Abstract
Background
MLT-550N is a device to measure the body fluid volume based on bioimpedance spectroscopy. When extracellular water (ECW) or total body water (TBW) is measured with MLT-550N before and after hemodialysis, the change in ECW (ΔECW) or TBW (ΔTBW) is markedly larger than the change in body weight (ΔW). Good agreements between ΔECW and ΔTBW calculated by Moissl equations with ΔW were reported. The aim of this study was to develop novel equations to calculate the body fluid volume by modifying Moissl equations.
Methods
A total of 466 measurements of 351 hemodialysis patients were used to develop the novel equations. The equations were based on the agreement between ΔECW and ΔW as a guide. The volume of intracellular water was postulated to be constant during hemodialysis. For evaluation of the equations, 5485 measurements of 627 patients were used. Agreements between values of two groups were assessed with Lin’s concordance correlation coefficients. The normal edema ratio (ER = ECW/TBW) corrected with the fat ratio (fcER) according to the parameters of normally hydrated lean and adipose tissues was used as the reference for normal hydration. The fluid status at dry weight was considered to be close to normal. The absolute values of the deviated ratio of actual ER (aER) from fcER (dER = (aER−fcER)/fcER) were compared. In this study, 1 L of body water corresponded to 1.02 kg of body fluid according to a previous report.
Results
The concordance correlations between ΔW and 1.02∙ΔECW or 1.02∙ΔTBW with the novel equations were higher than with the MLT method or Moissl equations (0.896, 0.596 vs. 0.411, 0.375 or 0.813, 0.411, respectively). The median value of dER with the novel equations was the lowest (0.062) compared with those of the MLT method and Moissl equations (0.164 and 0.144) (p < 0.001).
Conclusions
The agreements between ΔECW or ΔTBW and ΔW were improved by the novel equations compared with the MLT method or Moissl equations. Based on the relation between aER and fcER at dry weight, the fluid volume calculated using the novel equations may be more adequate than those with the MLT method or Moissl equations.
Similar content being viewed by others
Background
Accurate assessment of the fluid status of hemodialysis (HD) patients poses great challenges for physicians. Bioimpedance spectroscopy (BIS) is a safe, convenient, and non-invasive method to evaluate the fluid status [1,2,3]. The basic theory of BIS for body fluid volume measurements was previously reported [4, 5]. Since extracellular (ECW) and intracellular (ICW) water contain ions, they are conducting and measurement of their volume is based on their resistance (Re and Ri, respectively). In the whole-body bioimpedance method, the human body is approximated as a cylinder. From the resistance-volume relationship for a single cylinder and Hanai’s mixture conductivity theory [6] on the effect of non-conducting tissues embedded in the body fluid, ECW is calculated as:
where H is height (cm) and W is body weight (kg). The details of the basic theory and the derivation of Eq. 1 are described in Appendix 1. Some previous reports assumed Ke as a constant according to sex [5]. In Moissl equations, personalized Ke is estimated from the body mass index (BMI) irrespective of sex [7]. A number of volume equations converting measured resistance and reactance to the body fluid volume have been published over the years [4, 5, 7,8,9]. However, the accuracy of the body fluid volume values given by these equations has not been established.
MLT-550N (SK Medical Electronics Co., LTD., Shiga, Japan) is one of the BIS devices commonly used in Japan. This device provides information on the body composition using whole-body BIS at 140 frequencies via electrodes placed on the wrist and ankle. The volume equations of the MLT method were developed using the fat-free mass determined by dual-energy X-ray absorptiometry as a reference [10] (Appendix 2). This device is also utilized for assessment of the fluid or nutritional status of HD patients. However, when ECW or total body water (TBW) is measured with MLT-550N before and after a HD session, it is frequently noted that the change in ECW (ΔECW) or TBW (ΔTBW) is markedly larger than the change in body weight (ΔW) [11]. This questions the reliability of fluid volume measurement with MLT-550N in HD patients. As a rule, equations for calculation of the fluid volume are appropriate for the population in which they were developed, but they are inappropriate for subjects with a different underlying pathology or variable hydration status [12]. Therefore, it may be necessary to develop novel equations for the determination of the fluid volume using BIS measured by MLT-550N for Japanese HD patients.
