Abstract
Background
Enteral nutritional therapy (ENT) has the principle of maintaining or recovering the nutritional status of individuals who cannot or unable to feed them the oral diet. The aim of this study was to verify the clinical and nutritional outcome of patients on ENT during the period of 1 year.
Methods
It is a quantitative, descriptive, retrospective, and documentary research, through the analysis of medical records of all individuals who used ENT for 1 year in a public hospital of Bauru, SP, with evaluation of weight loss, time of ENT’s use, and outcomes such as death and weaning. The collection took place in the adult hospital unit containing 165 hospital beds, including 33 beds of the intensive care unit (ICU), and 132 beds divided into nine clinics (surgical and medical), with reference mainly to trauma, neurosurgery, and neurology. All patients admitted to these wards using ENT were collected.
Results
A total of 527 patients were included, and it was observed that the majority of ENT’s indications came from neurological diseases (42.2%), with the onset of the ENT in the intensive care unit with 69.0% due to needs for mechanical ventilation. The mean number of ENT days was 20.4 days. There was a positive correlation between the percentage of weight loss and time of ENT’s use (p < .0001). There was worst outcome and lower weaning rate in the elderly.
Conclusions
It has been shown that the longer the time of ENT’s use, the greater the percentage of weight loss of these individuals; malnourished patients present longer time using the therapy, and the elderly presented higher mortality rate.
Similar content being viewed by others
Background
There are several clinical situations related to nutritional status, one of them is malnutrition, and it is classified as “a morbid state secondary to a deficiency or relative/excess of one or more essential nutrients, clinically manifested, or detected through biochemical, anthropometric, topographical, or physiological tests” [1].
The occurrence of malnutrition in hospitalized individuals is a public health problem that has been widely described [2,3,4,5]. According to Naberet al. [3], the prevalence of malnutrition may vary between 20 and 50% of hospitalized individuals depending on the nutritional screening method used. It is associated with a significant increase in morbidity and mortality, time, and cost of hospitalization. A long period, or even a short period without adequate food intake, may cause damage to organic functions [2].
In hospitalized individuals, malnutrition is a result of a number of factors and may be associated with disease and/or treatment [5]. Inadequate food consumption is one of the main causes and is related to several clinical situations that may lead of losing appetite or impeding food intake, as well as investigation and treatment procedures that require the fasting and/or changes in diet composition. Delay in nutritional screening and inadequate intervention may also result in the worsening of nutritional status during hospitalization [5].
In case of inability of food intake orally, or if intake is not sufficient to supply energy and protein intake, the enteral nutritional therapy (ENT) is the first choice [6]. ENT is a set of therapeutic procedures, used for the maintenance or recovery of nutritional status, to supply nutrients through the digestive tract when it is functioning by gastric or enteral probes. Among its advantages, the following can be highlighted: prevention of intestinal mucosal atrophy, protection against bacterial translocation (displacement of bacteria from the lumen of the gastrointestinal tract to sterile sites), and reduction of inflammatory response, improving the immune response, reducing the incidence of complications, and providing exogenous energy substrates in order to overcome intense catabolism and repair injuries [4].
Despite the benefits of ENT, there might be some complications during its use such as malposition and obstruction of the probe, contamination during handling/installation of ENT inadequate dietary administration, or formula intolerance [7]. There is also a risk of hypoalimentation, leading to increased hospitalization, respiratory compromise with increased mechanical ventilation, delay in healing of lesions, and loss of intestinal integrity and immune response leading to weight gain and hospitalization costs. On the other hand, it can offer an excess of calories, especially when the person is fasting. It may lead to Refeeding Syndrome, causing metabolic complications, electrolyte imbalance, respiratory compromise, hepatic dysfunction, increased morbidity and mortality, physiological stress, abnormal glucose metabolism, and increased carbon dioxide production [8].
