects usually sit on the bed and do not respond to external stimuli. The episodes usually last no more than a few minutes in adults, and afterward, subjects usually relax and return spontaneously to sleep. However, ST episodes can be followed by CA, especially if the bed partner tries to awake the subject. Facial expressions could reflect intense fear. Episodes are often accompanied by incoherent vocalizations and agitated motor activity as if reacting to imminent danger. Although appearing alert, with eyes open, subjects may not recognize their family members and any attempt at consolation is fruitless and may serve only to prolong or even intensify the episode. If the patient wakes up at the end of the episode as may happen in older children or adults for long episodes, he/she may describe a feeling of primitive threat or danger but rarely offer the extended sequence of mental images resembling a dream (Kales et al. 1980; Meltzer and Mindell 2006; Provini et al. 2011; American Academy of Sleep Medicine 2014). ST need to be differentiated from nightmares, which are vivid dreams associated with intense and negative emotional content that awake patients from sleep (Levin and Fireman 2002). Compared to ST, nightmares are more common during the second half of the night (because they occur during REM sleep) and are not characterized by motor activity during sleep or confusion following the awakening. Furthermore, the memory of the event is common, people are fully awake, and report an appropriate and detailed description of dream imagery (Sheldon 2004; Mason and Pack 2007) (Table 2).
Sleepwalking
SW episodes may start with a CA. Episodes can also start with the subject getting out of bed and walking or also “jumping out” of bed and running. Behaviors may be simple and purposeless or complex and prolonged. Walking may end spontaneously, sometimes in inappropriate places, or the subject may go back to bed, lie down and resume sleeping without reaching conscious awareness. The subject is disorientated in time and space, with slow speech, markedly reduced mental activity and inappropriate answers to questions or requests made to him/her. Despite the reduced perception of external stimuli, as the result of blocked sensory stimuli, the individual may appear awake, with reduced vigilance and impaired cognitive response (Kavey et al. 1990; Crisp 1996; Plante and Winkelman 2006; American Academy of Sleep Medicine 2014). Often there is severe anterograde and retrograde amnesia. Dreaming typically is not present, but sleepwalkers may recount limited mentation of their motivations for their behavior, especially if awakened during an episode (Oudiette et al. 2009).
Self-report questionnaires
Several tools may be used to screen subjects at high risk for DOA, evaluate their severity, and assess the benefit of treatment. In contrast to RBD, there are very few instruments developed for DOA.
The MUPS is a self-administered questionnaire that assesses 21 different nocturnal behaviors and disorders with a single question, including SW, ST, CA. The MUPS assesses the past or current frequency of each behavior. In addition, for each item, it is asked to report if the behavior is observed by the sleeper themselves and/or by others. The psychometric properties of the MUPS were assessed in patients with various psychiatric sleep disorders and healthy controls. The MUPS has a sensitivity ranging from 83 to 100% and a specificity ranging from 89 to 100% for the diagnosis of the three main clinical presentations of DOA (Fulda et al. 2008).
The Paris Arousal Disorders Scale (PADS) is a self-administered questionnaire designed to screen and assess the severity of DOA. The PADSS consists of 17 items related to parasomniac behaviors (with two components, wandering and violence/handling), one item for their frequency per night, and five items evaluating consequences and daytime functioning. The total score ranges from 0 to 50. The threshold of > 13/50 correctly identified patients with SW and/or ST from healthy controls (sensitivity 83.6%, specificity 98.1%) and from patients with RBD (specificity of 89.5%) (Arnulf et al. 2014).
Video recording at home
A homemade video using a camera applied in the patient’s bedroom is a good option to record motor episodes of different origin such as epileptic seizures, psychogenic or other events (Johansen et al. 1999; Sartori et al. 2008; Cuppens et al. 2012). Home video recordings can capture rare episodes difficult to record with overnight video-EEG polysomnography in a sleep lab, picking up semiological features lacking in the history provided by the caregivers of the patients (Sartori et al. 2008; Ramanujam et al. 2018). Many authors concluded that also in a setting with limited resources, mobile phones, which are easy to use and not technologically challenging, can be harnessed to capture motor episodes to diagnose them accurately (Dash et al. 2016).
Considering the widespread availability of video cameras and video phones, the analysis of homemade video recordings of DOA together with the historical features, could become an important tool for a correct diagnosis. The only report describing the use of home video for DOA was performed in 2013 by Mwenge et al. In this study an adult sleepwalker monitored her behaviors during 36 nights documenting complex prolonged episodes not usually observed during ambulatory VPSG and providing the tools for differentiating SW from seizures (non-stereotyped vs. stereotyped behaviors) (Mwenge et al. 2013).