It was reported previously that the ultrafiltration volume (UFV), which corresponds to ΔW, closely agrees with the change in ECW (ΔECW) [13]. In this study, the equations to calculate ECW and intracellular water (ICW) reported by Moissl et al. [7] provided better estimation of the body fluid volume. Based on this report, we aimed to develop novel equations to calculate the body fluid volume using bioelectrical impedance data measured via MLT-550N by modifying the Moissl equations. We only used the agreement between ΔW and ΔECW as a guide for the novel equations. This retrospective study was approved by the Institutional Ethical Review Board of the Himeji Dokkyo University (No. 17–04).
Methods
Study design
Firstly, we developed novel equations to calculate the body fluid volume via BIS using MLT-550N based on the following assumptions. As mentioned above, we assumed that UFV closely agreed with the change in extracellular fluid (ECF) before and after hemodialysis (HD) and that intracellular fluid was constant during HD [13, 14]. UFV corresponds to the change in body weight (ΔW (kg)). In this study, extracellular fluid (ECF (kg)) was discriminated from extracellular water (ECW (L)), because body fluid contains minerals and proteins. Based on a previous report [15], ΔECF is equal to 1.02∙ΔECW. Therefore, the following equation was assumed:
where Δ stands for the change before and after HD.
Secondly, the actual agreements between ΔECW and ΔTBW calculated using the novel equations with ΔW were evaluated. Thirdly, the adequacy of assessment of the fluid status at the post-dialysis dry weight (DW) with the novel equations was compared with that with the MLT method or Moissl equations. DW was determined clinically by attending physicians based on the physical signs, blood pressure, cardiothoracic ratio, serum concentrations of atrial natriuretic peptide, and other methods used routinely. It was postulated that the fluid status at clinically determined DW was close to the normal hydration status.
Data analysis and statistics
Statistical analyses were performed using EZR [16] based on R commander. Values are presented as means ± standard deviations or medians with the first and third quartiles. Agreements between values of two groups were assessed with Lin’s concordance correlation coefficients (ρ) [17]. Correlation was estimated by Pearson’s correlation coefficients (R). Differences between two paired groups were examined by the paired t test or Wilcoxon’s signed rank test, if indicated. Differences among three corresponding groups were examined by the Friedman test. Post hoc analysis was performed by the Bonferroni test.
Measurements
Bioimpedance data were measured using MLT-550N before and after HD. Measurement was performed according to the attached manual of MLT-550N by experienced medical engineers and nurses. The data of the patients treated in various schedules (morning, afternoon, and night) of HD were incorporated taking the actual clinical use of this device into account. Therefore, the interval from the meal to BIS measurements was not consistent.
Principal for development of novel equations
Calculation of extracellular water
A total of 466 measurements of 351 patients collected from four collaborating institutions were used. The basal data are shown in Table 1.
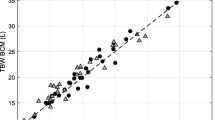
As expected, 1.02∙ΔECW of the MLT method was markedly greater than ΔW (ρ = 0.320, R = 0.772, Fig. 1a). The agreement of 1.02∙ΔECW of Moissl equations with ΔW was confirmed to be higher than that of MLT (ρ = 0.826, R = 0.828, Fig. 1b). Therefore, we decided to develop novel equations by modifying Moissl equations [7] as our preliminary plan. Moissl equations were as follows:
BMI is the body mass index. The value of ECW as a percentage of W was reported to be from 12.5 to 27% [18]. Because ECW calculated with Moissl equations (ECW(Mo)) as a percentage of the body weight is close to the upper limit even in the post-dialysis phase, as shown in Table 1, Ke was reduced by a coefficient of m (m < 1):
This value of m was determined to minimize the value of Eq. 9.
where ΔECW(m)i is the change in ECW(m)i before and after HD. The “i” stands for data number. The determined value of m was 0.8285. Since the coefficient of m also reduced ∆ECW(m) compared with ΔW, a corrected factor of c for the post-dialysis phase was introduced to increase ΔECW(m):
The subscript stands for the phase of each variable (pre- and post-HD). The corrected factor of c was determined by regression analysis using a logarithmically converted value of ΔW:
The “reg” stands for a regression equation.
Thus, the novel equations for ECW were as follows:
It must be noted that ECW(novel)post can be calculated independently from ECW(novel)pre. Thus, BIS measurement pre-HD is not necessary to calculate ECW(novel)post.
The reference value of ICW was not available in the current study. In this study, ICW was postulated to be constant during HD. Based on this postulation, the following equations were derived for ICW:
The details of development of the above Eqs. 12–15, are shown in Appendix 3.
