Abstract
Background
Coronavirus disease 2019 (COVID-19) has spread to almost every region and country in the world, leading to widespread travel restrictions and national lockdowns. Currently, there are limited epidemiological and clinical data on COVID-19 patients from low and middle-income countries. We conducted a retrospective single-center study of the first 100 individuals with suspected COVID-19 (between Jan. 25 and Mar. 29, 2020) admitted to San Lazaro Hospital (SLH), the national infectious diseases referral hospital in Manila, Philippines.
Results
Demographic data, travel history, clinical features, and outcomes were summarized and compared between COVID-19 confirmed and non-confirmed cases. The first two confirmed cases were Chinese nationals, admitted on Jan. 25. The third confirmed case was a Filipino, admitted on Mar. 8. Trends toward confirmed COVID-19 cases not reporting international travel and being admitted to SLH from the densely populated area of Manila city were observed during Mar. 8-29. All 42 of the 100 confirmed COVID-19 cases were adults, 40% were aged 60 years and above and 55% were male. Three were health workers. Among individuals with suspected COVID-19, confirmed cases were more likely to be older, Filipino, not report international travel history and have at least one underlying disease, particularly diabetes, report difficulty in breathing, and a longer duration of symptoms. In over 90% of non-COVID-19 cases, the alternative diagnosis was respiratory. Nine (21%) confirmed cases died. The median duration from symptoms onset to death was 11.5 (range: 8–18) days.
Conclusions
Imported COVID-19 cases have reduced but local transmission persists and there is a trend toward cases being admitted to SLH from densely populated areas. This study highlights the difficulty in diagnosing COVID-19 on clinical grounds and the importance of diagnostic capacity in all settings. Difficulty of breathing was the only symptom associated with COVID-19 infection and should alert clinicians to the possibility of COVID-19. Clinical characteristics of confirmed COVID-19 cases and a hospital case fatality rate of 21% are comparable with other settings.
Similar content being viewed by others
Introduction
Coronavirus disease 2019 (COVID-19) is a respiratory disease caused by a novel coronavirus named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [1]. Since December 2019, when initial cases were identified in Wuhan, China, COVID-19 has spread to almost every region and country in the world, leading to widespread travel restrictions and national lockdowns [1]. The World Health Organization declared a global pandemic on Mar. 11, 2020 [2]. The epidemiological and clinical characteristics of COVID-19 have been well described in a range of settings, including China, the USA, and Singapore [3,4,5]. However, there are limited reports of the epidemiological and clinical characteristics of COVID-19 from low and middle income (LMIC) countries with tropical climates.
The first COVID-19 case in the Philippines was confirmed on Jan. 31, 2020, admitted to San Lazaro Hospital (SLH), the national infectious disease referral hospital in Manila [6]. The second case was the close contact of the first case and was the first confirmed death in the country as well as the first mortality outside China. Both of the cases were imported cases (travelers from China). The Philippine government implemented travel restrictions on foreign travelers from Hubei province on Jan. 31, and then extended this to include additional countries with COVID-19 cases during February [7,8,9]. The first confirmed local transmission of COVID-19 in the country, without any travel history, was reported on Mar. 5 [10]. As of May 2, 8772 confirmed cases were reported in the Philippines [11]. In this study, we describe the epidemiological, clinical characteristics, and clinical outcomes of the first 100 individuals with suspected COVID-19 admitted to SLH by Mar. 31, 2020.
Methods
Study design and participants
We conducted a retrospective single-center descriptive study summarizing the first 100 individuals with suspected COVID-19 admitted to SLH, which serves a low-income population in Manila, the most densely populated city with Metropolitan Manila, Philippines. During this time, adult and pediatric patients with suspected COVID-19 residing in the National Capital Region of Manila were admitted to SLH, in addition to other hospitals dedicated for COVID-19 admission in the region. Admitted patients included either self-referrals (walk-in patients) or referrals from other health facilities through direct coordination or through the Regional Epidemiologic Surveillance Unit (RESU). From March 7, the Department of Health (DOH) guidelines stated that only confirmed COVID-19 patients that were severe or critical should be referred to SLH [12].