Therefore, home video recordings could be a relevant tool for DOA diagnosis. It confirms DOA when clinical history is suggestive of DOA and supports the diagnostic process when clinical history is not clear (e.g., no episode memory; subjects sleeping alone; witnesses who cannot describe episodes accurately) or when it is not completely suggestive of DOA (adult onset; high frequency of the episodes; suspected stereotyped behaviors).
Polysomnography
Sleep macrostructure
Sleep macrostructure is a term used to indicate the architecture of sleep based on the method standardized by Rechtshaffen and Kales which allows the construction of hypnic diagrams (i.e. hypnograms) and conventional sleep measures based on 30-s epochs (Rechtschaffen and Kales 1968). Until recently, polysomnography was considered to be of limited value in differentiating patients with DOA from normal sleepers and is thus not indicated for the routine evaluation of NREM sleep parasomnia. Polysomnography is usually performed to rule out differential diagnoses and to assess other potentially associated sleep disorders, such as obstructive sleep apnea syndrome, which can coexist with DOA.
Most of the studies examining the overall sleep macrostructure in DOA revealed contrasting results, with no major findings associated with DOA (Zucconi et al. 1995; Espa et al. 2000; Schenck et al. 1998; Blatt et al. 1991). A recent study on the largest sample of DOA patients and controls, who underwent one-night VPSG recording, reported a reduction of stages 1 and 2 NREM sleep and an increase of REM sleep percentages (Lopez et al. 2018). The authors also found a longer Slow Wave Sleep (SWS) duration and a shorter latency to SWS in patients in comparison with controls.
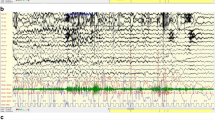
Case-control studies consistently found increased arousals and/or microarousals from SWS in patients with DOA compared with healthy controls (Blatt et al. 1991; Brion et al. 2012; Espa et al. 2002; Espa et al. 2000; Gaudreau et al. 2000; Joncas et al. 2002; Oudiette et al. 2009; Schenck et al. 1998; Uguccioni et al. 2015). Excessive SWS fragmentation appears to represent a typical polysomnographic pattern in DOA. One recent study provided a scoring method to quantify such fragmentation. The authors defined SWS interruption events as (1) the occurrence of abrupt EEG frequency shifts on the central or occipital leads with a combination of theta and alpha waves, frequencies > 16 Hz and lasting 3 to 15 s (i.e., microarousals); or (2) similar events but lasting > 15 s (i.e., awakenings); or (3) events with persistent delta waves (0.5-3 Hz) on central derivations associated with increased muscle activity and lasting > 3 s. The sum of all SWS interruptions per hour of SWS was named SWS fragmentation index (SWSFI). A twice higher SWSFI was found in DOA patients in comparison with healthy controls, this index offering satisfactory classification performances, with a sensitivity and specificity around 80% obtained with a 6.8/h cut-off. Of interest, the SWSFI is a scoring method easy to set up in clinical practice, with an excellent inter-rater agreement (Fig. 1) (Lopez et al. 2018).
Polysomnographic characteristics of a patient with Disorders of Arousal (DOA) and a healthy adult. a: The hypnogram shows an excessive amount of Slow Wave Sleep (SWS) interruptions, frequently characterized by slow/mixed post-arousal EEG activity. Three SWS interruptions are accompanied by complex behavioral manifestations defining parasomniac episodes (lower panel). During such interruption, the polysomnography reveals slow or mixed sleep-wake features, with motor and autonomic activations (upper panel). b: By contrast, SWS continuity is preserved in healthy subjects with rare interruptions (lower panel). The polysomnography reveals a fast post-arousal EEG activity during SWS interruption (upper panel)
Sleep microstructure
Sleep microstructure is a term used to indicate the architecture of sleep based on scoring methods using intervals less than 30-s allowing us to obtain information regarding k-complex, sleep spindles, delta bursts and cyclic alternating pattern (Parrino et al., 2017). Zucconi et al. finely studied sleep microstructure through the analysis of cyclic alternating pattern (CAP) in 13 DOA patients (Zucconi et al. 1995). CAP is a periodic EEG activity of non-REM sleep characterized by sequences of transient electrocortical events that are distinct from background EEG activity and recur at up to 1 min intervals (Terzano et al. 2002). In DOA, the sleep microstructure is characterized by an increase in CAP rate (a measure of NREM instability with a high level of arousal oscillation), in the number of the CAP cycles, and arousals with EEG synchronization (Zucconi et al. 1995). An increased CAP rate was further reported in children with SW and concomitant sleep respiratory disorders (Guilleminault et al. 2005).