Nasoenteric tubes (nasogastric, nasoduodenal, and nasojejunal) are usually reserved for short-term (less than 30 days) enteral feeding [9]. For medium- and long-term enteral feeding, gastric feeding is the most common type of enteral feeding. Due to low cost, less invasive, and no need for general anesthesia in most cases, percutaneous endoscopic gastrostomy (PEG) is considered to be a better choice than surgical methods [10].
This study investigates the characteristics of individuals using this alternative feeding method and the main reasons for ENT administration, as well as the outcomes of individuals hospitalized in a public hospital. The aim of this study was to verify the clinical and nutritional outcome of patients on ENT during the period of 1 year.
Methods
This is a quantitative, descriptive, retrospective, and documentary study that aims to verify the clinical and nutritional outcome of patients on ENT during the period of 1 year.
The study was approved by the Ethics and Research Commission of the Sacred Heart University under number of opinions 2.031.670, approved also by the Nucleus of Research and Teaching of the hospital unit. No informed consent form was signed, since the data collected were already performed as routine in the sector.
The analyzed public hospital is located in the center-west of the state of São Paulo in Brazil. The adult hospital unit has 165 hospital beds, including 33 beds of the intensive care unit (ICU), and 132 beds divided into nine clinics (surgical and medical), with reference mainly to trauma, neurosurgery, and neurology. There are around 750 to 800 hospitalizations per month.
In total, 574 individuals which started ENT in this period were included and retrospectively registered. However, some individuals had to be excluded: 6 individuals because they were under 18 years old, 38 individuals because on the last day of collection they were still using ENT and an outcome could not be analyzed, and 3 individuals who did not have a nutritional evaluation. Then, 527 medical records were considered.
To obtain the data of the research, we analyzed data collected monthly by the clinical nutrition team. Information from individuals who used ENT from May 2016 to April 2017 was obtained, such as age, sex, initiation of therapy, medical specialty, reason for initiation of ENT, initial nutritional status, final nutritional status, percentage of weight loss, duration of ENT’s use, and outcome of the subjects. The main outcomes evaluated were ENT weaning and mortality.
The nutritional status was classified according to the body mass index (BMI) for age group, classifying nutritional status of adults (< 60 years) according to WHO, 1997 [11], and nutritional status of the elderly (> 60 years) according to Lipschitz, 1994 [12].
For the analysis of weight, the following was considered: the weight of the first evaluation prior to starting ENT and the weight when the therapy was over. For adults and the elderly, they were classified into three groups: low weight, eutrophic, and overweight. The percentage of weight loss was performed according to Blackburn (1977) [13].
The normality of the data was analyzed using the Shapiro Wilk test. For comparison between two groups, the Student’s t test was used when the continuous variables presented normal distribution and the Mann-Whitney test when they had a non-normal distribution. For comparison between groups of categorical variables, the chi-square test or Fisher’s exact test was used. Correlations between continuous variables were performed using the Pearson correlation or Spearman correlation if the variables presented normal or non-normal distribution, respectively.
Data analyses were performed using the SAS System software. The level of significance was 5%.
Results
The study included 527 medical records of individuals aged between 18 and 97 years old, with a mean age of 64.5 ± 20.1 years. 65.6% were elderly (≥ 60 years old) and predominantly male (57%). In cases of re-hospitalization and the need for ENT within the analyzed period, the medical record was included again as a new individual.
When analyzing the hospitalization profile, 42.2% were admitted to neurological specialties (neurosurgery/neurology), with diseases such as ischemic and hemorrhagic brain vascular accident, cranial trauma, subdural hematoma, among others; with relevant hospitalizations for specialty of the medical clinic (29.84%); and followed by cardiology/cardio surgery (8%), orthopedics (5.3%), general surgery (3.6%), nephrology (3.4%), head and neck surgery (3%), and other specialties (4.8%).
The main sector with the need of stating ENT was the intensive care unit (ICU, 69.01%), followed by the medical clinic (23.18%), the surgery clinics (5.13%), and the neurological sectors (2.66%).
