Abstract
Background
The definition and guideline of sepsis and septic shock were recently updated. The aim of this study is to evaluate the ability of Third Consensus Definitions of Sepsis and Septic Shock (Sepsis-3) to predict outcomes among patients with community-acquired sepsis receiving continuous renal replacement therapy (CRRT).
Methods
We conducted a retrospective observational study between January 2013 and December 2015 in a single university hospital. From 368 patients receiving CRRT for various reasons, 64 patients who suffered from community-acquired sepsis and required CRRT were selected and evaluated using the current and previous sepsis criteria. We additionally assessed infection characteristics. The primary outcome was 28-day mortality, and the secondary outcome was in-hospital mortality.
Results
Of the 64 participants (70.3% male, median age 66.5 years), 33 (51.6%) administered antimicrobials before admission. The most common source of infections was pneumonia, and 27 participants (42.2%) had positive cultures. The Sepsis-3 criteria identified 64 cases (100%) as sepsis at the start of CRRT, while the previous criteria identified 44 cases (68.8%). According to the Sepsis-3 criteria, the 28-day mortality of sepsis and septic shock were 31.3% (20/64) and 46% (17/37), and in-hospital mortality was 43.8% (28/64) and 62.2% (23/37), respectively. Septic shock diagnosed using the Sepsis-3 criteria predicted mortality (log-rank P = 0.0001); however, using the previous criteria was not associated with mortality (log-rank P = 0.437). Among variables, lactate levels ≥ 2 mmol/L and SOFA score ≥ 14 were significantly associated with mortalities, with an optimal cutoff value for lactate of 1.8 mmol/L (AUC 0.777, sensitivity 85.7%, specificity 58.3%). Although age ≥ 65 years predicted in-hospital mortality, and pre-hospital antimicrobial therapy tended to be associated with 28-day mortality, we did not detect any association between outcomes and the CRRT regimen or general risk factors (e.g., acute kidney injury, serum creatinine levels, and comorbidities).
Conclusions
Our data suggests that the Sepsis-3 criteria predicted survival more accurately than the previous criteria among patients with community-acquired sepsis receiving CRRT. This is based on lactate levels and SOFA scores being strongly associated with mortality.
Similar content being viewed by others
Background
Sepsis and septic shock are the most common contributing factors to acute kidney injury (AKI) in critically ill patients and account for approximately 50% of AKI cases in intensive care units (ICU) [1]. Septic AKI has a higher mortality rate than non-septic AKI [2,3,4,5]. Continuous renal replacement therapy (CRRT) is used to address sepsis-related renal failure and improve outcomes by stabilizing circulation and removing inflammatory mediators [6]. It has been reported that early diagnosis and treatment using appropriate antimicrobials can reduce mortality from sepsis [7,8,9]. Although early initiation of renal replacement therapy may contribute to reduced mortality [10,11,12], there is limited evidence about the usefulness of CRRT in sepsis [13,14,15]. Recent reports have clarified clinical features associated with mortality in patients with sepsis-related AKI receiving CRRT [16]. However, most of these studies included patients with nosocomial sepsis, such as postoperative cases, and there are few reports about clinical features and prognosis of patients who required CRRT for community-acquired sepsis.
Definitions of sepsis and septic shock have evolved since the early 1990s. Sepsis-1 [17] and Sepsis-2 [18] defined sepsis as a systemic inflammatory response caused by infection, and the systemic inflammatory response syndrome (SIRS) criteria were used to identify cases of sepsis. However, in 2016, the Third Consensus Definitions of Sepsis and Septic Shock (Sepsis-3) provided a more precise approach to diagnosing sepsis [19]. Sepsis-3 defines sepsis as a life-threatening organ dysfunction caused by a dysregulated host response to infection and recommends using the Sequential Organ Failure Assessment (SOFA) score to monitor patients in the ICU for organ dysfunction and sepsis. A simpler quick SOFA (qSOFA) score has also been developed for use in non-ICU patients with infection, and lactate levels have become indispensable for diagnosing septic shock.