Quantitative EEG studies documented an abnormal temporal course and a decrease of slow wave activity during the first sleep cycle (Espa et al. 2000; Gaudreau et al. 2000), and a significant decrease in sleep spindle number during the first cycle of sleep (especially in SWS), confirming the hypothesis of alterations in the sleep homeostasis process in DOA (Espa et al. 2000). A recent high-density EEG study conducted in 15 DOA patients confirmed the decrease in slow wave activity over the centroparietal regions (cingulate, motor, and sensorimotor associative cortices) from SWS during the first half of the night, with similar patterns during REM sleep and wake, even in the absence of any detectable clinical or electrophysiological sign of arousal (Castelnovo et al. 2016). These microarchitectural sleep characteristics are consistently associated with DOA; however, their ability to contribute to the diagnosis of DOA has not been assessed, with no pathological cut-off established so far. Furthermore, these analyses required time, specific software, and expertise that limit their use in clinical routine for the diagnosis of DOA.
EEG characteristics of arousals during SWS
Hypersynchronous delta wave activity (HSD) has been the first EEG marker to be described in relation to DOA episodes. This EEG pattern, similar to that seen in partial arousals in healthy children, was characterized by continuous high-voltage (> 150-uV) delta waves. Further studies demonstrated that HSD has low specificity for the DOA diagnosis, being found in patients with sleep-disordered breathing and healthy subjects after sleep deprivation. In a study on 10 adult sleepwalkers and 10 matched controls investigated polysomnographically during a baseline night and following 38 h of sleep deprivation, HSD showed a clear frontocentral gradient across all subjects during both baseline and recovery sleep, with low specificity for the diagnosis of NREM parasomnias. The coexistence of arousal and deep sleep in the 20 s immediately preceding the onset of DOA has been confirmed with spectral analysis and by stereo EEG. An intracerebral stereo EEG study documented the coexistence of a sleep-like pattern (delta waves over frontoparietal associative networks and spindles in the hippocampus) and wake-like patterns (low-voltage fast activity over the motor cortex and limbic structures) during CA (Terzaghi et al. 2009; Sarasso et al. 2014).
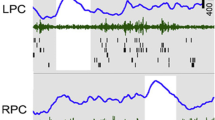
A study on 38 adults presenting with injurious SW and ST analyzed post-arousal EEG characteristics of arousals in SWS, associated or not with DOA episodes. The authors confirmed the presence of a slow EEG pattern, characterized by predominant diffuse and synchronous slow delta activity. They also described two other EEG patterns, one characterized by diffuse and irregular, moderate-to-high voltage delta and theta activity intermixed with alpha and beta activity (Fig. 2) and the other characterized by prominent alpha and beta activity, at times intermixed with moderate voltage theta activity. Irrespective of specific EEG patterns, delta activity was present in 44% of the post-arousal EEGs (Schenck et al. 1998). These EEG patterns were subsequently confirmed by other studies and revealed that the slower patterns were more likely to accompany progressive onset rather than abrupt onset DOA episodes. The diagnostic value of these EEG patterns was recently assessed in a case control study. The authors classified each SWS interruption according to the predominant slow, mixed or fast EEG activity during the first three seconds of the motor behavior. They calculated three indices being the sum of all SWS interruptions classified as fast, mixed, or slow patterns per hour of SWS. They found a higher slow/mixed arousal index in DOA patients in comparison with healthy controls (7.0/h versus 1.6/h). They proposed two pathological thresholds, the lower (2.5/h) having an excellent sensitivity of 94% and the higher (6/h) a specificity of 100%. This assessment, however, requires scoring skills and time and appears to be a more appropriate scoring method for research settings rather than for clinical routine (Lopez et al. 2018).
Typical Confusional Arousal episode. On the top: polysomnographic tracing. The episode arises during Slow Wave Sleep. Motor onset corresponds to an EEG artifact followed by the appearance of theta-delta activity on the anterior regions and of alpha and beta activity on the posterior regions. On the bottom: photographic sequences of the episode. The patient is sleeping in a supine position, raises his head, raises his trunk looking around; lies down and flexes the left thigh; lies down recovering sleep
Autonomic activation
Early studies found that DOA episodes, especially ST, were associated with intense autonomic activation, a dramatic increase of heart rate and respiratory amplitude, and decrease in skin resistances (Fisher et al. 1974; Schenck et al. 1998). Such autonomic activation could help clinicians to improve the diagnostic procedure and differentiate DOA episodes from normal arousals, and from other complex motor behaviors arising from sleep. A recent study attempts to characterize autonomic activation before and after DOA episodes (ST and CA), nocturnal epileptic behaviors, and normal arousals from SWS. The authors did not find any major differences in heart rate patterns among the three types of events (Peter-Derex et al. 2018).