The high number of ENT in the ICU was due to tracheal intubation or tracheostomy associated with mechanical ventilation. This was the main reason for initiating ENT(52.9%). Another relevant cause of initiating of ENTwas due to neurological changes (lowering of consciousness level/drowsiness) due to the complications/consequences of the hospitalization pathologies (14.1%). The decrease in general state/lowering of the level of consciousness not associated with neurological pathologies add up to 11.4% of the reasons for initiating ENT, followed by insufficient oral intake (4.18%), motor swallowing (3.6%), oral ingestion by non-functioning upper gastrointestinal tract (1%), and severe cachexia/malnutrition (0.6%).
The mean number of days of use of ENT in the 527 medical records analyzed was 20.4 days, with a minimum of 1 day and a maximum of 242 days of the therapy.
Correlations among weight loss percentage and initial/final BMI with the time of ENT’s use can be observed in Table 1. There was a positive correlation between weight loss percentage and the time of ENT’s use (p < .0001). In relation to the BMI measured at the beginning of the therapy, no statistical difference was observed associated with the time of ENT’s use. However, when evaluating at the final moment, a negative association with the time of ENT’s use (p = 0.0002) was observed, demonstrating that the lower the BMI during the use of ENT, the longer these individuals remained with this route of feeding.
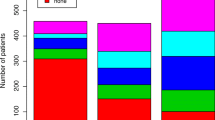
Regarding the outcome of these individuals, some of the individuals were weaned from ENT, with hospital discharge receiving a via oral exclusive diet (29.3%); 17.9% of individuals returned to home dependent on ENT, being advised about the therapy at the time of discharge and referred to outpatient units; 1.1% of individuals had to suspend ENT due to the impossibility of using the gastrointestinal tract (GIT), initiating exclusive parenteral nutrition; 1.3% of individuals were transferred to other hospitals/counties, however, a large number of individuals who used ENT died (50.2%).
When analyzing weaning of ENT with the time of ENT’s use, no statistical difference was observed among variables (p = 0.61). However, individuals who died were the ones with the lowest time of ENT’s use (p = 0.007) (Table 2).
Evaluating the outcomes and the age groups, it can be observed that adults had a higher weaning rate than the elderly (p < .0001). In relation to death, a higher rate was observed among the elderly (p < .0001), as shown in Table 3.
Tables 4 and 5 show the classification of ENT weaning and death outcomes according to BMI at the initial and final moments. It was observed that the group that presented ENT weaning had a higher BMI (p = 0.006) at the initial moment, however with no statistical difference at the final moment. Regarding death, no statistical difference was observed in the BMI at both moments.
Discussion
The need to indicate the beginning of ENT is related to the individual’s clinical conditions because they cannot or want to receive oral feeding and medications [14, 15]. Improperly supplied nutritional support results in loss of weight and general worsening of nutritional status, increasing the risk of mortality and morbidity, hospitalization time, and thus increasing health costs. There are several causes that can lead to hospital malnutrition, such as the disease itself, prolonged or unnecessary fasting prescription, and even the triviality of malnutrition in the clinical routine [15, 16].
Regarding the age of the individuals studied, Carvalho et al. [7] evaluated 65 individuals from a university’s hospital who benefited from ENT during hospitalization, observing a mean age of ± 48 years. Santos [17] found among the group studied the mean age of 69 years ± 17.5 years, from a philanthropic hospital analyzing 688 individuals during 4 years. Pérez [18] analyzed 160 individuals in ENT for 6 months, observing the mean age of 60 years. The variation of the mean age is due to the type of hospital analyzed, as well as predominant diseases at least. The mean age of hospitalized individuals analyzed in this study is close to the literature, 64.5 years ± 20.13 years.
The population of hospitalized individuals (229 individuals) studied by Nogueira [19] was a large part of the elderly, with 64.5% of the total, corroborating the results obtained in 65.6% of elderly individuals. Older people have more fragile health in relation to chronic degenerative diseases (cardiovascular, oncology, mental alterations, pathologies that affect the motor system and senses), increasing the frequency of disease affection and sequels, and consequently needing to use more the health services [6].In addition, the aging of our population makes health professionals maintain more intense and specific care, especially when it comes to hospitalization, which can lead to fragility syndrome, sarcopenia, and other complications that increase with age.
