Abstract
Insulin replacement therapy is mostly used by patients with type 2 diabetes who become insulin deficient and have failed other therapeutic options. They comprise about a quarter of those with diabetes, endures the majority of the complications and consumes the majority of the resources. Adequate insulin replacement therapy can prevent complications and reduce expenses, as long as therapy goals are achieved and maintained. Sadly, these therapy goals are seldom achieved and outcomes have not improved for decades despite advances in pharmacotherapy and technology.
There is a growing recognition that the low success rate of insulin therapy results from intra-individual and inter-individual variations in insulin requirements. Total insulin requirements per day vary considerably between patients and constantly change without achieving a steady state. Thus, the key element in effective insulin therapy is unremitting and frequent dosage adjustments that can overcome those dynamics. In practice, insulin adjustments are done sporadically during outpatient clinic. Due to time constraints, providers are not able to deliver appropriate insulin dosage optimization.
The d-Nav® Insulin Guidance Service has been developed to provide appropriate insulinization in insulin users without increasing the burden on healthcare systems. It relies on dedicated clinicians and a spectrum of technological solutions. Patients are provided with a handheld device called d-Nav® which advises them what dose of insulin to administer during each injection and automatically adjust insulin dosage when needed. The d-Nav care specialists periodically follow-up with users through telephone calls and in-person consultations to bestow user confidence, correct usage errors, triage, and identify uncharacteristic clinical courses.
The following review provide details about the service and its clinical outcomes.
Similar content being viewed by others
Background
Index cases
Ms. R. is a 69-year-old woman with type 2 diabetes who has been treated with insulin since 2011. She is currently treated with basal-bolus insulin therapy that consists of once daily long-acting insulin analog and 3 rapid-acting insulin analog boluses with meals. Her diabetes control was poor for years, and in 4/2013 her A1c was 9.8%. Since 7/2014, her glycemic control has improved considerably with A1c levels ranging between 6.9% and 7.7%. She typically measures glucose 4 times/day before all meals and before bedtime. The frequency of her recorded hypoglycemia (glucose < 60 mg/dl) has been low at about 0.5 events per week without any nocturnal events. To achieve good glycemic control on insulin therapy, her insulin dosage has been adjusted 48 times over the past 28 weeks (see details in Fig. 1a). Notably, her total daily insulin was increased by about 15% for a period of 5 months before it decreased to the original daily insulin dosage. Most of her dosage changes occurred in her long-acting insulin dose and her dinner rapid-acting insulin dose, although other components have changed as well.
d-Nav downloads for the index patients. The upper graph denotes total daily insulin over time. The lower graph denotes each component of the patient dosage, including long-acting insulin analog before bed and rapid-acting insulin analog with breakfast, lunch and dinner. Correction factors are not shown. a) Ms. R.; b) Mr. E
Mr. E. is a 61-year-old man with type 2 diabetes who has been treated with insulin for 20 years. He is currently treated with basal-bolus insulin therapy. His diabetes control was poor for years and in 8/2015 his A1c was 9.1%. Since 11/2015, his glycemic control has improved considerably with A1c levels ranging between 5.5% to 6.6%. Lately, he has been measuring glucose about 23 times per week, regularly skipping pre-dinner tests. The frequency of his recorded hypoglycemia (glucose < 60 mg/dl) has been low at 0.2 events per week with a single nocturnal event for the past year. To achieve good glycemic control on insulin therapy, his insulin dosage has been adjusted 49 times over the past 32 weeks (see details in Fig. 1b). Between the beginning of 2017 and 6/2017, his insulin requirements and hence total daily insulin gradually increased by about 60% until it steadied in the beginning of 6/2017. Despite this relative stability in total daily insulin requirement, each component of his therapy continued to change. For example, dinner rapid-acting insulin bolus decreased by about 20%, breakfast increased by about 7% and long-acting insulin decreased by about 35%.