Video-polysomnography
VPSG has substantial diagnostic value and is considered the gold standard for every kind of motor manifestation during sleep providing the recordings of motor events and behaviors during sleep and their correlation with EEG and polygraphic parameters (e.g., tachycardia, respiratory changes) (Aldrich and Jahnke 1991). According to the update of the AASM Practice Parameters for the Indications for Polysomnography and Related Procedures drafted in 2005, the minimum channels required for the diagnosis of DOA include an EEG expanded bilateral montage (Kushida et al. 2005). VPSG findings revealed that DOA behaviors are usually observed during the first sleep cycles, preferentially related to the first episode of SWS, but they also can occur in stage 2 and be distributed throughout the night (Espa et al. 2000; Guilleminault et al. 1995; Kavey et al. 1990; Zucconi et al. 1995). Nevertheless, while EEG patterns of DOA have been extensively studied, only small case series or case reports have reported the VPSG semiological features until recently.
Kavey et al. made the first attempt to describe DOA semiology in 1990, evaluating the VPSG recordings of 10 consecutive adults with SW often accompanied by violent behavior or self-injury. The authors described three types of behavior differing in intensity: (1) dramatic episodes with abrupt, impulsive movements, sometimes culminating in attempts to get out of bed; (2) episodes during which the patient arose quickly and moved to a sitting or kneeling position, often with a short and clear somniloquy; (3) verbalization accompanying behavior such as kicking or gesticulating (Kavey et al. 1990).
One year later, Blatt and colleagues enrolled 24 young adults referred to the sleep laboratory for SW. Although no SW episodes were recorded, other DOA motor activities were described such as sitting up in bed, performing semi-purposeful movements and gestures and lying down again; raising both legs in the air several times in the supine position; talking or screaming (Blatt et al. 1991). A similar description was reported in a VPSG study designed to evaluate sleep microstructure in 21 DOA patients, in which abnormal motor movements of the arms or trunk with some semi-purposeful movements of sitting up or talking and screaming have been described (Zucconi et al. 1995).
In another study, the complexity of motor behaviors during sleep was classified on a 3-point scale. Level 1 was scored when a change in bodily position characterized the episode (e.g., turning and resting on one’s hands) or any simple behaviors (e.g., playing with the bed sheets). Level 2 was scored if the patient executed a complex behavior such as sitting up in bed, resting on his/her knees, or trying to get out of bed. Any event during which the subject left the bed was scored as 3 (Joncas et al. 2002). Based on this behavioral characterization, the study of Lopez et al. assessed the diagnostic value of the occurrence of such motor episodes in VPSG performed in the clinical routine evaluation of patients with DOA (n = 100) compared to controls (n = 50). In combination with both the frequency and EEG characteristics of SWS interruptions (i.e., SWSFI and slow/mixed arousal index), the video-based analysis significantly increased the classification rate above 90% (Lopez et al. 2018).
A more accurate semiological description of DOA episodes was carried out by Derry et al. (Derry et al. 2009). The authors recorded 57 DOA episodes classified into three main behavioral patterns: 1) arousal behaviors; 2) non-agitated motor behavior; 3) distressed emotional behavior. Arousal behaviors included eye-opening, head elevation, and staring; face rubbing, yawning, scratching, moaning, and mumbling also sometimes occurred. Non-agitated motor behavior included actions such as sitting, manipulating objects (such as EEG equipment) or searching behaviors (e.g., looking over the side of the bed). Distressed emotional behavior was characterized by fearful behavior, facial expression, and speech content. Sitting or standing, screaming, and frantic searching, recoiling, or evasive behaviors were prominent. The three behavior patterns occurred in various combinations and sequences with an apparent hierarchy.
Finally, an objective, accurate description of DOA episodes in a large sample of adult patients with DOA was performed in 2017 by Loddo et al. Fifty-nine VPSG of 30 consecutive adult patients with DOA were reviewed and 184 DOA episodes were analyzed. DOA were classified according to three different semiological motor patterns characterized by increasing intensity, complexity and duration with an apparent hierarchy: simple arousal movements (pattern I or SAMs); rising arousal movements (pattern II or RAMs) and complex arousal with ambulatory movements (pattern III or CAMs). SAMs were the most represented patterns (93%) and were characterized by 3 different motor expressions: A) head flexion/extension (Fig. 3); B) head flexion/extension and limb movement (Fig. 4); C) head flexion/extension and partial trunk flexion/extension (Fig. 5). Opening eyes (71%), exploring the environment with eyes opened (63%) or bringing hands to face (54%) were the most frequent recorded behaviors. Speaking was observed in 25% of the episodes. RAMs were characterized by trunk flexion followed by sitting with feet in or out of the bed (Fig. 6). At the onset, the behavior was like that of SAMs although screaming (40%), speaking (54%), bringing a hand to the face (75%) were more frequent. Finally, CAMs were characterized by ambulatory movements with patients sitting up, getting out of bed, and walking. Manipulating objects, speaking, and exploring the environment were frequently observed. Speaking (89%) and screaming (63%) were more common than other patterns (Fig. 7). The duration of the three different motor patterns increased progressively from SAMs to CAMs from a few seconds to three minutes. This study confirmed a hierarchical continuum in the behavioral manifestations of DOA, characterized by increased intensity, complexity, and duration of the recorded episodes.