Evaluation of novel equations
Supplemental data were collected after developing the novel equations for evaluation. The software provided with MLT-550N gives the fat mass (F). F for Moissl and the novel equations were calculated using the body weight, ECW, and TBW according to a previous report [15]. However, some clearly unrealistic data with a negative fat mass were included in these supplemental data (44 with the MLT method, 120 with Moissl equations in the pre-HD phase, and 21 with the MLT method, 144 with Moissl equations in the post-HD phase). These data were excluded, and a total of 5485 data from 627 patients including the original data for developing the novel equations were used for evaluation. The basic profile of these data is shown in Table 2. The agreements between 1.02 ∙ ∆ECW or 1.02 ∙ ∆TBW and ΔW were compared among the MLT method, Moissl equations, and novel equations.
The ratio of ECW to TBW (ECW/TBW) is often called the edema ratio (ER). It has been used as the measure of fluid overload [19]. The normal value of ER varies with a change in the fat ratio (f = F/W). The normal ER corresponding to each f value was termed the fat ratio-corrected normal ER (fcER). The relation between ER and f was derived using hydration parameters of normally hydrated lean tissue and adipose tissue [15] (Appendix 4). The absolute value of the deviation ratio of actual ER (aER) from fcER at DW was calculated according to the following Eq. 16 (dER), and they were compared among the MLT method, Moissl equations, and novel equations:
Results
The values of ECWpost as percentages of W (%ECWpost) were significantly different among the three groups (MLT method, Moissl equations, and the novel equations) (p < 0.001) (Table 2).
%ECW values with the MLT method were the lowest and those with Moissl equations were the highest. The relations between ΔW and 1.02∙∆ECW with the MLT method, Moissl equations, and novel equations in the evaluated data are shown in Fig. 2. The concordance correlation (ρ) and Pearson’s correlation coefficient (R) between ΔW and 1.02∙ΔECW or 1.02∙ΔTBW of MLT method, Moissl equations, and the novel equations are shown in Table 3. The value of ρ using the novel equations was the highest and that using the MLT method was the lowest. The value of R with the novel equations was the highest for 1.02∙ΔECW but R using the MLT method is the highest for 1.02∙ΔTBW.
As the fluid distribution in the body is potentially influenced by age and sex, the effects of these factors on the value of ρ between 1.02∙ΔECW using the novel equations and ΔW were examined. For age, the patients were divided into three groups (younger: under 65 years old, middle: from 65 to under 75 years old, older: equal to or over 75 years old). The numbers of data for each group were 1782, 1866, and 1837, respectively. The values of ρ in younger, middle, and older groups were 0.924, 0.867, and 0.849, respectively. The values of ρ in males and females were 0.908 and 0.847, respectively.
The relations between fcER or aER and f at DW are shown in Fig. 3. Because the fluid status at DW is considered to be close to normal hydration, aER is expected to be close to fcER if the fluid volume is adequately calculated. The median values (first quartile, third quartile) of dER using the MLT method, Moissl equations, and novel equations were as follows: 0.164 (0.076, 0.291), 0.144 (0.074, 0.211), and 0.062 (0.028, 0.110), respectively. They were significantly different from each other (p < 0.001). The aERs at DW with the novel equations were closer to fcERs compared with those using the MLT method or Moissl equations. The trends of aERs and fcERs along with f were reverse with the MLT method. Based on the relationship with fcERs, aERs using the novel equations were underestimated compared with those using Moissl equations in the lower f range. On the other hand, aERs with Moissl equations were markedly overestimated compared with those using the novel equations in the higher f range.
Discussion
In this study, we developed novel equations to calculate the body fluid volume from BIS data of MLT-550N. These equations were specialized for both HD patients and the device. The equations for pre-HD and post-HD phases were distinct. The change in ECW calculated with the novel equations closely agreed with the body weight change before and after HD compared with that calculated with the MLT method or Moissl equations. We postulated that the fluid status at clinically determined DW was close to normal. The values of %ECWpost were significantly different among the MLT methods, Moissl equations, and novel equations. The average value of %ECWpost of the novel equations was the closest to the average normal value (20%) [18], and that of the MLT method was underestimated, and that of Moissl equations was overestimated. Based on the postulation that patients had a normal fluid status at DW, actual edema ratios (aERs) of the patients were considered to be close to the fat ratio-corrected normal edema ratios (fcERs). As indicated in this study, aERs at DW with the novel equations were closer to fcERs compared with those using the MLT method or Moissl equations. These findings indicate that the body fluid volume of the novel equations was closer to the actual value compared with the MLT method or Moissl equations.