Some studies have compared the utility of the Sepsis-3 criteria to that of the previous definitions [20]. However, few studies have investigated whether Sepsis-3 is useful for evaluating patients who require CRRT. Therefore, the present study examined the characteristics of patients who required CRRT for community-acquired sepsis and assessed the ability of Sepsis-1 and Sepsis-3 to predict clinical outcomes.
Methods
Study design
This study was a retrospective observational study conducted at the Tohoku University Hospital, a university hospital in Miyagi Prefecture, Japan. The study was approved by the Ethics Committee of the Tohoku University Graduate School of Medicine (2016-1-008).
Participant selection
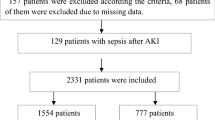
Patients attending the ICU or emergency department (ED) between January 2013 and December 2015 who had primary infections and performed CRRT were screened for inclusion in this study. During the study period, 368 patients performed CRRT for various reasons. As shown in Fig. 1, the exclusion criteria were cardiopulmonary arrest on admission, burns, traffic injuries, drug poisoning, heat stroke, organ transplantation surgery (including bone marrow transplantation), age of < 18 years, pregnancy, chronic maintenance dialysis, previous renal transplantation, and insufficient data at admission. We also excluded 86 patients who performed CRRT for non-infectious diseases and a further 111 who had secondary infections, such as nosocomial infections that developed after a scheduled surgery or examination, and the underlying disease for hospitalization. We ultimately identified 64 patients with primary infectious diseases who started CRRT within 72 h of hospitalization, who became our study participants (Fig. 1).
Data collection
We used medical records for the 64 participants to collect the following information: age, sex, body mass index, underlying medical conditions, date and cause of admission, time and reason for CRRT administration, CRRT type, clinical and physiological data at the time of hospitalization and the start of CRRT, origin of infection, laboratory data at the start of CRRT (including lactate levels), Acute Physiology and Chronic Health Evaluation (APACHE) II score [21], and SOFA score [22].
Sepsis definitions
We used Sepsis-3 and Sepsis-1 criteria to diagnose sepsis and septic shock and compared the results. Sepsis-1 was used as the reference because previous studies had reported that Sepsis-1 and Sepsis-2 had similar diagnostic performances, but Sepsis-1 was simpler and more frequently used [23]. Sepsis was evaluated at admission and the start of CRRT. Using Sepsis-3 criteria, sepsis was diagnosed at admission in participant with a qSOFA score ≥ 2, and at the start of CRRT in participants, a SOFA score ≥ 2. Using Sepsis-1 criteria, sepsis was diagnosed in participants with any SIRS score ≥ 2.
Septic shock was only evaluated at the start of CRRT, that is when reliable lactic acid levels were available. Using Sepsis-3 criteria, septic shock was diagnosed when vasopressor treatment was required to maintain a mean arterial pressure ≥ 65 mmHg in the absence of hypovolemia and lactate levels were > 2 mmol/L. Using Sepsis-1 criteria, septic shock was diagnosed based on perfusion abnormalities and hypotension (a systolic blood pressure < 90 mmHg, a reduction in systolic blood pressure ≥ 40 mmHg from baseline, or receiving vasopressor agents), despite adequate fluid resuscitation.
Other definitions
The severity of AKI was evaluated using serum creatinine levels, based on the Kidney Disease Improving Global Outcomes (KDIGO) classification [24]. Urine output and CRRT were not considered in this assessment. Baseline serum creatinine levels were defined as the level at the time of hospitalization, the most recent data from before admission, or the estimated serum creatinine level (based on the KDIGO guidelines) for patients with no information regarding prior kidney function.
The time of CRRT initiation was ascertained based on clinical status of each patient that included factors such as severe shock, increase in serum creatinine level, and decreased urine output. The attending physician determined the time of initiation and CRRT regimen.
All patients underwent central venous catheterization, and the dialysis membrane was changed every 24 h, or earlier if clotting occurred.
Cultures collected within 48 h of admission or performed before hospitalization were used to identify causative pathogens. Patients were classified as having positive cultures if the same bacteria were detected in two cultures of blood or other specimens (e.g., sputum, urine, abdominal ascites, or pus). Any antimicrobial administered before admission was classed as pre-hospital antimicrobial therapy.
