Abstract
Infectious endocarditis (IE) with acute heart failure is a medical emergency. In particular, postoperative IE after aortic repair with an artificial vascular graft is a life-threatening matter. We present a case in which a mobile abscess appeared on the aortic valve annulus with an intra-cardiac shunt in the left ventricle (LV) to the right atrium (RA) after ascending aortic repair with aortic valve replacement (AVR) for acute type A aortic dissection. It was diagnosed with transesophageal echocardiography (TEE), which prompted further exploration.
Similar content being viewed by others
Background
Intra-cardiac shunts in the left ventricle (LV) to the right atrium (RA) are mostly congenital [1]. Similar acquired shunts are reported as follows: chest trauma, mitral and aortic valve replacement, or infectious endocarditis (IE) [2, 3]. In particular, intra-cardiac shunts with periannular abscesses related to IE have been reported in 14 % of patients after prosthetic valve replacement [2]. We present a case in which a mobile abscess appeared on the aortic valve annulus with an intra-cardiac shunt in the LV to the RA after ascending aortic repair with aortic valve replacement (AVR) for acute type A aortic dissection. It was diagnosed with transesophageal echocardiography (TEE), which prompted further exploration.
Case presentation
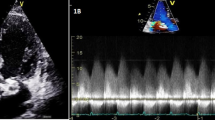
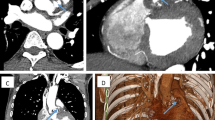
An 82-year-old woman underwent emergent aortic repair for acute type A aortic dissection. Intraoperative TEE showed aortic dissection in ascending to abdominal aorta with moderate aortic valve (AV) regurgitation. Neither regional wall motion abnormalities nor tricuspid and mitral valve abnormalities were shown on TEE. Under cardiopulmonary bypass (CPB), the aortic valve was replaced with a biological valve. After that, under circulatory arrest with selective brain perfusion, the ascending aorta was replaced with a vascular graft. The TEE after weaning from CPB showed no unusual findings. Tracheal extubation was performed on postoperative day (POD) 1. The postoperative course was comparatively stable and inflammatory reaction was not remarkable. We administrated an antibacterial drug, cefazolin of 2 g intraoperatively and 1 g/day postoperatively. On POD 9, however, she suddenly complained of both dyspnea and fever. C-reactive protein (CRP) was remarkably increased at 22 mg/dl. To prevent infection of the artificial vascular graft, we changed the antibacterial drug, vancomycin of 1.5 g/day and imipenem of 0.5 g/day. She was transferred to the intensive care unit (ICU) immediately. After emergency tracheal intubation, we inserted the pulmonary artery catheter (PAC) from the right internal jugular vein to evaluate cardiac function. Mixed venous blood oxygen saturation obtained from the PAC was revealed to be 90 %. As we suspected an intra-cardiac shunt, we firstly performed a transthoracic echocardiography (TTE). The two-dimensional TTE in the apical four-chamber view showed that a large vegetation seemed to be attached on the septal leaflet of the tricuspid valve (Fig. 1). Furthermore, TTE with color Doppler from a parasternal aortic valve short axis view showed abnormal flow in the RA (Fig. 2). To evaluate intra-cardiac appearance in detail, we performed a TEE examination, suspicious of an intra-cardiac shunt. The two-dimensional TEE from the modified four-chamber view clearly showed a large vegetation on the annulus of the aortic valve which protruded into the RA chamber (Fig. 3). Furthermore, the color Doppler TEE from the modified five-chamber view showed an intra-cardiac shunt from the LV to the RA through a subaortic ventricular septal fistula (Fig. 4). The three-dimensional TEE showed a structural connection between the aortic valve annulus and the attachment site of the vegetation (Fig. 5). After the intraoperative TEE found the abnormalities coincidently, we decided to perform an emergency surgical repair. We performed aortic annuloplasty with re-AVR and closure of the subaortic ventricular septal fistula using bio-pericardium. After repairing, the patient was somehow weaned from CPB with a high-dose inotrope. We confirmed by TEE that there was no pathologic flow associated with the fistula. Pathogenic bacteria were gram-positive coccus. In spite of all our medical efforts, on 30 POD, the patient died of multiple organ failure due to IE at the hospital.