Appropriate estimation of total-body and limb muscle mass (TBMM) is crucial for evaluating the frailty of HD patients. TBMM is often calculated using the equation reported by Kaysen et al. [20]. Based on this equation, separating excess fluid mass from the body weight is necessary for accurate estimation of TBMM. The close estimation of the actual fluid volume of the novel equations may enable a more accurate estimation of TBMM.
The agreements between the changes in ECW and body weight before and after HD were lower in the older age group and females, although the reasons could not be clarified in this study. The equations developed for each sex or the equations incorporating the factor of age may achieve higher-level accuracy. However, since the Moissl equations that we used as the basis of the novel equations do not take these factors into consideration, we did not add these factors to the novel equations.
Generally, equations for calculation of the body fluid volume from BIS were developed by comparing impedance values with the corresponding reference fluid volume measured by the standard dilution method using reagents such as bromide [21] or deuterium oxide [22]. In this study, we used ΔW as the reference volume of ΔECW and compared this value with the change of impedance before and after HD. Owing to using this method, it was not necessary to administer any reagents to evoke possible deleterious adverse effects. Only data readily available in daily clinical services were used in this study.
The calculation of ECW with Moissl equations was based on relatively robust electrochemical basis [7]. Although we developed novel equations by modifying Moissl equations, our equations were based on an empirical approach. We introduced the “c” factor related to ΔW subtracted from Ke(m)post. This approach did not have any electrochemical basis. However, the following explanation may be possible. The impedance of body fluid is affected by the electrolyte composition. When the contents of electrolytes increase, the impedance of same-volume solutions decreases [23]. Therefore, when an identical value of Ke determined only from BMI is used to calculate ECW with higher electrolyte contents, the calculation results in an overestimation of ECW. Hyponatremia is often encountered in the pre-HD phase [24] due to dilution by ingesting free water in the interdialytic period. The effect of dilution may become more intense along with an increase of water ingestion resulting in an increase of ΔW. Because hyponatremia is corrected with HD, the contents of sodium are expected to increase post-HD. These considerations may support the utilization of reduced Ke (Ke(c)post) in the post-HD phase. However, as it is necessary to take the change of other electrolytes or diverse trends of patient-specific electrolyte compositions into consideration, the explanation is just one possibility. We used the corrected factor “c” for the reduction of Ke(m)post as the logarithmic regression equation of ΔW (creg) only on the basis of graphical approximation. This approach also lacks a robust physiological basis. In Moissl equations, Ke or Ki may be graphically approximated by linear regression equations of 1/BMI. These empirical approaches may be inevitable to develop equations for calculating the fluid volume from BIS.
As indicated in Fig. 2, relatively marked deviation of 1.02∙ΔECW from ΔW in the range of negative ΔW was noted for the novel equations. Negative ΔW means body weight gain after hemodialysis. Such cases were not included in the data for developing the novel equations. The novel equations may be inappropriate for calculation of the body fluid volume in the post-HD phase without a significant ultrafiltration volume.
In this study, there were no means to develop equations to calculate ICW. Although the MLT method and Moissl equations to calculate ICW were based on a different electrical equivalent model, calculated ICW volumes closely agreed with each other. We considered that this high-level agreement supported the reliance of these ICW values. As stated in the “Methods” section, we used the regression analysis between ICW calculated with Moissl equations and that of the MLT method due to the need to use the same electrical equivalent model as that used for ECW calculation (Moissl model). The lack of means to develop unique equations for ICW was a limitation of this study. Because ICW of the novel equations still markedly fluctuated between pre- and post-HD phases, the agreements of the novel equations between ΔTBW and ΔW were weaker than those between ΔECW and ΔW. However, the same tendency was noted for the MLT method and Moissl equations. Significant fluctuations of ICW measured soon after HD were reported previously, and the fluctuations became smaller after 30 to 120 min [14]. They reported that measurements taken soon after HD should be avoided, and the weaker agreement between ΔTBW and ΔW might be attributable to the measurements soon after HD used in this study.
The ratio of ECW to TBW, the edema ratio (ER) in this study, has been used as a measure of fluid overload. As there is a positive correlation between ER and age, ER is often corrected by age [19]. Instead of the correction, we used fat-ratio correction based on a previous report [15] in this study. This report argued that the composition of normally hydrated lean tissue and normally hydrated adipose tissue were the same irrespective of the age, sex, degree of obesity, and basal pathological condition. According to their report, the change in ER along with the change in age can be attributed to the change in the fat ratio. Therefore, we used the fat ratio-corrected normal edema ratio as a reference of the normal fluid status.