Outcome
The primary outcome was 28-day mortality, and the secondary outcome was in-hospital mortality.
Statistical analysis
Data were reported as median (interquartile range) or number (%). Statistical significance was set at P < 0.05. Correlations were calculated using the non-parametric Spearman rank test. Fisher’s exact test was used to assess the association of categorical variables with mortality. Univariate and multivariate logistic regression models were used to evaluate the relative risks of mortality, with results presented as odds ratios (OR) and 95% confidence intervals. The factors identified as clinically related to the outcome on univariate analysis (based on P value ≤ 0.20) were included in the multivariate analysis. Receiver operating characteristic (ROC) curve analyses were performed to identify cutoff values, areas under the curve (AUC), sensitivities, and specificities. Survival was analyzed using Kaplan-Meier survival curves and the log-rank test. All analyses were performed using JMP Pro software version 12.2.0 (SAS Institute Inc.).
Results
Participant characteristics
The characteristics and laboratory data of the 64 participants (70.3% male, median age 66.5 years) are shown in Table 1. The median APACHE II score was 31, the median SOFA score was 11, the median lactate level was 2.25 mmol/L, and 51.6% of participants had received pre-hospital antimicrobial therapy.
The sources of infection and the culture results are shown in Table 2. The most common source of infection was pneumonia, followed by pancreatitis. Among the 27 participants (42.2%) with positive cultures, the most common causal agents were Gram-positive bacteria, then Gram-negative bacteria. Most Gram-positive sepsis originated as a soft tissue infection or infective endocarditis, and most Gram-negative sepsis originated as a urinary tract infection. More than half of the participants received pre-hospital antimicrobial therapy, and no antimicrobial-resistant bacteria were detected within 48 h of admission.
Regarding the initial antimicrobial agents, Carbapenem was most commonly used in 40 cases (62.5%), as the empiric antimicrobial therapy. About the number of initial antimicrobial agents, only one drug was used in 35 cases (54.7%), and two drugs were used in 21 cases (32.8%), respectively. In 8 cases (12.5%), more than three drugs were used for initial treatment.
The details of the CRRT regimes are summarized in Table 3. Filters having high-adsorption capability, such as polymethylmethacrylate (PMMA) and AN69ST, were frequently used in 33 cases (51.6%) and 11 cases (17.2%), respectively.
Diagnosing sepsis using Sepsis-1 and Sepsis-3 criteria, and those outcomes
Figure 2 shows the diagnosis of sepsis using Sepsis-3 and Sepsis-1 criteria. The Sepsis-3 criteria identified 27 cases (42.2%) at admission and 64 cases (100%) at the start of CRRT (Fig. 2a). On the other hand, the Sepsis-1 criteria identified 53 cases (82.8%) at admission, but only 44 cases (68.8%) at the start of CRRT (Fig. 2b).
Among 64 participants, 20 (31.3%) died within 28 days, and 28 (43.8%) died in hospital. As shown in Table 4, the participants diagnosed with septic shock using the Sepsis-3 criteria had higher mortality rates than the participants without septic shock, both 28-day (46.0 vs 11.1%, P = 0.003) and in-hospital mortality (62.2 vs 18.5%, P = 0.0005), respectively. On the other hand, Sepsis-1 criteria could not detect any significance for both 28-day mortality (42.9 vs 25.6%, P = 0.16) and in-hospital mortality (52.4 vs 39.5%, P = 0.33). Sepsis-3 criteria were superior to Sepsis-1 in predicting survival.
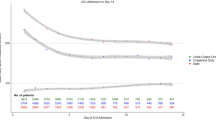
The Kaplan-Meier survival curves are shown in Fig. 3. Participants diagnosed with septic shock using the Sepsis-3 criteria had a significantly higher mortality rate than participants without septic shock (log-rank P = 0.0001) (Fig. 3a), while no significant difference was observed using the Sepsis-1 criteria (Fig. 3b).