Images of transesophageal echocardiography (TEE) in the mid-esophageal modified aortic valve short axis view. Left two-dimensional TEE, demonstrating the vegetation attached to the annulus of the aortic valve (arrow). Right color Doppler TEE, demonstrating the abnormal flow into the right atrium through the subaortic valve
Discussion
An acquired ventricle-atrium shunt has various etiologies: (1) after aortic and/or mitral valve replacement surgery, (2) infective endocarditis, and (3) chest trauma [4]. A schematic transverse section of a heart of the case is shown in Fig. 6; a membranous ventricular septum divides the LV chamber from the RA chamber [5]. Because a membranous ventricular septum is structured by thin connective tissue of the fibrous ring, an acquired LV-RA and/or RV shunt is likely to generate a membranous ventricular septum. The authors thought that the membranous ventricular septum was included in the aortic prosthetic valve structure line because of its proximity to the aortic root, resulting in IE and subsequently resulting in intra-cardiac shunt.
After the patient complained of the abnormality, the authors firstly inserted the PAC to evaluate the cardiac function. This revealed abnormal increased mixed venous blood oxygen saturation. Among many causes of increased mixed venous blood oxygen saturation, an intra-cardiac left to right shunt is one of the possible causes because of acute appearance of dyspnea. Although the patient unfortunately died of acute heart failure due to IE, decisive diagnosis without delay was required for performing adequate treatment. Although TTE revealed both the vegetation on the peri-aortic root and abnormal flow in the RA, the detailed site of the intra-cardiac shunt was difficult to detect. Because TEE depicts the subaortic structures clearly using an acoustic window from both of the LA and the RA, TEE depicts the structures better than TTE [6]. One of the tips for clearly depicting the detailed site of the LV-RA shunt is to adjust the aliasing velocity appropriately [7]. The authors adjusted the aliasing velocity at 30.8 cm/ms. Because pressure gradient between the LV and the RA decreases due to pressure overload at the RA, a relative slow velocity of shunt flow was predicted. Furthermore, three-dimensional TEE revealed the exact location of the vegetation attached to the aortic root structures. In this aspect, TEE examination in the ICU was a crucial diagnostic method to decide emergent surgical revision.
Conclusions
Although the patient died of acute heart failure due to infectious endocarditis, TEE information could be helpful for depicting the exact location of the fistula and for guiding the surgical procedure.
Abbreviations
- AV:
-
Aortic valve
- LA:
-
Left atrium
- LCC:
-
Left coronary cusp of the aortic valve
- LV:
-
Left ventricle
- NCC:
-
Noncoronary cusp of the aortic valve
- RA:
-
Right atrium
- RCC:
-
Right coronary cusp of the aortic valve
- RV:
-
Right ventricle
- TV:
-
Tricuspid valve
- vege:
-
Vegetation
References
Gerbode F, Hultgren H, Obsborn J. Syndrome of left ventricular-right atrial shunt: successful surgical repair of defect in five cases, with observation of bradycardia on closure. Ann Surg. 1958;148:433–46.
Sabik JF, Lytle BW, Bkackstone EH, Marullo AG, Pettersson GB, Cosgrove DM. Aortic root replacement with cryopreserved allograft for prosthetic valve endocarditis. Ann Thorac Surg. 2002;74:650–9.
Stechert MM, London MJ. Native aortic root endocarditis with invasion of the right outflow tract. Anesth Analg. 2010;110:36–8.
Silverman NA, Sethi GK, Scott SM. Acquired left ventricular-right atrial fistula following aortic valve replacement. Ann Thorac Surg. 1980;30:482–6.
Walmsley R, Watson H. The medial wall of the right atrium. Circulation. 1966;3:400–11.
Karalis DG, Bansal RC, Hauck AJ, Ross Jr JJ, Applegate PM, Jutzy KR, Mintz GS, Chandrasekaran K. Transesophageal echocardiographic recognition of subaortic complications in aortic valve endocarditis. Clinical and surgical implications. Circulation. 1992;86:353–62.
Stechert MM, Kellermeier JP. Aorto-atrial fistula: an important complication of aortic prosthetic valve endocarditis. Anesth Analg. 2007;105:332–3.
Acknowledgements
Authors’ contributions
TS was involved in patient care during the operation and prepared the manuscript. JN carried out the TEE study and substantially contributed to drafting the manuscript. MK drew the schema of the venous malformation. TM helped draft the manuscript. All authors read and approved the manuscript.
Authors’ information
TS is an Associate Professor at the Department of Anesthesiology, Osaka Medical College. JN is an Assistant Professor at the Department of Anesthesiology, Osaka Medical College. MK is an Assistant Professor at the Department of Anesthesiology, Osaka Medical College. TM is a Professor at the Department of Anesthesiology, Osaka Medical College.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Written informed consent for publication was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Sawai, T., Nakahira, J., Kitano, M. et al. A postoperative left ventricular-right atrial shunt due to infectious endocarditis after aortic repair with aortic valve replacement detected by transesophageal echocardiography. JA Clin Rep 2, 26 (2016). https://doi.org/10.1186/s40981-016-0052-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40981-016-0052-7