In this study, the interval from meals to BIS measurements was not consistent. Although measurement of body fluid via BIS may be affected by meals, the actual measurement in daily clinical settings is conducted with various intervals from meals. Therefore, measured data under various conditions were included in the data for development or evaluation of the current equations. Moreover, there is a report that although there were significant changes in body composition estimates after meals, these were small and within the imprecision of the impedance technique and so are unlikely to be of clinical significance [25]. Based on this report, we considered that the various intervals from meals to measurements might not have a significant impact on the results.
The agreements between ΔECW and ΔW or constant ICW before and after HD were the principal postulations in the current approach. These were based on previous reports [13, 14, 26]. However, there were some conflicting reports [27]. If these postulations are found to be erroneous, our approach will lose credibility. This is a major limitation of this study.
Although we postulated that clinically determined DW of each patient was adequate and their fluid status was close to normal, this postulation was not necessarily valid. The appropriateness of fluid volume calculation using the novel equations must be confirmed by comparisons with the fluid status evaluated by other methods, such as atrial natriuretic peptide levels [28], diameter of the inferior vena cava [29], or blood volume measurement during HD [30], in a future study.
The data with a negative fat mass were excluded from the additional data for evaluation of the novel equations. However, as shown in Fig. 3, some data with a markedly low or high fat ratio that was not realistic were still included. Because the adequate cut-off range for reasonable exclusion could not be determined, all data were used for evaluation, being another limitation of this study.
Conclusions
The novel equations for MLT-550N to calculate the fluid volume for hemodialysis patients were developed by modifying Moissl equations. The agreements between the change in extracellular water or total body water and body weight change were improved with the novel equations compared with the MLT method or Moissl equations. Based on the relation between the actual edema ratio and fat ratio-corrected normal edema ratio at dry weight, the fluid volume calculated by the novel equations may be more adequate than those by the MLT method or Moissl equations.
Abbreviations
- A :
-
Fraction of extracellular water in normally hydrated lean tissue
- a :
-
Mass of normally hydrated adipose tissue (kg)
- aER:
-
Actual edema ratio
- B :
-
Fraction of total water in normally hydrated lean tissue
- BIS:
-
Bioimpedance spectroscopy
- BMC:
-
Bone mineral content (kg)
- BMI:
-
Body mass index
- DW:
-
Dry weight (kg)
- ECF:
-
Extracellular fluid (kg)
- ECW:
-
Extracellular water (L)
- ER:
-
Edema ratio (ECW/TBW)
- F :
-
Fat mass (kg)
- f :
-
Fat ratio
- fcER:
-
Fat ratio-corrected normal edema ratio
- H :
-
Height (cm)
- HD:
-
Hemodialysis
- ICW:
-
Intracellular water (L)
- K :
-
Ratio of mass of normally hydrated adipose tissue to fat mass
- I :
-
Mass of normally hydrated lean tissue (kg)
- LTM:
-
Lean tissue mass (kg)
- M :
-
Fraction of extracellular water in normally hydrated adipose tissue
- N :
-
Fraction of total water in normally hydrated adipose tissue
- R0:
-
Impedance at zero frequency (Ω)
- Re:
-
Resistance of extracellular water (Ω)
- Ri:
-
Resistance of intracellular water (Ω)
- Rinf:
-
Impedance at infinite frequency (Ω)
- Rm:
-
Resistance of cell membrane (Ω)
- TBW:
-
Total body water (L)
- UFV:
-
Ultrafiltration volume (L)
- W :
-
Body weight (kg)
- Δ:
-
Standing for the change of before and after HD
References
Davies SJ, Davenport A. The role of bioimpedance and biomarkers in helping to aid clinical decision-making of volume assessments in dialysis patients. Kidney Int. 2014;86:489–96.
Spiegel DM, Bashir K, Fisch B. Bioimpedance resistance ratios for the evaluation of dry weight in hemodialysis. Clin Nephrol. 2000;53:108–14.
Chamney PW, Krämer M, Rode C, Kleinekofort W, Wizemann V. A new technique for establishing dry weight in hemodialysis patients via whole body bioimpedance. Kidney Int. 2002;61:2250–8.