Ms. S. is a 62-year-old woman with type 2 diabetes who has been treated with insulin for 15 years. She is currently treated with basal-bolus insulin therapy. Her diabetes control was inadequate for years and in 2/2013 her A1c was 11.7%. Since 7/2013, her glycemic control has improved considerably with A1c levels ranging between 6.8% to 7.6%. Lately, she has been measuring glucose about 20 times per week, missing about a third of the times before lunch and bedtime. In 11/2015, her insulin requirements decreased by about 40% over a period of 2 weeks without warning or clear clinical reason. This reduction occurred mainly in her long-acting insulin dosage component, and to some extent in her lunch and breakfast boluses. After this noteworthy dosage reduction occurred, the frequency of her recorded hypoglycemia (glucose < 60 mg/dl) has been low at 0.7 events per week without any nocturnal events. To achieve good glycemic control on insulin therapy, her insulin dosage has been adjusted 50 times over the past 30 weeks (see details in Fig. 2c).
The above examples represent 3 typical patients with type 2 diabetes who use insulin. They have required considerable clinical effort in insulin titrations to improve and maintain appropriate diabetes control. In reality, most specialized providers are expected to provide care for hundreds of patients using insulin. Is it realistic to expect healthcare professionals to provide such a level of care to their patients?
In fact, the 3 examples are patients whose insulin therapy has been managed by the d-Nav® Insulin Guidance Service. The providers who referred these patients to the service had the ability to supervise the process but were not involved in the process of insulin dosage titration.
The “insulin paradox”
Patients with hormonal deficiencies are commonly seen in endocrinology practices. The endocrinologist is expected not only to diagnose the deficiency but also to fully replace it with adequate dosage of the appropriate hormone. Fundamentally, Inappropriate hormonal replacements such as hypothyroidism, adrenal insufficiency, or hypogonadism are considered as clinically unacceptable and poor quality-markers for the clinician. In contrast, replacement of the most common hormone deficiency, namely insulin deficiency (i.e., diabetes), is ineffective in the majority of the cases, even in the most reputable clinics and predominantly blamed on the patient.
Insulin replacement therapy is mostly used by patients with type 2 diabetes who become insulin deficient and have failed other therapeutic options (herein referred to as advanced diabetes). During the first decade with the disease, oral or non-insulin injectable medications that enhance endogenous insulin secretion and alleviate its resistance [1,2,3,4], are mostly suitable and effective in maintaining adequate glycemia. The clinical picture changes typically toward the second decade, during which many patients progress their insulin deficiency to the extent that insulin replacement therapy is warranted [5]. Initially, many patients can do well with simple regimens such as long-acting insulin only, yet over a period of a few years most require some level of fast acting insulin coverage to maintain appropriate glycemia [6]. About a quarter of the patients with type 2 diabetes use insulin. This cohort endures the majority of the complications and consumes the majority of the resources [7].
Although insulin as a hormone possesses multiple metabolic functions [8], the main therapeutic marker used to assess therapy adequacy is average glucose, or glycated hemoglobin (A1c). Studies have shown that adequate insulin replacement therapy prevents complications and premature death as long as therapy goals are achieved and maintained [9, 10]. Undoubtedly, supervision of statins and maintenance of normal blood pressure are vital [11]. The importance in reassuring appropriate insulin availability transpires beyond preventing glycemic damage [12]. Emerging data has shown that loss of insulin signaling in critical organs, worsens atherosclerosis and nephropathy in normoglycemic animals [13,14,15].
Most authorities recommend an A1c goal between 6.5% (and even lower if feasible) to 7.5% for the majority of patients [16,17,18]. Sadly, these therapy goals are seldom achieved and outcomes have not improved for decades despite advances in pharmacotherapy and technology. The average A1c in insulin users in the USA (as in Europe) is approximately 8.5% and a third of users continue to experience A1c at 9% or higher [19,20,21].
This phenomenon (also called the “insulin paradox”) is peculiar given the benefit of the drug and its safety profile. Insulin has been available for almost a century and exists in a variety of formulations with different pharmacokinetic and pharmacodynamic profiles. Compared to all other diabetes drugs, insulin does not have an upper dosage limit, and therefore, there is no level of hyperglycemia it cannot overcome. The only considerable side effect related to insulin therapy is hypoglycemia. It is the only known side effect that has been shown to be directly related to insulin and may be hazardous [22, 23]. Hypoglycemia has been experienced by most patients with insulin and it is the main limiting factor for effective insulin therapy. Severe hypoglycemia is the main aspect of hypoglycemia that has been feared by patients and clinicians alike. Tremendous amount of research has been made to understand and prevent these severe events [24, 25]. Intriguingly, in prospective clinical studies, for each individual who dies of severe hypoglycemia, hundreds die from other conditions of which many are related to diabetes and may potentially be preventable [26, 27].