In-lab recording vs. home recording
In clinical samples, 30 to 59% of patients with DOA displayed at least one parasomniac episode during a single night VPSG assessment (Lopez et al. 2018; Pilon et al. 2008). The occurrence of a typical parasomniac behavior during the routine VPSG evaluation has thus a low sensitivity for the positive diagnosis of DOA. Sleep deprivation is a well-known predisposing factor that increases the frequency of parasomniac episodes in patients with DOA (Lopez et al. 2013). Some studies attempted to increase the opportunity to record parasomniac episodes with a standardized protocol using controlled sleep deprivation up to 38 h, and the combination of 25-h sleep deprivation and forced arousals from SWS by auditory stimuli (Mayer et al. 1998; Joncas et al. 2002; Zadra et al. 2004; Pilon et al. 2008). Compared to baseline recordings, these methods increased the probability to record at least one parasomniac episode in patients with DOA (from 30 to 100%). Such protocols also increased the behavioral complexity and intensity of parasomniac episodes. Although these protocols would improve the diagnostic procedure of DOA, they can be difficult to be routinely used in sleep labs and thus may be considered as a research tool instead of a practical clinical test. In-lab video-EEG recording is time consuming, expensive, and requires admission to the hospital with generally long waiting lists. Moreover, in patients with less frequent events, the probability of capturing an episode during a single night is very low. Considering the widespread availability of video cameras and videophones, the analysis of homemade video recordings with the historical features could become an important tool for helping physicians in DOA recognition (Nobili 2009).
Conclusion
DOA can usually be diagnosed based on careful history-taking alone in typical cases, especially in childhood. When history taking is insufficient homemade video could be a relevant tool for DOA diagnosis. VPSG is required in atypical presentations in particular if events are repetitive or stereotypic, occur frequently, or in the presence of concurrent sleep pathologies (such as sleep-related breathing disorders or restless legs syndrome) (Fig. 8). Further studies are needed to define standardized guidelines or protocols for the evaluation of DOA episodes with VPSG (how many nights should be run or whether there should be prior sleep deprivation or attempts to stimulate an episode during slow-wave sleep).
Recent advances in EEG analysis and in the semiological characterization of DOA motor pattern have provided a better definition of DOA characteristics. It is clear that the three traditional subtypes of DOA (CA, ST, and SW) could be an oversimplification and they probably do not exist as three nosologically and biologically distinct entities. Rather, DOA comprises a composite of different behavioral patterns, on a hierarchical continuum, the proportion of which may vary between triggers, events, patients, and age.
According to the classification system widely used in sleep medicine practice (ICSD-3), the diagnosis of DOA is based only on clinical criteria, in contrast to other parasomnias, particularly RBD, which requires additional polysomnographic features (i.e., REM sleep without atonia). The lack of objective and quantitative diagnostic criteria for DOA remains a major issue and prevents the development of collaborative clinical and research studies with good quality standards.
We described here some potential new diagnostic tools to improve the clinical and neurophysiological characterization of DOA. Self-report questionnaires and homemade video are underused but useful tools to provide a better clinical characterization of DOA. Our review highlights the potential interest of VPSG for the diagnosis of DOA. In a routine clinical setting, VPSG may provide objective findings that support the diagnosis of DOA. It can reveal specific sleep macrostructure abnormalities such as excessive SWS fragmentation, typical post-arousal EEG characteristics of SWS interruptions, associated or not with parasomniac behaviors. VPSG also allowed a better semiological characterization of motor and behavioral manifestations in DOA. Nevertheless, a consensus based on the behavioral definition of a DOA episode versus physiological arousal is still lacking. Such a consensus is necessary to provide new clinical and video-polysomnographic-based diagnostic criteria for DOA, to be included in the future revision of the classifications system.
Availability of data and materials
The authors declare that all studies referenced in this article can be found on PubMED/Medline.
Abbreviations
- CA:
-
Confusional Arousals
- CAMs:
-
Complex Arousal with Ambulatory Movements
- DOA:
-
Disorders of Arousal
- HSD:
-
Hypersynchronous delta wave activity
- ICSD-3:
-
International Classification of Sleep Disorders
- RAMs:
-
Rising Arousal Movements
- RBD:
-
REM sleep Behavior Disorder
- SAMs:
-
Simple Arousal Movements
- SHE:
-
Sleep-related Hypermotor Epilepsy
- ST:
-
Sleep Terrors
- SW:
-
Sleepwalking
- SWS:
-
slow wave sleep
- VPSG:
-
video-polysomnography
References
Aldrich MS, Jahnke B. Diagnostic value of video-EEG polysomnography. Neurology. 1991;41(7):1060–6.