In the study by Nozaki [8], after analysis and comparison between two hospital units, it was observed that in both hospitals, the majority of the study population was male, 71.4% and 66.7%, respectively. Similar to the result obtained in this study (57%), Nogueira [18], analyzing 229 individuals, also observed a greater percentage of men (55.0%) in ENT use. In contradiction to these data, we found other studies with a higher percentage of women using ENT, again emphasizing the variation due to the specialty and type of hospital [7, 20].
It was analyzed, in our study, that the sector with the highest frequency of onset of ENT was the ICU (69.0%). A survey of 361 individuals in ENT also observed a greater number of catheter passages for naso-enteral feeding in intensive care units (85.0%), sequenced by the wards [20]. Another study that analyzed two different hospitals found that in the hospital, 1.80% of the individuals using this therapy were hospitalized in the ICU, and in hospital 2, this number was 77.8% [8]. Critical individuals evolve with a complex and variable high metabolic rate, consequently decreasing muscle supply, wound healing, and cognitive impairment, and it is like benefiting the early diet to alter the physiological response to this stress, justifying the high onset of ENT in intensive care [21]. Most of the indications pointed out in our study are related to the need for mechanical ventilation, but with a functioning GIT, which leads to alternative feeding. ENT weaning is performed after weaning from mechanical ventilation, at a safe moment, often being hampered by weakened neurological status. Neurological-based pathology is also one of the causes for the need for ENT, due to the risks of dysphagia, low food intake, neurological confusion, and lowering of the level of consciousness, which may lead to malnutrition/weight loss due to inadequate consumption.
Even though neurological individuals are the largest percentage requiring ENT (42.2%), the specific ward was the one with the lowest percentage, since most individuals start nutritional therapy in the ICU, due to the severity of the disease at hospital admission.
In relation to the great part of the onset of ENT occurring in the ICU in our study, the major reason for naso-enteric catheterization was through oro-tracheal intubation or tracheostomy in the use of mechanical ventilation, followed by lowering the level of consciousness in neurological individuals and lowering the level of consciousness in other pathologies (adding 25.5%). Other authors have also observed indications for ENT due to sensory lowering in individuals in their analyzes [15, 19]. In the study by Doundoulakiset al. [16], which followed 150 insertion catheter insertion procedures in emergency units, it was observed that 40.0% of the individuals started ENT by lowering the level of consciousness, different from what this research shows, in which 14.7% were due to invasive or non-invasive mechanical ventilation. Another author also observed that lowering the level of consciousness was the most usual justification for the use of ENT [19].
The mean time of ENT’s use was 20.4 days, with a maximum of 242 days. Santos et al. [17] observed a shorter time of ENT’s use in their study group with an average of 11 days in relation to this analysis and a maximum of 96 days. Sicchieri [22] had a longer mean time of ENT’s use with 23.5 days, being very close to the study, but with a shorter maximum time (125 days). We observed time close to Cervo’s study [23], with an average time of 18.5 days, but the maximum time of use of the much lower comparative study (maximum of 30 days). In spite of the time of ENT’s use close when compared to the last two studies, when analyzing the maximum time of ENT’s use, there is a big difference for the hospital studied, which can be explained by the high number of hospitalizations of the elderly (65.6%). It might require greater care in relation to the nutritional supply, due to the greater frequency of hospitalization and longer hospitalization, which may require ENT for a longer time than an adult (up to 59 years) [24]. The data of this current study is related to the profile of the analyzed hospital, with many inpatients for neurological complications and trauma, which can extend the treatment, increasing this time, and also explaining the maximum number of days of use (242 days), compared to the shorter time in other hospitals.