Risk factors
The univariate analyses revealed that both 28-day and in-hospital mortality were significantly associated with lactate levels ≥ 2 mmol/L, SOFA scores ≥ 14, and septic shock diagnosed using the Sepsis-3 criteria. Age > 65 years was only associated with in-hospital mortality (Tables 5 and 6). The multivariate analyses revealed that 28-day mortality was independently associated with lactate levels ≥ 2 mmol/L, and pre-hospital antimicrobial therapy tended toward significance (Table 5), while in-hospital mortality was independently associated with age > 65 years and lactate levels ≥ 2 mmol/L (Table 6).
As a continuous variable, lactate levels were strongly associated with in-hospital mortality. ROC analysis of in-hospital mortality revealed an optimal cutoff value for lactate levels of 1.8 mmol/L (AUC 0.777, sensitivity 85.7%, specificity 58.3%). In-hospital mortality was less strongly associated with SOFA score (AUC 0.67), APACHE II score (AUC 0.528), and age (AUC 0.637).
Among SOFA organ sub-scores, coagulation (OR = 1.55, P = 0.046), hepatic function (OR = 1.85, P = 0.014), and central nervous system (OR = 1.55, P = 0.025) were significantly associated with 28-day mortality, while respiratory, circulatory, and renal were not. Additionally, the hepatic function sub-score was significantly correlated with lactate levels (Spearman ρ = 0.35, P = 0.005). Regarding the source of infection, pneumonia which was the most common in this study was not associated with 28-day mortality, but it was significantly associated with in-hospital mortality (OR = 3.79, P = 0.046).
We did not detect any association between outcomes and regimen of CRRT, polymyxin B-immobilized fiber column direct hemoperfusion (PMX-DHP) combination, or general risk factors (e.g., AKI, serum creatinine levels, and comorbidities).
Discussion
The present study evaluated the usefulness of Sepsis-3 for predicting mortality among patients with primary infections who required CRRT. Mortality was associated with higher lactate levels, SOFA scores, and a septic shock diagnosis of Sepsis-3 criteria (lactate level ≥ 2 mmol/L). Diagnosis with Sepsis-3 criteria is very accurate to discriminate septic shock from sepsis and is better for predicting survival than diagnosis with Sepsis-1 criteria. In the present study, lactate levels were the most critical risk factor for the participants. Lactate levels are known to reflect the condition of critically ill patients, and their prognostic value had been identified in previous studies of patients with sepsis [25,26,27], and patients who required CRRT [28, 29]. Our results support those findings.
According to Sepsis-3, sepsis is defined as a “life-threatening organ dysfunction caused by a dysregulated host response to infection” [19], and the participants of this study were in severe condition, requiring CRRT. As expected, using the Sepsis-3 criteria, all participants were diagnosed with sepsis based on their SOFA score at the start of CRRT. However, the qSOFA score at admission only identified 42.2% of these cases, and it was not associated with mortality rates. Therefore, the clinical course of patients should be carefully followed even if qSOFA is low, and it may be appropriate to use the SOFA score to evaluate a patient’s condition from an early stage. In contrast, Sepsis-1 criteria (using SIRS scores) identified sepsis in 53 patients (82.8%) at admission and in only 44 patients (68.8%) at the start of CRRT (Fig. 2). Thus, 9 patients experienced a reduction in their SIRS score to < 2 between admission and starting CRRT, although their outcomes were similar to participants with higher SIRS scores. It revealed that SIRS scores had the limitation on evaluating and predicting outcomes for patients in the ICU, as they do not consider the effects of interventions, such as respirator and vasopressor treatment.
With regard to the influence of each organ dysfunction on the outcome, our statistical analysis revealed that AKI was not associated with mortality. In addition, SOFA organ sub-scores of respiratory, circulatory, and renal were not significantly associated with mortality. The reason for this may be that organ injury of these systems could be treated with advanced strategies for mechanical ventilation, vasopressor, and CRRT. We think that hepatic dysfunction may be particularly important in SOFA organ sub-scores because the liver plays a crucial role to lactate metabolism. In fact, in this study, the hepatic function sub-score was significantly correlated with a lactate level which had a major influence on mortality.