American Academy of Sleep Medicine. International Classification of Sleep Disorders, 3rd ed. Darien: American Academy of Sleep Medicine; 2014.
Arnulf I, Zhang B, Uguccioni G, Flamand M, de Fontréaux AN, Leu-Semenescu S, et al. A scale for assessing the severity of arousal disorders. Sleep. 2014;37(1):127–36.
Bisulli F, Vignatelli L, Naldi I, Pittau F, Provini F, Plazzi G, et al. Diagnostic accuracy of a structured interview for nocturnal frontal lobe epilepsy (SINFLE): a proposal for developing diagnostic criteria. Sleep Med. 2012;13(1):81–7.
Blatt I, Peled R, Gadoth N, Lavie P. The value of sleep recording in evaluating somnambulism in young adults. Electroencephalogr Clin Neurophysiol. 1991;78(6):407–12.
Brion A, Flamand M, Oudiette D, Voillery D, Golmard J-L, Arnulf I. Sleep-related eating disorder versus sleepwalking: a controlled study. Sleep Med. 2012;13(8):1094–101.
Cartwright R. Sleepwalking violence: a sleep disorder, a legal dilemma, and a psychological challenge. Am J Psychiatry. 2004;161(7):1149–58.
Castelnovo A, Lopez R, Proserpio P, Nobili L, Dauvilliers Y. NREM sleep parasomnias as disorders of sleep-state dissociation. Nat Rev Neurol. 2018;14(8):470-81.
Castelnovo A, Riedner BA, Smith RF, Tononi G, Boly M, Benca RM. Scalp and source power topography in sleepwalking and sleep terrors: a high-density EEG study. Sleep. 2016;39(10):1815–25.
Crisp AH. The sleepwalkning/night terrors syndrome in adults. Postgrad Med J. 1996;72:599–604.
Cuppens K, Chen C, Wong KB, Van de Vel A, Lagae L, Ceulemans B, et al. Using spatio-temporal interest points (STIP) for myoclonic jerk detection in nocturnal video. In: 2012 Annual International Conference of the IEEE Engineering in Medicine and Biology Society; 2012. p. 4454–7.
Dash D, Sharma A, Yuvraj K, Renjith A, Mehta S, Vasantha PM, et al. Can home video facilitate diagnosis of epilepsy type in a developing country? Epilepsy Res. 2016;125:19–23.
Dauvilliers Y, Schenck CH, Postuma RB, Iranzo A, Luppi P-H, Plazzi G, et al. REM sleep behaviour disorder. Nat Rev Dis Primer. 2018;4(1):19.
Derry CP, Harvey AS, Walker MC, Duncan JS, Berkovic SF. NREM arousal parasomnias and their distinction from nocturnal frontal lobe epilepsy: a video EEG analysis. Sleep. 2009;32(12):1637–44.
Espa F, Dauvilliers Y, Ondze B, Billiard M, Besset A. Arousal reactions in sleepwalking and night terrors in adults: the role of respiratory events. Sleep. 2002;25(8):871–5.
Espa F, Ondze B, Deglise P, Billiard M, Besset A. Sleep architecture, slow wave activity, and sleep spindles in adult patients with sleepwalking and sleep terrors. Clin Neurophysiol. 2000;111(5):929–39.
Fisher C, Kahn E, Edwards A, Davis DM, Fine J. A psychophysiological study of nightmares and night terrors. 3. Mental content and recall of stage 4 night terrors. J Nerv Ment Dis. 1974;158(3):174–88.
Fulda S, Hornyak M, Muller K, Cerny L, Beitinger P, Wetter T. Development and validation of the Munich Parasomnia Screening (MUPS). Somnologie. 2008;12:56–65.
Gaudreau H, Joncas S, Zadra A, Montplaisir J. Dynamics of slow-wave activity during the NREM sleep of sleepwalkers and control subjects. Sleep. 2000;23(6):755–60.
Guilleminault C, Lee J, Chan A, Lopes M, Huang Y, Darosa A. Non-REM-sleep instability in recurrent sleepwalking in pre-pubertal children. Sleep Med. 2005;6(6):515–21.
Guilleminault C, Moscovitch A, Leger D. Forensic sleep medicine: nocturnal wandering and violence. Sleep. 1995;18(9):740–8.
Johansen JR, Lindahl G, Sandstedt P. Home-video observation of seizures in children with epilepsy—impact on quality of family life. Seizure. 1999;8(6):356–7.