Jaffrin MY, Morel H. Body fluid volumes measurements by impedance: a review of bioimpedance spectroscopy (BIS) and bioimpedance analysis (BIA) methods. Med Eng Phys. 2008;30:1257–69.
De Lorenzo A, Andreoli A, Matthie J, Withers P. Predicting body cell mass with bioimpedance by using theoretical methods: a technological review. J Appl Physiol. 1997;82:1542–58.
Hanai T. Theory of the dielectric dispersion due to the interfacial polarization and its application to emulsions. Colloid Polym Sci. 1960;171:23–31.
Moissl UM, Wabel P, Chamney PW, Bosaeus I, Levin NW, Bosy-Westphal A, Korth O, Müller MJ, Ellegård L, Malmros V, Kaitwatcharachai C, Kuhlmann MK, Zhu F, Fuller NJ. Body fluid volume determination via body composition spectroscopy in health and disease. Physiol Meas. 2006;27:921–33.
Matthie JR. Second generation mixture theory equation for estimating intracellular water using bioimpedance spectroscopy. J Appl Physiol. 2005;99:780–1.
Van Loan MD, Withers P, Matthie J, Mayclin PL. Use of bioimpedance spectroscopy to determine extracellular fluid, intracellular fluid, total body water, and fat-free mass. Basic Life Sci. 1993;60:67–70.
Tanaka K, Okuno J, Fujimoto T, Wada M, Uehara K, Ri H, Watanabe H, Nakadomo F. The utility for evaluation of body composition by multi-frequency bioimpedance spectroscopy – based on comparisons between DEXA and method of body fluid. Himankennkyu. 2000;6:68–75 (in Japanese).
Kotera H, Yashiro M, Kita T, Nishitani Y, Tanaka H, Sakai R. The evaluation of accuracy of body fluid volume measure using bioimpedance spectroscopy according to the change in body weight before and after hemodialysis. J Jpn Soc Dial Ther. 2014;47 suppl 1:665 (in Japanese).
Kyle U, et al. Bioelectrical impedance analysis part i: review of principles and methods. Clin Nutr. 2004;23:1226–43.
Dou Y, Liu L, Cheng X, Cao L, Zuo L. Comparison of bioimpedance methods for estimating total body water and intracellular water changes during hemodialysis. Nephrol Dial Transplant. 2011;26:3319–24.
Wabel P, Rode C, Moissl U, Chamney P, Wizemann V. Accuracy of bioimpedance spectroscopy (BIS) to detect fluid status changes in hemodialysis. Nephrol Dial Transplant. 2007;22(6(suppl)):Vi129.
Chamney PW, Wabe K, Moissl UM, et al. A whole-body model to distinguish excess fluid from the hydration of major body tissues. Am J Clin Nutr. 2007;85:80–9.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statics. Bone Marrow Transplant. 2013;48:452–8.
Lin LI. A concordance correlation coefficient to evaluate reproducibility. Biometrics. 1989;45:255–68.
Mount DB. Fluid and electrolyte imbalances. In: Long DL, Fauci AS, Hauser SL, Jameson JL, Loscalzo J, editors. Harrison’s principles of internal medicine, 18th ed., 4th Japanese ed., Tokyo: Medical Sciences International, Ltd; 2013. p. 288–305 (in Japanese).
Lopot F, Nejedlý B, Novotná H, Macková M, Sulková S. Age-related extracellular to total body water volume ratio (Ecv/TBW)--can it be used for "dry weight" determination in dialysis patients? Application of multifrequency bioimpedance measurement. Int J Artif Organs. 2002;25:762–9.
Kaysen GA, Zhu F, Sarkar S, Heymsfield SB, Wong J, Kaitwatcharachai C, Kuhlmann MK, Levin NW. Estimation of total-body and limb muscle mass in hemodialysis patients by using multifrequency bioimpedance spectroscopy. Am J Clin Nutr. 2005;82:988–95.
Miller ME, Cosgriff JM, Forbes GB. Bromide space determination using anion-exchange chromatography for measurement of bromide. Am J Clin Nutr. 1989;50:168–71.
Schloerb PR, Friis-Hansen BJ, Edelman IS, Solomon AK, Moore FD. The measurement of total body water in the human subject by deuterium oxide dilution; with a consideration of the dynamics of deuterium distribution. J Clin Invest. 1950;29:1296–310.
Scharfetter H, Wirnsberger GH, Holzer H, Hutten H. Influence of ionic shifts during dialysis on volume estimations with multifrequency impedance analysis. Med Biol Eng Comput. 1997;35:96–102.