This was a retrospective analysis of anonymized routinely collected data, implemented under an existing acute respiratory tract/COVID-19 study, approved by the SLH research ethics and review unit (Ref: SLH-RERU-2020-022-I) and the School of Tropical Medicine and Global Health, Nagasaki University Ethical Committee (NU_TMGH_2020_119_1).
Procedures
We obtained data from “Case Investigation Forms (CIF)” for 2019 coronavirus disease completed by the clinical teams and submitted to the SLH epidemiology department. The CIF was designed by the Philippines DOH Epidemiology Bureau, which evolved from the SARI (severe acute respiratory illness) case report form, and collected information in the following domains: patient profile, Philippine residence, overseas employment address (if relevant), travel history, likely exposure (imported or local), clinical information, specimen information final classification (COVID-19 or not COVID-19), outcome (died or discharged). Information on whether the patient self-referred or was referred from another hospital was not systematically recorded. Selected data were encoded to create an anonymized dataset. Clarifications were discussed with the epidemiology department encoders or clinical teams. The analysis was undertaken after clinical outcomes were available for all patients.
Case definition of COVID-19 suspect
The case definition for a suspected COVID-19 individual in the Philippines has been modified over a short period of time as the epidemic has evolved. The initial decision tool released by the DOH on Jan. 21, 2020 [13], classified individuals as a suspected case, or person under investigation (PUI), if they fulfilled at least three of the following criteria: fever, respiratory infection (cough and/or coryza), residence or travel history to Wuhan, Hubei, in the 14 days prior to symptom onset, or a history of exposure such as close contact with a confirmed case [14]. The case definition was adapted on Feb. 26, 2020, with the suspected COVID-19 case criteria expanded to include all areas with travel restrictions [15]. Following the onset of community transmission, on Mar. 16, the case definition was further modified to include individuals without a travel history and added shortness of breath to the symptom list [10]. Cases were considered “imported” if a history of international travel was reported within 14 days prior to the admission, and conversely “local” if no international travel was reported within 14 days prior to the admission.
Confirmatory test for COVID-19
Laboratory confirmation for the first COVID-19 case was performed at the Victorian Medical Center (Australia) [16] and subsequently for all other cases at the Research Institute for Tropical Medicine (RITM) [17]. Nasopharyngeal and oropharyngeal swabs (NPS/OPS), and in some cases sputum and endotracheal aspirates, were obtained from patients and maintained in viral-transport medium. COVID-19 was confirmed by real-time PCR detecting SARS-CoV-2 at the RITM using the Corman et al. protocol [13].
Statistical analysis
We summarized demographic characteristics, travel history, symptoms on admission, co-morbidities by whether a suspected case tested positive for COVID-19 or not. We also summarised duration between onset of symptoms and admission. Continuous variables were expressed as mean (standard deviation, SD), median (range), and categorical variables were expressed as number (%). Fisher’s exact test was used to test for associations between categorical variables and Mann-Whitney tests were used to compare discrete variables between categories of categorical variables. All analyses were performed using Stata v15 [18].
Results
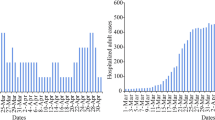
One hundred patients with suspected COVID-19 infection admitted in SLH from Jan. 25 to Mar. 29, 2020, were included in this study. Of these, 42 (42%) were identified as laboratory-confirmed COVID-19. Figure 1 shows the timeline of admission of cases indicating whether a history of international travel was reported. The first two suspected patients were admitted on Jan. 25, 2020, both of whom became confirmed cases. During Jan. 27-Mar. 7, a further 42 suspected cases were admitted, none of whom were confirmed cases. The next confirmed case was admitted on Mar. 8. From Mar. 8-29, a further 55 suspected cases were admitted, of whom 39 were confirmed cases. Figure 2 shows the approximate residence of suspected and confirmed COVID-19 cases admitted during Mar. 8-29, 2020, excluding those residents outside Metro Manila or staying in a hotel. During Mar. 8-18, 14 confirmed cases resident in Metro Manila were admitted to SLH, none of whom lived in Manila city. During Mar. 19-29, 15 confirmed cases resident in Metro Manila were admitted to SLH, of whom 8 lived in Manila city.