About the time of CRRT initiation, it is controversial whether early initiation of CRRT improve survival outcome or not [11, 12, 16, 30]. Although CRRT can correct uremic status and acid-base balance, survival may depend on the control of systemic lactate production in septic shock. The median serum creatinine level at the start of CRRT was 2.78 mg/dL in this study, and 26.6% of the participants did not meet definition of AKI by serum creatinine levels. In other words, there were some patients treated with CRRT by “non-renal indication” in this study, and they must have acidemia and/or high lactate levels because the medians (interquartile range) of pH and lactate were 7.35 (7.29–7.40) and 2.25 (1.22–4.01), respectively (Table 1). It is speculated that the initiation of CRRT was decided not only to supplement renal function but also to treat the critical multiple organ disorders associated with serious lactate retention. This is also suggested by the fact that the attending physicians tended to choose the hemofilter, which had the absorption characteristics.
This study also focused on the infection characteristics and the prognosis of the patients with community-acquired sepsis who required CRRT. Among various infectious diseases, pneumonia can easily cause hypoxia, and the hypoxia of multiple organs leads to serious lactate retention. This may be the reason why pneumonia was the most common source of infection in our study and the associated mortality was high among patients who required CRRT for community-acquired sepsis. Interestingly, positive culture results were not associated with mortality, while pre-hospital antimicrobial therapy had a clear trend as a risk factor for 28-day mortality. This result may reflect the fact that these patients started CRRT relatively late after the onset of their infection. Unfortunately, the present study was not able to accurately identify the timing of onset or pre-hospital course of the infection, so we cannot definitively comment on those relationships.
The present study had several limitations. First, because this was a single-center retrospective study, we only investigated a small number of patients with community-acquired sepsis who required CRRT and did not consider all patients with sepsis at our center. In order to simply compare Sepsis-1 and Sepsis-3 for diagnosis ability of sepsis, we need to extend the target population. Second, our findings may be biased because of the absence of standardized requirements for determining the time of CRRT initiation. Third, we did not measure cytokines or biomarkers relevant to sepsis cases, so we were unable to comment on underlying biology that might affect findings. Even if the sample size is small, we believe that the present study provides useful data for the following two reasons. Only a few studies have considered the Sepsis-3 criteria for diagnosing sepsis among patients who require CRRT, and the baseline data includes relatively uniform and detailed infectious characteristics because our cohort consists of a single-center community-acquired sepsis without in-hospital onset.
Considering the recent Japanese sepsis registry [31], which was successful in evaluating standard quality of care and mortality based on the international Surviving Sepsis Campaign guidelines, a similar prospective study of patients who required CRRT must be needed. Further research is required to validate our findings and to conduct a multicenter registry system considering the Sepsis-3 criteria for diagnosing sepsis among patients who required CRRT.
Conclusions
The experience at our center suggests that SOFA scores and lactate levels are strongly associated with mortality and that diagnosing septic shock with Sepsis-3 criteria is critical for predicting outcomes for patients who required CRRT for community-acquired sepsis. We concluded that in this population, Sepsis-3 criteria discriminated septic shock from sepsis very well, and it predicted outcomes, especially survival, more accurately than the previous criteria.
Abbreviations
- AKI:
-
Acute kidney injury
- APACHE:
-
Acute Physiology and Chronic Health Evaluation
- AUC:
-
Areas under the curve
- CI:
-
Confidence interval
- CPA:
-
Cardiopulmonary arrest
- CRRT:
-
Continuous renal replacement therapy
- CTA:
-
Cellulose triacetate
- ED:
-
Emergency department
- ICU:
-
Intensive care unit
- KDIGO:
-
The Kidney Disease Improving Global Outcomes
- OR:
-
Odds ratio
- PES:
-
Polyethersulfone
- PMMA:
-
Polymethylmethacrylate
- PMX-DHP:
-
Polymyxin B-immobilized fiber column direct hemoperfusion
- PS:
-
Polysulfone
- qSOFA:
-
Quick SOFA
- ROC:
-
Receiver operating characteristic
- Sepsis-3:
-
The Third Consensus Definitions of Sepsis and Septic Shock
- SIRS:
-
The systemic inflammatory response syndrome
- SOFA:
-
The Sequential Organ Failure Assessment
References
Uchino S, Kellum JA, Bellomo R, Doig GS, Morimatsu H, Morgera S, Schetz M, Tan I, Bouman C, Macedo E, et al. Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA. 2005;294:813–8.