Joncas S, Zadra A, Paquet J, Montplaisir J. The value of sleep deprivation as a diagnostic tool in adult sleepwalkers. Neurology. 2002;58(6):936–40.
Kales JD, Kales A, Soldatos CR, Caldwell AB, Charney DS, Martin ED. Night terrors. Clinical characteristics and personality patterns. Arch Gen Psychiatry. 1980;37(12):1413–7.
Kavey NB, Whyte J, Resor SR, Gidro-Frank S. Somnambulism in adults. Neurology. 1990;40(5):749–52.
Kushida CA, Littner MR, Morgenthaler T, Alessi CA, Bailey D, Coleman J Jr, et al. Practice parameters for the indications for polysomnography and related procedures: an update for 2005. Sleep. 2005;28(4):499–521.
Levin R, Fireman G. Nightmare prevalence, nightmare distress, and self-reported psychological disturbance. Sleep. 2002;25(2):205–12.
Licchetta L, Bisulli F, Vignatelli L, Zenesini C, Di Vito L, Mostacci B, et al. Sleep-related hypermotor epilepsy. Neurology. 2017;88(1):70–7.
Loddo G, Sessagesimi E, Mignani F, Cirignotta F, Mondini S, Licchetta L, et al. Specific motor patterns of arousal disorders in adults: a video-polysomnographic analysis of 184 episodes. Sleep Med. 2018;41:102–9.
Lopez R, Jaussent I, Scholz S, Bayard S, Montplaisir J, Dauvilliers Y. Functional impairment in adult sleepwalkers: a case-control study. Sleep. 2013;36(3):345–51.
Lopez R, Shen Y, Chenini S, Rassu AL, Evangelista E, Barateau L, et al. Diagnostic criteria for disorders of arousal: a video-polysomnographic assessment. Ann Neurol. 2018;83(2):341–51.
Mason TBA, Pack AI. Pediatric parasomnias. Sleep. 2007;30(2):141–51.
Mayer G, Neissner V, Schwarzmayr P, Meier-Ewert K. Sleep deprivation in somnambulism. Effect of arousal, deep sleep and sleep stage changes. Nervenarzt. 1998;69(6):495–501.
Meltzer LJ, Mindell JA. Sleep and sleep disorders in children and adolescents. Psychiatr Clin North Am. 2006;29(4):1059–76.
Mwenge B, Brion A, Uguccioni G, Arnulf I. Sleepwalking: Long-term home video monitoring. Sleep Med. 2013;14(11):1226–8.
Nobili L. Can homemade video recording become more than a screening tool? Sleep. 2009;32:1544–5.
Ohayon MM, Guilleminault C, Priest RG. Night terrors, sleepwalking, and confusional arousals in the general population: their frequency and relationship to other sleep and mental disorders. J Clin Psychiatry. 1999;60:268–76.
Oudiette D, Leu S, Pottier M, Buzare M-A, Brion A, Arnulf I. Dreamlike mentations during sleepwalking and sleep terrors in adults. Sleep. 2009;32(12):1621–7.
Parrino L, Terzano M.G. Central Nervous System Arousals and Cyclic Alternating Patterns. In: Kryger M, Roth T, Dement WC editors. Principles and Practice of sleep Medicine. Philadelphia: Elsevier; 2017. p. 1576.
Peter-Derex L, Catenoix H, Bastuji H, Chouchou F. Parasomnia versus epilepsy: an affair of the heart? Neurophysiol Clin Neurophysiol. 2018;48(5):277–86.
Petit D, Touchette E, Tremblay RE, Boivin M, Montplaisir J. Dyssomnias and parasomnias in early childhood. Pediatrics. 2007;119(5):e1016–25.
Pilon M, Montplaisir J, Zadra A. Precipitating factors of somnambulism: impact of sleep deprivation and forced arousals. Neurology. 2008;70(24):2284–90.
Plante DT, Winkelman JW. Parasomnias. Psychiatr Clin North Am. 2006;29(4):969–87.
Provini F, Plazzi G, Tinuper P, Vandi S, Lugaresi E, Montagna P. Nocturnal frontal lobe epilepsy: a clinical and polygraphic overview of 100 consecutive cases. Brain. 1999;122(6):1017–31.
Provini F, Tinuper P, Bisulli F, Lugaresi E. Arousal disorders. Sleep Med. 2011;12(Suppl. 2):S22–6.
Ramanujam B, Dash D, Tripathi M. Can home videos made on smartphones complement video-EEG in diagnosing psychogenic nonepileptic seizures? Seizure. 2018;62:95–8.
Rechtschaffen A, Kales A. A manual of standardized terminology, techniques, and scoring systems for sleep stages of human subjects. Los Angeles: UCLA Brain Information Service/Brain Research Institute; 1968.