Timeline of admission date of the first 100 suspected COVID-19 cases to an infectious diseases hospital in Metro Manila. Cases were considered “imported” if a history of international travel was reported within 14 days prior to the admission, and conversely ‘local’ if no international travel was reported within 14 days prior to the admission
Residence of suspected and confirmed COVID-19 individuals if resident in the National Capital Region of Metropolitan Manila admitted during 8–18 March (left) and 19–29 March (right). Twenty-two individuals were admitted during Mar. 8–18, of whom 14 were confirmed COVID-19 (imported [5] vs. local [9]). Twenty-three individuals were admitted during Mar. 19–29 of whom 15 were confirmed COVID-19 (imported (n = 1) vs. local [n = 14]). Excludes population not resident in Metro Manila (n = 21) or admitted before March 8 (n = 34). Dots overlap in the case of identical or similar residence and hence a separate dot is not visible for every case
Table 1 shows the demographic and baseline characteristics of the 100 individuals with suspected COVID-19. Most were aged over 18 (98%) and Filipino (83%). Other nationalities included Chinese (14), American (2), and German (1). Just over half were male (58%), 11% were healthcare workers and recent travel history outside of the Philippines was reported in 47% of suspected cases. Around one-third of suspected cases reported at least one underlying disease (31%), including hypertension (23%), diabetes (9%), cardiovascular disease (7%), respiratory disease (10%), and HIV (1%). One patient reported being pregnant.
Cough was the predominant symptom reported (70%), followed by coryza and fever in around 40%, then sore throat and difficulty of breathing in around 20% of individuals with suspected COVID-19. A small number (6%) had other symptoms which included back pain (2%), diarrhea (2%), and body malaise (2%). The median time from onset of symptoms to hospital admission was 4 days (0, 29).
All confirmed COVID-19 cases were adults. Confirmed cases were older (Fishers test p = 0.003); 40% of confirmed cases were aged 60 years or older and a third were 41-59 years of age. Country of travel history was associated with confirmed COVID-19 (p ≤ 0.001) and increased likelihood of COVID-19 among the Filipino population than other nationalities in this sample (p = 0.024). Confirmed COVID-19 was more common among suspected cases with at least one underlying disease (p = 0.004), in particular, diabetes (p = 0.033) and those who presented with difficulty breathing (p = 0.033). Confirmed cases had experienced symptoms for longer (median of 7 days vs 3 days, p < 0.001). Among the 42 COVID-19 laboratory-confirmed cases, 9 (21%) died (data not shown). Among the 9 patients who died, the median duration of hospitalization was 5 days (0, 8) and the median duration between onset of symptoms and outcome was 11.5 days (8, 18). The sample size did not allow a detailed analysis of factors associated with an outcome of discharged or died. Among the 58 non-COVID-19 cases, 91% of the alternative diagnoses were respiratory (upper respiratory tract infection [39], community-acquired pneumonia [13], chronic bronchitis [1]). Other diagnoses included cardiac (2), viral unspecified (1), gingivitis (1), and not-specified (1).