Zhang R, Wang S, Zhang M, Cui L. Hyponatremia in patients with chronic kidney disease. Hemodial Int. 2017;21:3–10.
Androutsos O, Gerasimidis K, Karanikolou A, Reilly JJ, Edwards CA. Impact of eating and drinking on body composition measurements by bioelectrical impedance. J Hum Nutr Diet. 2015;28:165–71.
Schneditz D, Roob J, Oswald M, et al. Nature and rate of vascular refilling during hemodialysis and ultrafiltration. Kidney Int. 1992;42:1425–33.
Kumar S, Khosravi M, Massart A, Potluri M, Davenport A. Haemodiafiltration results in similar changes in intracellular water and extracellular water compared to cooled haemodialysis. Am J Nephrol. 2013;37:320–4.
Plum J, Grabensee B. Atrial natriuretic peptide in dialysis patients under various conditions of volume homeostasis. J Intern Med. 1991;229:209–16.
Ando Y, Yanagiba S, Asano Y. The inferior vena cava diameter as a marker of dry weight in chronic hemodialyzed patients. Artif Organs. 1995;19:1237–42.
Rodriguez HJ, Domenici R, Anne D, Goykhman I. Assessment dry weight by monitoring changes in blood volume during hemodialysis using Crit-Line. Kidney Int. 2005;68:854–61.
Cole KS, Cole RH. Dispersion and absorption in dielectrics. I. Alternating current characteristics. J Chem Phys. 1941;9:341–51.
Acknowledgements
We appreciate the collaboration for data collection of Nozatomo Clinic (Hyogo), Honma Hospital (Yamagata), Hakuyuchiyoda Clinic (Osaka), and Iwakura Hospital (Aichi). We thank Dr. Ishii Y, Kobayashi S (Nozatomo Clinic), Dr. Sugawara T, Igarashi K (Honma Hospital), Dr. Okada N, Imamura M (Hakuyuchiyoda clinic), Dr. Takada M, and Nagao H (Iwakura Hospital) for their support.
Funding
This study was supported by funds provided by Toray Medical Co., Ltd.
Availability of data and materials
The datasets of the patients generated and/or analyzed during the current study are not publicly available because there is no approval other than for the utilization of the datasets of the patients for this current study. The datasets are available from the corresponding author on reasonable request if approval from the collaborating institutions is given.
Author information
Authors and Affiliations
Contributions
MY developed the novel equations, organized the study, and prepared the manuscript. HK made significant recommendations for the study and manuscript and performed the preliminary study. Both authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This retrospective study was approved by the Institutional Ethical Review Board of Himeji Dokkyo University (No. 17–04).
Consent for publication
All data were anonymized in this study. Consent for publication was obtained thorough collaborating institutions.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1
The basic theory of BIS and the derivation of Eq. 1
The simple circuit model of a human body represents the current path into two parallel branches, one through ECW and the other through ICW. The simplest electrical equivalent model is shown in Fig. 4a. The path of ECW is considered purely resistive while the intracellular path includes the capacitive effects in the cell membrane (Cm). Owing to these capacitive effects, the magnitude of impedance of the intracellular path is dependent on the frequency. For technical reasons, impedance measured using surface electrodes is limited to a frequency range of 5–1000 kHz. The locus of impedance data at multi-frequencies in the resistance-reactance plane lies on a semicircle with its center below the horizontal axis according to the Cole model [31]. Total resistance at 0 (R0) and infinite (Rinf) frequencies can be described as:
Re and Ri can be calculated from Eqs. 17 and 18, when R0 and Rinf are estimated. These values (R0 and Rinf) cannot be measured directly, but they can be estimated by extrapolation of the Cole-Cole semicircle [31].
In the whole-body bioimpedance method, the human body is approximated as a cylinder. The resistance-volume relationship for a single cylinder is:
where R is the resistance of the human body (Ω), Kb is a shape factor (dimensionless), ρ is resistivity (Ωcm), H is the height (cm), and Vb is the body volume (cm3). When the effect of non-conducting tissues embedded in ECW and ICW, which increases their resistivity, is taken into account, the actual resistivity (ρa) is calculated as Eq. 20, based on Hanai’s mixture conductivity theory [6]:
where r is the volume fraction of non-conducting tissues. At 0 frequency, the current is considered to pass exclusively through the extracellular space, and the volume fraction of non-conducting tissues is equal to:
where ECW is the volume of extracellular water (L). Using Eqs. 20 and 21, ρa is written as:
where ρe is the resistivity of ECW. Vb is written as:
where W (kg) is the body weight and Db (kg/L) is its density. Using Eq. 23, Eq. 22 is written as:
Using Eqs. 17, 23, and 24, Eq. 19 at 0 frequency can be written as:
Thus, ECW is written as:
The first half of the right of Eq. 26 can be regarded as a constant:
Thus, ECW is calculated as Eq. 1 in the main text.