There was no difference between the initial nutritional status (BMI) and the time of ENT’s use, but the results showed that the greater weight loss during ENT, the longer the use of therapy and that the worse nutritional status along the use of therapy, the longer the use of ENT. Santos et al. [17] observed that there was no difference between the time of nutritional therapy when related to the energy supply. There is a high prevalence of hospital malnutrition in the elderly, and it may reach up to 52% [25]. One study verified the evolution of the elderly during hospitalization and observed weight loss in 30.6%, with a loss greater than 2 kg during the treatment period [26]. Duarte et al. [27] observed in their study, with adults and the elderly, significant weight loss during the period of hospitalization longer than 15 days. The prolonged hospitalization time associated with other factors, not only the use of ENT, resulted in weight loss, especially in the elderly.
It is important to point out that there was a bias in the data analyzed, since only the profile of the patients in relation to the use of ENT and the time of therapy were observed. Also, because it was a documentary work, they were not accompanied by caloric and protein supply prescribed and infused to verify if the weight loss of these individuals was associated with underlying disease and hospitalization complications.
Regarding death, it was observed that individuals who used ENT for a shorter time had a higher death rate. This can be explained by the fact that the majority of individuals with ENT are in the ICU, due to the severity of the clinical picture, and there may be a higher mortality rate than individuals hospitalized in the sectors with a shorter hospital stay [28].
The high death rate (50.2%) that was found was evidenced by other authors, but there was no relation to the nutritional status [8, 29]. Santos et al. [17], analyzing 688 individuals for 4 years, did not obtain results of malnutrition directly related to death. The sequel generated by diseases in the elderly, as mentioned, led to a lower weaning rate in this age group when compared to adults. This fragility of the age group explains the highest death rate evaluated in this study for the elderly when compared to adults, and this result is confirmed in the literature [17, 28, 30].
In the literature, the weaning rate of ENT for oral nutritional therapy does not have single data, showing weaning from 45.7 to 13.9% [8, 31]. This study showed a return to the oral use of 29.3%, a value close to other studies. It is worth mentioning that there is a speech-language pathology team working in the studied hospital, helping to withdraw ENT to the oral route, minimizing the risks of complications and rehabilitation of swallowing disorders [19].
It is observed that has been much researched in recent years on the malnutrition of the hospitalized individuals; however, there has not been a reduction in the number of malnourished patients over the years. Studies indicate improvements with adequate nutritional support in improving healing, less catabolism in lesion responses, reduction of hospitalization time and intra-hospital complications, and integrity of the gastrointestinal tract [32]. Comparing Tables 4 and 5, we can observe that the patients who presented ENT weaning were the ones that had the highest initial BMI, however with no difference for the final BMI, demonstrating that a higher nutritional status at the beginning of the use of an enteral catheter seems favor weaning. Regarding death, we did not observe a significant response regarding BMI, which may be associated with the hospitalization profile of the hospital, with reference to trauma, admitting polytraumatized patients, often with associated head injury, increasing the catabolic rate, and accelerating mass loss muscle, thus altering the weight of this individual.
This study has raised the main findings about hospitalized patients using ENT, so that we seek strategies to reduce the time of ENTs, consequently improving survival and quality of life, as well as reducing hospitalization costs and related risks such as infections.
Conclusion
It can be observed mainly that the greater time of ENT’s use, the greater percentage of weight loss of these individuals, and malnourished patients presented a longer time of use of this nutritional therapy. There was no difference in relation to the death rate compared to nutritional status, showing that all individuals should receive the same importance for ENT. There is still a need for more studies regarding the time of ENT’s use and its consequences, so that there is an adequate and more effective intervention, reducing hospitalization time and hospital costs.
Abbreviations
- BMI:
-
Body mass index
- ENT:
-
Enteral nutritional therapy
- ICU:
-
Intensive care unit
References
Silva SRJ, Waitzberg DL. Gastoenergético. In: Waitzberg DL, editor. Nutrição oral, enteral e parenteral napráticaclínica. 3ª ed. São Paulo: Atheneu; 2002. p. 327–42.
Souza MD, Nakasato M. A gastronomia hospitalar auxiliando na redução dos índices de desnutrição entre pacientes hospitalizados. O Mundo da Saúde, São Paulo. 2011;35(2):208–14.