Discussion
In this study, we report the first 100 individuals with suspected COVID-19 admitted to an infectious disease hospital in Metro Manila from Jan. 25 to Mar. 29, 2020. For comparison, there were 2084 confirmed cases reported nationally in the Philippines as of Mar. 31, 2020 [19]. Some temporal and geographic trends can be observed, with regards to suspected and confirmed infections at SLH. The first two suspected COVID-19 cases admitted to SLH on Jan. 25, 2020, were Chinese nationals on vacation from Wuhan, becoming the first confirmed COVID-19 cases in the Philippines [6]. The Philippine government implemented travel restrictions on foreign travelers from Hubei province on Jan. 31, and then extended this to include additional countries with COVID-19 cases during February [7, 8]. The DOH conducted contact tracing on all the confirmed cases and released an interim guideline for contact tracing for confirmed COVID-19 cases on February 5, 2020 [20]. The absence of further confirmed cases among foreign nationals suggests that these measures were effective. The third confirmed case was admitted on Mar. 8, more than a month after the first case. No epidemiological link was found between the third case and the first two cases. The third, fourth, and fifth cases all reported a history of international travel. The case admitted on Mar. 10 was the first case suggestive of local transmission. On Mar. 12, the Philippine government expanded the travel ban to visitors from all 65 estimated countries with local transmission [9]. Trends toward confirmed COVID-19 cases not reporting international travel (Fig. 1) and being admitted from the populous area of Manila city rather than other areas (Fig. 2) were observed during Mar. 8-29. While only from one hospital, this data suggests the COVID-19 epidemic may have reached Manila city during this time period, as it is likely that symptomatic individuals would have attended SLH rather than another hospital. Increased COVID-19 infections in Manila city are of concern; given it is the most densely populated city in Metro Manila, with 71,263 persons per square kilometer [21]. Small dwelling sizes, social mixing due to extended families, overcrowding in slums, poses a high risk of community transmission and large outbreak in the absence of public health interventions. In order to suppress and mitigate transmission in the Philippines, the government has implemented contract tracing and surveillance, triage systems, increased testing, and improved case management. Enhanced community quarantine has been in place in Luzon island since Mar. 17, 2020 [19]. The effect of these interventions on community transmission and number of severe COVID-19 cases in the context of relatively young population in a tropical climate needs to be carefully assessed.
The factors we report to be associated with COVID-19 confirmed cases among suspected cases should be interpreted with caution. Our finding that COVID-19 confirmed cases tended to be older, Filipino, and less likely have had recent international travel history could be explained by an over-representative number of younger cases with milder symptoms in our sample, reflecting the evolving suspected case definition and referral guidelines.
In over 90% of non-COVID-19 cases, the alternative diagnosis was respiratory, highlighting the difficultly in diagnosing COVID-19 on clinical grounds and the importance of diagnostic capacity in all settings. Difficulty of breathing was the only reported symptom associated with COVID-19 infection. The presence of this symptom should alert healthcare workers to the possibility of COVID-19 infection in this setting. COVID-19 cases were more likely to have an underlying disease, in particular diabetes and hypertension. However, for the aforementioned reasons, these findings should be interpreted with caution.
Among the first 100 cases, seven health care workers were admitted, three of whom were COVID-19 confirmed. This highlights the importance of protecting HCWs during the COVID-19 pandemic. This highlights the importance of protecting HCWs during the COVID-19 pandemic. As of Apr. 6, it has been reported that 299 HCWs have tested positive and 10 have died in the Philippines [22]. During the same time period, there were reports of HCWs hit hard by COVID-19 across several countries [23]. Ensuring adequate supplies of personal protective equipment (PPE), COVID-19 testing and psychological support for HCWs will be important in order to sustain the COVID-19 response in the country. Recently, the Philippine government had secured a US$ 100 million loan from World Bank for COVID-19 Emergency Response including the provision of PPEs [24]. In addition, PPE is being locally manufactured with support from the Philippine Department for Trade and Industry [25].
The clinical characteristics of the confirmed COVID-19 cases in this study are comparable with the early case series from China and reports from other countries [4, 5, 24]. Cough and fever were the most common symptoms, similar to results reported in China, Italy, and the USA. Shortness of breath and muscle aches were less frequently reported in our study but may not have been systematically recorded on the CIF [3, 26, 27].