Roth B, Nevsimalova S, Rechtschaffen A. Hypersomnia with “sleep drunkenness”. Arch Gen Psychiatry. 1972;26(5):456–62.
Sarasso S, Pigorini A, Proserpio P, Gibbs SA, Massimini M, Nobili L. Fluid boundaries between wake and sleep: experimental evidence from stereo-EEG recordings. Arch Ital Biol. 2014;152(2–3):169–77.
Sartori S, Vecchi M, Toldo I, Boniver C, Bernardina BD, Laverda AM. Benign nocturnal alternating hemiplegia of childhood: the first clinical report with paroxysmal events home-video recordings. Mov Disord. 2008;23(11):1605–8.
Schenck CH, Bundlie SR, Ettinger MG, Mahowald MW. Chronic behavioral disorders of human REM sleep: a new category of parasomnia. Sleep. 1986;9(2):293–308.
Schenck CH, Milner DM, Hurwitz TD, Bundlie SR, Mahowald MW. A polysomnographic and clinical report on sleep-related injury in 100 adult patients. Am J Psychiatry. 1989;146(9):1166–73.
Schenck CH, Pareja JA, Patterson AL, Mahowald MW. Analysis of polysomnographic events surrounding 252 slow-wave sleep arousals in thirty-eight adults with injurious sleepwalking and sleep terrors. J Clin Neurophysiol Off Publ Am Electroencephalogr Soc. 1998;15(2):159–66.
Sheldon SH. Parasomnias in childhood. Pediatr Clin N Am. 2004;51(1):69–88.
Siclari F, Khatami R, Urbaniok F, Nobili L, Mahowald MW, Schenck CH, et al. Violence in sleep. Brain J Neurol. 2010;133(Pt 12):3494–509.
Tassi P, Muzet A. Sleep inertia. Sleep Med Rev. 2000;4(4):341–53.
Terzaghi M, Sartori I, Tassi L, Didato G, Rustioni V, LoRusso G, et al. Evidence of dissociated arousal states during NREM parasomnia from an intracerebral neurophysiological study. Sleep. 2009;32(3):409–12.
Terzano MG, Parrino L, Smerieri A, Chervin R, Chokroverty S, Guilleminault C, et al. Atlas, rules, and recording techniques for the scoring of cyclic alternating pattern (CAP) in human sleep. Sleep Med. 2002;3(2):187–99.
Tinuper P, Provini F, Bisulli F, Vignatelli L, Plazzi G, Vetrugno R, et al. Movement disorders in sleep: guidelines for differentiating epileptic from non-epileptic motor phenomena arising from sleep. Sleep Med Rev. 2007;11(4):255–67.
Trotti LM. Waking up is the hardest thing I do all day: sleep inertia and sleep drunkenness. Sleep Med Rev. 2017;35:76–84.
Uguccioni G, Pallanca O, Golmard J-L, Leu-Semenescu S, Arnulf I. Is sleep-related verbal memory consolidation impaired in sleepwalkers? J Sleep Res. 2015;24(2):197–205.
Zadra A, Pilon M, Joncas S, Rompré S, Montplaisir J. Analysis of postarousal EEG activity during somnambulistic episodes. J Sleep Res. 2004;13(3):279–84.
Zucconi M, Oldani A, Ferini-Strambi L, Smirne S. Arousal fluctuations in non-rapid eye movement parasomnias: the role of cyclic alternating pattern as a measure of sleep instability. J Clin Neurophysiol Off Publ Am Electroencephalogr Soc. 1995;12(2):147–54.
Acknowledgements
We thank Elena Zoni for figures and Cecilia Baroncini for English editing.
Funding
The authors declare there was no funding for this study.
Author information
Authors and Affiliations
Contributions
GL, RL, YD, FP, conceived of the study, participated in its design and coordination, performed a literature search and helped to draft the manuscript. RC helped to draft the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
Dr. Loddo received honoraria as sub-investigator activities from UCB Pharma.
Dr. Provini received honoraria for speaking engagements or consultancies from Sanofi, Bial, Fidia, Vanda Pharmaceuticals Ltd., Zambon, Eisai Japan and Italfarmaco.
Dr. Lopez received honoraria for speaking engagements and travel to conferences from UCB Pharma, Shire and HAC Pharma.
Pr. Dauvilliers received honoraria for speaking, board engagements and travel to conferences by UCB Pharma, Jazz, Theranexus, Flamel and Bioprojet.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Loddo, G., Lopez, R., Cilea, R. et al. Disorders of Arousal in adults: new diagnostic tools for clinical practice. Sleep Science Practice 3, 5 (2019). https://doi.org/10.1186/s41606-019-0037-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41606-019-0037-3