Naber TH, Schermer T, de Bree A, Nusteling K, Eggink L, Kruimel JW, et al. Prevalence of malnutrition in nonsurgical hospitalized patients and its association with disease complications. Am J ClinNutr. 1997;66(5):1232–9.
Couto LFC. Nutrição Enteral no PacienteCrítico: Via de Administração, Avaliação do GastoEnergético e Impacto da AdequaçãoNutricionalsobreDesfechosemCurto e Longo Prazo. Tese (Pós-graduaçãoemCiênciasPneumológicas) – Faculdade de Medicina, Universidade Federal do Rio Grande de Sul, Porto Alegre, 2016, 14–74.
Aquino CR, Philippi TS. Identificação de Fatores de Risco de DesnutriçãoemPacientesInternados. Rev Assoc Bras. 2011;57(6):637–43.
Barndregt K, Soeters P. Suportenutricional. In: Gibney MJ, et al., editors. Nutriçãoclínica. Tradução Maria Angelica Borges dos Santos; PatriciaLydieVoeux. Rio de Janeiro: Guanabara Koogan; 2007. p. 106–21.
Carvalho AMR, Oliveira DC, Neto JEH, Martins BCC, Vieira VMSF, Silva LIMM, Ponciano AMS, Fonteles MMF. Análise da prescrição de pacientes utilizando sonda enteral em um hospital universitário do Ceará. R Bras Farm Hosp Serv Saúde, São Paulo. 2010;1:1–24.
Nozaki VT, Peralta RM. Adequação do suporte nutricional na terapia nutricional enteral: comparação em dois hospitais. Rev Nutr Campinas. 2009;22(3):341–50.
Rahnemai-Azar AA, Rahnemaiazar AA, Naghshizadian R, Kurtz A, Farkas DT. Percutaneous endoscopic gastrostomy: indications, technique, complications and management. World J Gastroenterol. 2014;20(24):7739–51.
Grant JP. Comparison of percutaneous endoscopic gastrostomy with Stamm gastrostomy. Ann Surg. 1988;207:598–603.
Wold Health Organization. Obesity: preventing and managingthe global epidemic. Geneva: WHO; 1997.
Lipschitz DA. Screening for nutritional status in the elderly. PrimCare. 1994;21(1):55–67.
Blackburn GL, Bistrian BR, Maini BS. Nutritional and metabolic assessment to the hospitalized patient. JPEN. 1977;1:11–32.
Waitazberg DL. Nutrição Oral, Enteral e Parenteral na Prática Clínica. 4th ed. EditoraAtheneu: São Paulo; 2009.
Anziliero F, Corrêa APA, Silva BA, Soler BED, Batassini E, Beghetto MG. Sonda Nasoenteral: fatores associados ao delay entre indicação e uso em Emergência. Rev Bras Enferm. 2017;70(2):326–34.
Doundoulakis I, Poulia KA, Antza C, Bouras E, Kasapidou E, Klek S, Chourdakis M. Screening for malnutrition among people accessing health services at Greek public hospitals: results from an observation multicenter study. J Parenter Enteral Nutr. 2018;42(4):709–18. https://doi.org/10.1177/0148607117722748.
Santos CA, Firmino HH, Esmeraldo MLF, Alfenas RCG, Ribeiro AQ, Almeida LF, Amorim GP. Perfil nutricional e fatores associados à desnutrição e ao óbito em pacientes com indicação de terapia nutricional. BRASPEN J. 2017;32(1):30–5.
Pérez OM, Avilés AM, Martínez A, Boix A, Aznar S, Martín MD, Picó AM. Factores prognósticos de morbi-mortalidad em nutrición enteral hospitalaria: studio prospectivo. Nutr Hosp. 2005;20:210–6.
Nogueira SCJ, Carvalho APC, Melo CB, Morais EPG, Chiari BM, Gonçalves MIR. Perfil de pacientes em uso de via alternativa de alimentação internados em um hospital geral. Rev CEFAC. 2013;15(1):94–104.