Among the 9 patients who died, most deaths occurred within a week of admission and within 18 days of symptom onset (median 11.5 days). A range of about 2-8 weeks from time of symptom onset to death was reported in China early in the outbreak [28]. Recent studies also report a similar range of hospitalization among the non-survivors, with the majority requiring ICU care [29, 30]. Larger adequately powered studies to analyze risk factors for mortality in this setting are required. Among admitted COVID-19 cases, the case fatality rate was 21%. This is comparable to other in-patient settings in Wuhan China (CFR—15% and 28%) and New York (CFR—21%) [26, 31, 32]. The CFR is higher than the overall mortality rate in the Philippines, reported to be 6.6% [33]. However, this cannot be compared as hospitalized cases are likely to be more severe than cases in the general population. In this study, almost half of confirmed admitted cases were older, had at least one co-morbidity, most commonly hypertension (33%), diabetes (17%), or respiratory illness (17%). Older age and hypertension were reported to be key risk factors for COVID-19 mortality in Italy [34].
This study has some limitations. First, this is a modest case series of 100 patients with suspected COVID-19 infection, of whom only 42 patients had confirmed COVID-19 infection. The study was underpowered to detect associations with mortality. Second, the findings from this study cannot be generalized to other populations in the Philippines or elsewhere given the small sample size and evolving suspected COVID-19 criteria and heterogeneous study population. Third, this analysis was limited to data collected on the CIFs and did not include detailed travel, referral or contact history, or information on investigations and treatments received. Our assumption that cases reporting recent international travel were imported may not be true and could be coincidental in some cases.
While this study provides some insights, a larger study would help further define the epidemiology and clinical features of COVID-19 in this setting. We would caution against any change in patient management based on this study. However, the data we present allows an early assessment of epidemiological and clinical characteristics of COVID-19 in Metro Manila, Philippines, and a hospital in a tropical LMIC country.
Conclusion
As of May 2, there have been 3,267,184 cases confirmed cases globally, and 8772 confirmed cases in the Philippines [10, 35] indicating sustained community transmission. We report an increasing trend of confirmed COVID-19 cases being admitted to SLH from the densely populated Manila city area and a hospital case fatality rate of 21%.
Availability of data and materials
The dataset for this study is available from the corresponding author and San Lazaro Hospital on a reasonable request. Data without names and identifiers will be made available after approval from the corresponding author and San Lazaro Hospital.
Change history
22 October 2021
A Correction to this paper has been published: https://doi.org/10.1186/s41182-021-00373-5
07 July 2020
A Correction to this paper has been published: https://doi.org/10.1186/s41182-020-00244-5
Abbreviations
- CFR:
-
Case fatality rate
- CIF:
-
Case investigation forms
- COVID-19:
-
Coronavirus disease 2019
- DOH:
-
Department of Health
- HCW:
-
Healthcare worker
- LMIC:
-
Low and middle income
- NPS/OPS:
-
Nasopharyngeal and oropharyngeal swabs
- PCR:
-
Polymerase chain reaction
- PPE:
-
Personal protective equipment
- PUI:
-
Person under investigation
- RESU:
-
Regional Epidemiologic Surveillance Unit
- RITM:
-
Research Institute for Tropical Medicine
- SARI:
-
Severe acute respiratory illness
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
- SD:
-
Standard deviation
- SLH:
-
San Lazaro Hospital
References
Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–33.
Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. 2020;(2531-6745).
Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507.
Young BE, Ong SWX, Kalimuddin S, et al. Epidemiologic features and clinical course of patients infected with SARS-CoV-2 in Singapore. JAMA. 2020;323(15):1488–94.
Arentz M, Yim E, Klaff L, et al. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington state. JAMA. 2020;323(16):1612–4.
Edrada EM, Lopez EB, Villarama JB, et al. First COVID-19 infections in the Philippines: a case report. Tropical Medicine and Health. 2020;48:21.