Bagshaw SM, George C, Bellomo R. Early acute kidney injury and sepsis: a multicentre evaluation. Crit Care. 2008;12:R47.
Bagshaw SM, Uchino S, Bellomo R, Morimatsu H, Morgera S, Schetz M, Tan I, Bouman C, Macedo E, Gibney N, et al. Septic acute kidney injury in critically ill patients: clinical characteristics and outcomes. Clin J Am Soc Nephrol. 2007;2:431–9.
Nagata I, Uchino S, Tokuhira N, Ohnuma T, Namba Y, Katayama S, Kawarazaki H, Toki N, Takeda K, Yasuda H, et al. Sepsis may not be a risk factor for mortality in patients with acute kidney injury treated with continuous renal replacement therapy. J Crit Care. 2015;30:998–1002.
Neveu H, Kleinknecht D, Brivet F, Loirat P, Landais P. Prognostic factors in acute renal failure due to sepsis. Results of a prospective multicentre study. The French Study Group on Acute Renal Failure. Nephrol Dial Transplant. 1996;11:293–9.
Schetz M. Non-renal indications for continuous renal replacement therapy. Kidney Int Suppl. 1999;56:S88–94.
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41:580–637.
Ferrer R, Artigas A, Suarez D, Palencia E, Levy MM, Arenzana A, Perez XL, Sirvent JM, Edusepsis Study G. Effectiveness of treatments for severe sepsis: a prospective, multicenter, observational study. Am J Respir Crit Care Med. 2009;180:861–6.
Gaieski DF, Mikkelsen ME, Band RA, Pines JM, Massone R, Furia FF, Shofer FS, Goyal M. Impact of time to antibiotics on survival in patients with severe sepsis or septic shock in whom early goal-directed therapy was initiated in the emergency department. Crit Care Med. 2010;38:1045–53.
Karvellas CJ, Farhat MR, Sajjad I, Mogensen SS, Leung AA, Wald R, Bagshaw SM. A comparison of early versus late initiation of renal replacement therapy in critically ill patients with acute kidney injury: a systematic review and meta-analysis. Crit Care. 2011;15:R72.
Zarbock A, Kellum JA, Schmidt C, Van Aken H, Wempe C, Pavenstadt H, Boanta A, Gerss J, Meersch M. Effect of early vs delayed initiation of renal replacement therapy on mortality in critically ill patients with acute kidney injury: the ELAIN randomized clinical trial. JAMA. 2016;315:2190–9.
Gaudry S, Hajage D, Schortgen F, Martin-Lefevre L, Pons B, Boulet E, Boyer A, Chevrel G, Lerolle N, Carpentier D, et al. Initiation strategies for renal-replacement therapy in the intensive care unit. N Engl J Med. 2016;375:122–33.
Heering P, Morgera S, Schmitz FJ, Schmitz G, Willers R, Schultheiss HP, Strauer BE, Grabensee B. Cytokine removal and cardiovascular hemodynamics in septic patients with continuous venovenous hemofiltration. Intensive Care Med. 1997;23:288–96.
Hoffmann JN, Hartl WH, Deppisch R, Faist E, Jochum M, Inthorn D. Effect of hemofiltration on hemodynamics and systemic concentrations of anaphylatoxins and cytokines in human sepsis. Intensive Care Med. 1996;22:1360–7.
Honore PM, Joannes-Boyau O, Boer W, Collin V. High-volume hemofiltration in sepsis and SIRS: current concepts and future prospects. Blood Purif. 2009;28:1–11.
Perez-Fernandez X, Sabater-Riera J, Sileanu FE, Vazquez-Reveron J, Ballus-Noguera J, Cardenas-Campos P, Betbese-Roig A, Kellum JA. Clinical variables associated with poor outcome from sepsis-associated acute kidney injury and the relationship with timing of initiation of renal replacement therapy. J Crit Care. 2017;40:154–60.
Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, Schein RM, Sibbald WJ. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest. 1992;101:1644–55.
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G. International Sepsis Definitions C: 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Intensive Care Med. 2003;29:530–8.
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315:801–10.
Besen BA, Romano TG, Nassar AP Jr, Taniguchi LU, Azevedo LC, Mendes PV, Zampieri FG, Park M. Sepsis-3 definitions predict ICU mortality in a low-middle-income country. Ann Intensive Care. 2016;6:107.
Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–29.
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A, Bruining H, Reinhart CK, Suter PM, Thijs LG. The SOFA (Sepsis-related organ failure assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22:707–10.
Zhao H, Heard SO, Mullen MT, Crawford S, Goldberg RJ, Frendl G, Lilly CM. An evaluation of the diagnostic accuracy of the 1991 American College of Chest Physicians/Society of Critical Care Medicine and the 2001 Society of Critical Care Medicine/European Society of Intensive Care Medicine/American College of Chest Physicians/American Thoracic Society/Surgical Infection Society sepsis definition. Crit Care Med. 2012;40:1700–6.
KDIGO. Clinical practice guideline for acute kidney injury. Kidney Int Suppl. 2012;2:1–138.
Jansen TC, van Bommel J, Schoonderbeek FJ, Sleeswijk Visser SJ, van der Klooster JM, Lima AP, Willemsen SP, Bakker J, group Ls. Early lactate-guided therapy in intensive care unit patients: a multicenter, open-label, randomized controlled trial. Am J Respir Crit Care Med. 2010;182:752–61.
Mikkelsen ME, Miltiades AN, Gaieski DF, Goyal M, Fuchs BD, Shah CV, Bellamy SL, Christie JD. Serum lactate is associated with mortality in severe sepsis independent of organ failure and shock. Crit Care Med. 2009;37:1670–7.
Shankar-Hari M, Phillips GS, Levy ML, Seymour CW, Liu VX, Deutschman CS, Angus DC, Rubenfeld GD, Singer M, Sepsis Definitions Task F. Developing a new definition and assessing new clinical criteria for septic shock: for the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315:775–87.
Kawarazaki H, Uchino S, Tokuhira N, Ohnuma T, Namba Y, Katayama S, Toki N, Takeda K, Yasuda H, Izawa J, et al. Who may not benefit from continuous renal replacement therapy in acute kidney injury? Hemodial Int. 2013;17:624–32.
Passos RD, Ramos JG, Gobatto A, Mendonca EJ, Miranda EA, Dutra FR, Coelho MF, Pedroza AC, Batista PB, Dutra MM. Lactate clearance is associated with mortality in septic patients with acute kidney injury requiring continuous renal replacement therapy: a cohort study. Medicine (Baltimore). 2016;95:e5112.
Smith OM, Wald R, Adhikari NK, Pope K, Weir MA, Bagshaw SM. Standard versus accelerated initiation of renal replacement therapy in acute kidney injury (STARRT-AKI): study protocol for a randomized controlled trial. Trials. 2013;14:320.
Fujishima S, Gando S, Saitoh D, Mayumi T, Kushimoto S, Shiraishi S, Ogura H, Takuma K, Kotani J, Ikeda H, et al. A multicenter, prospective evaluation of quality of care and mortality in Japan based on the Surviving Sepsis Campaign guidelines. J Infect Chemother. 2014;20:115–20.
Acknowledgements
The authors thank all the nursing and medical staff (dialysis unit, ICU, and ED) for their patience and cooperation.
Availability of data and materials
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Author information
Authors and Affiliations
Contributions
MA collected and analyzed the data and wrote the manuscript. TY designed the study and helped to write the manuscript. MM, KW, EF, MN, HS, and SI helped to write the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Ethics Committee of the Tohoku University Graduate School of Medicine (2016-1-008).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Akiu, M., Yamamoto, T., Miyazaki, M. et al. Using Sepsis-3 criteria to predict prognosis of patients receiving continuous renal replacement therapy for community-acquired sepsis: a retrospective observational study. Ren Replace Ther 4, 37 (2018). https://doi.org/10.1186/s41100-018-0182-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41100-018-0182-7