Appendix 2
Equations of MLT method
The electrical equivalent model for the MLT method contains the resistance of the cell membrane (Rm, Fig. 4b) and is distinct from the simplest circuit model. The equations of MLT method are as follows:
Rm = 400(male), 300(female).
Male, P = 0.3879, Q = 0.3153, R = 0.0001453, S = 0.05117 α = 2.3
Female, P = 0.3675, Q = 0.2219, R = 0.0007983, S = 0.10227 α = 2
Appendix 3
Development of novel equations
Since ΔECW(m)i is m∙ΔECW(Mo)i, Eq. 9 in the main text is
The value of m to minimize Eq. 39 is:
As described in the main text, the value of m to reduce ECW calculated with Moissl equations was 0.8285. The regression equation with 0 of the intercept between 1.2 ∙ ∆ECW(m) and ΔW is as:
The “reg” stands for a regression equation. The use of Ke(m) can reduce ECW(m) but it causes the underestimation of 1.02 ∙ ∆ECW(m) compared with ΔW as indicated in Eq. 41. We hypothesized that Ke(m) in the post-HD phase decreases from Ke(m)post by c in order to increase ΔECW as mentioned in the main text. Using Eq. 10, ECW(c)post is written as:
ΔECW can be expressed as the following equation:
Using Eqs. 2–4, 7, 8, 10, and 42, Eq. 43 is as follows:
Equation 44 is transformed as follows:
The values on the right of Eq. 45 were plotted along with ΔW (Fig. 5). Based on graphical approximation, the regression equation to calculate c (creg) from logarithmically converted values of ΔW was determined based on a fitting method as Eq. 11. The correlation coefficient between c and ΔW in logarithmic regression analysis was higher than that in linear regression analysis (R = 0.510). Finally, ECW was calculated as Eqs. 12 and 13.
The reference value of ICW was not available in the current study. The concordance correlation coefficients (ρ) between ICW of the MLT method (ICW(MLT)) and that of Moissl equations (ICW(Mo)) are relatively high in both pre- and post-HD phases (ρ = 0.937 and ρ = 0.961, respectively). Based on high-level agreement between ICW(MLT) and ICW(Mo), we considered that both were close to the actual ICW value. In this study, ICW was postulated to be constant during HD. The changes in ICW during HD were compared between MLT (ΔICW(MLT)) and Moissl (ΔICW(Mo)). The values of ΔICW(MLT)2 were significantly lower than those of ΔICW(Mo)2 based on Wilcoxon’s signed rank test (p < 0.001). Therefore, we considered that ICW(MLT) is more compatible with the postulation of ICW constancy during HD than ICW(Mo). However, the electrical equivalent model of the MLT method containing resistance of the cell membrane is distinct from the Moissl model. We decided to calculate ICW from ICW(Mo) using a linear regression equation between ICW(Mo) and ICW(MLT) in the current approach instead of the direct utilization of ICW(MLT), because a consistent electrical equivalent model (Moissl model) must be used for both ECW and ICW. Thus, Eqs. 14 and 15 in the main text were derived using regression analysis.
Appendix 4
Calculation of fat ratio-corrected normal edema ratio
K = 1.328, A = 0.266, M = 0.127, B = 0.703, N = 0.197 [9].
Equations 48 and 49 can be written by substituting l and a with K, F, and W using Eqs. 46 and 47:
The edema ratio (ECW/TBW) can be written as follows:
Equation 52 can be written as follows by substituting F/W with the fat ratio (f = F/W):
The actual values were substituted for the parameters respectively. This edema ratio was denoted as the fat-ratio corrected normal edema ratio (fcER):
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Yashiro, M., Kotera, H. Novel equations for bioimpedance spectroscopy to calculate body fluid volume based on the agreement between body weight and extracellular water change before and after hemodialysis as a guide. Ren Replace Ther 5, 7 (2019). https://doi.org/10.1186/s41100-019-0203-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41100-019-0203-1