CNN Philippines. Duterte widens travel ban on mainland China, Hong Kong, Macau. 2020. https://cnnphilippines.com/news/2020/2/2/Duterte-travel-ban-mainland-China-Hong-Kong-Macau.html. Accessed 30 Mar 2020.
Government of Philippines. Interagency Task Force for the Management of Emerging Infectious Diseases Resolution No. 4. https://www.doh.gov.ph/COVID-19/IATF-Resolutions. Accessed 30 Apr 2020.
CNN Philippines. Philippines expands travel ban to all countries with local COVID-19 transmission. 2020. https://www.cnnphilippines.com/news/2020/3/12/Philippines-expands-travel-ban-to-all-countries-with-local-COVID-19-transmission.html. Accessed 30 Apr 2020.
Department of Health. DOH confirms local transmission of COVID-19 in Philippines; reports 6TH case March 7, 2020. https://www.doh.gov.ph/doh-press-release/doh-confirms-local-transmission-of-covid-19-in-ph. Accessed 1 May 2020.
Department of Health. COVID-19 tracker. https://www.doh.gov.ph/covid19tracker. Accessed 27 Apr 2020.
Department of Health.Public Advisory No. 13 - Updated guidelines for management and referral of suspected and confirmed COVID-19 cases under code red (as of March 07,2020). https://www.doh.gov.ph/sites/default/files/health-update/dc2020-0107.pdf. Accessed 29 May 2020.
Department of Health. Interim guidelines on the preparedness_and response to novel coronavirus (2019-nCoV) from Wuhan, China (as of Jan 21, 2020). https://www.doh.gov.ph/sites/default/files/health-update/DM-2020-0034-Interim-Guidelines-on-the-Preparedness-and-Response-to-2019-nCoV_0.pdf. Accessed 30 Apr 2020.
Department of Health. Advisory no. 2: decision tool for 2019-novel coronavirus acute respiratory disease (2019-nCoV ARD) https://www.doh.gov.ph/node/19291. Accessed 30 Apr 2020.
Department of Health. UPDATED DECISION TOOL FOR COVID-19. https://www.doh.gov.ph/node/20330. Accessed 29 Apr 2020.
Peter Doherty Institute for Infection and Immunity. Victorian infectious disease reference laboratory (VIDRL). https://www.vidrl.org.au/. Accessed 7 Feb 2020.
Republic of the Philippines Department of Health. Research Institute for Tropical Medicine http://ritm.gov.ph/. Accessed 25 Apr 2020.
StataCorp. Stata statistical software: release 15. College Station: StataCorp LLC.; 2017.
Department of Health. “Interim guidelines on contact tracing for confirmed 2019 novel coronavirus acute respiratory disease (2019-nCoV ARD) cases”. 2020. Retrieved May 28, 2020, from https://www.doh.gov.ph/sites/default/files/health-update/DC2020-0048-Reiteration-of-DM2020-0068-Interim-Guidelines-on-Contact-Tracing-for-Confirmed-2019-nCoV-ARD-Cases.pdf.
REPUBLIC OF THE PHILIPPINES PSA. Philippine Population Density (Based on the 2015 Census of Population). https://psa.gov.ph/content/philippine-population-density-based-2015-census-population. Accessed 30 Apr 2020.
Interagency Task Force for the Management of Emerging Infectious Diseases Resolution No. 12 recommendation for the management of the corona virus disease 2019 (COVID-19) situation. https://www.doh.gov.ph/COVID-19/IATF-Resolutions. Accessed 31 Mar 2020.
World Health Organization. Coronavirus disease (COVID-19) Situation Report 15 Philippines 6 April 2020. https://www.who.int/docs/default-source/wpro%2D%2D-documents/countries/philippines/emergencies/covid-19/. Accessed 30 Apr 2020.
The Lancet. COVID-19: protecting health-care workers. Lancet. 2020;395(10228):922.