Graciano RDM, Ferretti REL. Nutrição enteral em idosos na Unidade de Terapia Intensiva: prevalência e fatores associados. Geriatria & Gerontologia. 2008;2(4):151–5.
Patel JJ, Hurt RT, Mcclave SE, Martindale RG. Criticial care Nutricion: where’s the evidence? Crit Care Clin. 2017;33:397–412.
Sicchieri JMF, Unamuno MRDL, Marchini JS, Cunha SFC. Evolução antropométrica e sintomas gastrointestinais em paciente que receberam suplementos nutricionais ou nutrição enteral. Rev Assoc Med Bras. 2009;55(2):149–52.
Cervo AS, Magnago TSBS, Carollo JB, Chagas BP, Oliveira AS, Urbanetto JS. Eventos adversos relacionados ao uso de terapia nutricional enteral. Rev Gaúcha Enferm. 2014;35(2):53–9.
Gaino NM, Leandro-Merhi VA, Oliveira ARM. Idosos hospitalizados: estado nutricional, dieta, doença e tempo de internação. Rev Bras Nutr Clin. 2007;22(4):273–9.
Gomes JR, Santana AFF, Fidelix MSP. Prevalência de desnutrição hospitalar em idosos. RASBRAN. 2013;5(1):60–8.
Dalpiaz JS, Bertoni VM, Alves ALS, Bertol D. Estado nutricional e sua evolução durante a internação hospitalar em pacientes idosos. Rev Bras Nutr Clín. 2015;30(1):34–8.
Duarte A, Marques AR, Sallet LHB, Colpo E. Risco nutricional em pacientes hospitalizados durante o período de internação. Nutr Clín Hosp. 2016;36(3):146–52.
Freitas ERFS. Perfil e gravidade dos pacientes das unidades de terapia intensiva: aplicação prospectiva do escore APACHE II. Rev Latino-Am Enfermagem, 2010. 18(3): [07 telas]. Disponível em http://www.redalyc.org/html/2814/281421933004/. Acesso em 01 de out. 2017.
Maia FOM, Duarte YAO, Lebrão ML, Santos JLF. Fatores de risco para mortalidade em idosos. Rev SaúdePública. 2006;40(6):1049–56.
Teixeira VP, Miranda RC, Baptista DR. Desnutrição na admissão, permanência hospitalar e mortalidade de pacientes internadosem um hospital terciário. Demetra. 2006;11(1):239–51.
Martins AS, Rezende NA, Torres HOG. Sobrevida e complicações em idosos com doenças neurológicas em nutrição enteral. Rev Assoc Med Bras. 2012;58(6):691–7.
Mundi MS, Pattinson A, Mcmahon MT, Davidson J, Hurt RT. Prevalence of home parenteral and enteral nutrition in the United States. Nutr Clin Pract. 2017;32(6):799-805. https://doi.org/10.1177/0884533617718472.
Acknowledgements
English language editing was provided by Dr. Andréa Baraldi Cunha.
Availability of data and materials
The dataset and statistical code are available from the corresponding author: nataliabcunha@gmail.com
Author information
Authors and Affiliations
Contributions
FGGH was responsible for the design, intellectual and scientific content of the study, and acquisition of data and technical procedures. DN, KRP, KVdosF, MDF, TRM, TBTdeB, and VBdeM were responsible for the acquisition of data and technical procedures. SJP was responsible for the scientific content of the study and critical analysis. NBC was responsible for the critical analysis of scientific content of the study, technical procedures, and final approval of manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics and Research Commission of the Sacred Heart University under number of opinions 2.031.670, approved also by the Nucleus of Research and Teaching of the Bauru Base Hospital. No informed consent form was signed, since the data collected were already performed as routine in the sector, collecting data from medical records.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Homelis, F.G.G., Nakayama, D., Perpétuo, K.R. et al. Enteral nutritional therapy of inpatients: clinical and nutritional outcomes. Nutrire 43, 21 (2018). https://doi.org/10.1186/s41110-018-0080-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41110-018-0080-3