The World Bank. Philippines: World Bank approves US$100 M to support COVID-19 emergency response. April 22, 2020. https://www.worldbank.org/en/news/press-release/2020/04/23/philippines-world-bank-approves-usd100m-to-support-covid-19-emergency-response. Accessed 1 May 2020.
Department of Health. DOH: local companies to produce 10,000 personal protective equipment daily with support from DTI. https://www.doh.gov.ph/doh-press-release/DOH-LOCAL-COMPANIES-TO-PRODUCE-10000-PERSONAL-PROTECTIVE-EQUIPMENT-DAILY-WITH-SUPPORT-FROM-DTI. Accessed 4 Apr 2020.
Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA. 2020:e206775.
Colaneri M, Sacchi P, Zuccaro V, et al. Clinical characteristics of coronavirus disease (COVID-19) early findings from a teaching hospital in Pavia, North Italy, 21 to 28 February 2020. Euro Surveill. 2020;25(16).
Baud D, Qi X, Nielsen-Saines K, Musso D, Pomar L, Favre G. Real estimates of mortality following COVID-19 infection. Lancet Infect Dis. Published March 12, 2020.
Heath Information and Quality Authority. Evidence summary for average length of stay in intensive care unit for COVID-19 1 April 2020. https://www.hiqa.ie/reports-and-publications/health-technology-assessment. Accessed 20 May 2020.
Intensive care national audit and research center. ICNARC report on COVID-19 in critical care April 04, 2020. https://www.icnarc.org/About/Latest-News/2020/04/04/Report-On-2249-Patients-Critically-Ill-With-Covid-19. Accessed 30 Apr 2020.
Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet. 2020. https://doi.org/10.1016/S0140-6736(20)30183-5.
Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–62.
John Hopkins Corona virus Resource center. Mortality analyses. 2020. coronavirus.jhu.edu/data/mortality. Accessed 30 Apr 2020.
Zangrillo A, Beretta L, Scandroglio AM, et al. Characteristics, treatment, outcomes and cause of death of invasively ventilated patients with COVID-19 ARDS in Milan, Italy. Crit Care Resusc 2020.
World Health Organization. Coronavirus disease (COVID-19 Situation Report– 103. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports. Accessed 2 May 2020.
Acknowledgements
We thank the San Lazaro Hospital Epidemiology Department encoders and fellows.
We thank Chris Fook Ng and Saho Takaya for commenting on previous drafts.
Funding
This work is in part funded by Nagasaki University (salary support for CS, SJS, AV, XS, TE, SMH, KA). The funder of the study had no role in the study design, data collection, data analysis, data interpretation, or the writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Author information
Authors and Affiliations
Contributions
Eumelia P. Salva: data interpretation, writing. Jose Villarama: data interpretation. Edmundo B. Lopez: data interpretation. Ana Ria Sayo: data interpretation, writing. Annavi Marie G Villanueva: study design, data interpretation, writing. Tansy Edwards: data analysis, writing. Su Myat Han: literature search, writing. Shuichi Suzuki: data interpretation. Xerxes Seposo: figures. Koya Ariyoshi: study design, data interpretation. Chris Smith: study design, data interpretation, writing. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This was a retrospective analysis of anonymized routinely collected data, implemented under an existing acute respiratory tract/COVID-19 study, approved by the SLH research ethics and review unit (Ref: SLH-RERU-2020-022-I) and the School of Tropical Medicine and Global Health, Nagasaki University Ethical Committee (NU_TMGH_2020_119_1).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: “The Figure 1 is revised”.
The original version of this article was revised: a sentence has been added in the second paragraph of the Study design and participants section.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Salva, E.P., Villarama, J.B., Lopez, E.B. et al. Epidemiological and clinical characteristics of patients with suspected COVID-19 admitted in Metro Manila, Philippines. Trop Med Health 48, 51 (2020). https://doi.org/10.1186/s41182-020-00241-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41182-020-00241-8