Administration of insulin is largely painless, and the level of patient compliance is not different from compliance with other medications used to treat diabetes or other medical conditions such as hypertension [28,29,30]. It has been shown that about a quarter of patients with chronic medical conditions (including diabetes) do not follow providers’ recommendations [28]. Therefore, limited compliance doesn’t explain why most patients using insulin do not achieve their therapy goals.
There is a growing recognition that the “insulin paradox” results from intra-individual and inter-individual variations in insulin requirements. Normal pancreases secrete about 1 unit of insulin per kg body weight per day [31,32,33,34]. Endogenous pancreatic insulin secretion occurs in the portal system; whereas, the main organ responsive to the hormone is the liver. Under physiological settings, the liver retains about 85% of the digested glucose [31]. Once a patient loses their ability to secret enough insulin and requires insulin replacement therapy, the insulin is administered peripherally, outside the portal system. Due to peripheral metabolism of the hormone, mainly in the kidney, the required dosage needed to achieve similar levels of insulin in the portal system doubles [35]. This does not take into account cutaneous degradation of injected insulin that has been found to be considerable in some patients [36]. Endogenous insulin resources likely diminish gradually, as it may take a few years to build the required individual daily dosage once insulin therapy is initiated [6]. Although patients gain about 5 kg with insulin initiation, this weight gain plateaus within a year and therefore does not explain the gradual increase in insulin requirements that can last as long as 3 years [6]. In the majority of cases patients’ fluctuations in blood glucose and their tendency to develop hypoglycemia worsens after a few years [37]. Not surprisingly, in clinical studies that supervise treat-to-target insulin therapy in patients with type 2 diabetes, individual daily requirements average at 1.5–2 units per kilogram with a wide variance of distribution [38, 39]. Some patients use more than 500 units per day and occasionally utilize concentrated insulin formulations [40]. Importantly, higher dosage of insulin per day has not been shown to be associated with increased risk of hypoglycemia [41].
Insulin needs do not reach a steady state in patients with either type 1 or type 2 diabetes, as shown in the index cases in this review (Figs. 1 and 2). The need to constantly titrate insulin dosage in order to maintain euglycemia was demonstrated in clinical studies which supervised frequent insulin titrations both in the context of type 1 [42, 43] and type 2 diabetes [39, 44,45,46,47,48,49,50,51]. For most patients, insulin needs are unpredictable and dynamic, with requirements changing by 40% or even more (Fig. 3) [52, 54]. Unpredicted changes in insulin requirements expose patients to hypoglycemia or hyperglycemia [52,53,54].
Decline in insulin requirements over time (≥25% of prior dosage) in patients with type 2 diabetes using the d-Nav Insulin Guidance Service. a) Histogram depicting frequency of dosage reduction per year. In half of the cases, events occurred more than 0.6 times per year. b) Histogram depicting percentage of dosage reduction. In half of the cases, total daily insulin dosage decreased by more than 37.8%. c) Histogram depicting duration of decrease in insulin needs. In half of the cases, duration of the period exceeded 8.4 weeks. The graphs were reproduced from an already published information; Harper et al. [52]
Consequently, the key element in effective insulin therapy is unremitting and frequent dosage adjustments that can overcome those dynamics and enable maintenance of optimal glycemic control while minimizing occurrences of hypoglycemia [50, 53,54,55,56]. Judging from commonly used titration protocols, weekly titrations are preferable [39, 50, 51]. Simply stated, insulin is likely one the most dynamic drug existing in modern medicine. Not surprisingly, A1c goals have been achieved and maintained primarily in clinical trials that implement insulin dosage adjustment every few days-weeks [39, 44,45,46,47,48,49,50,51]. This beneficial effect lasts only as long as periodic adjustments are made by the medical staff, evidenced by deterioration of glycemic control within a few months after the studies end and insulin titrations became more sporadic [57, 58]. In practice, insulin adjustments are done sporadically during outpatient clinic visits every 3–6 months, which explains why the effectiveness of one of the earliest and most promising drugs in modern medicine has largely been poor. Patients are not typically blamed for inadequate blood pressure management or persistent elevated LDL, nor should they be blamed for inadequate insulin replacement therapy.
Insulin dosage titration is a teachable skill, yet it is time consuming and requires resources that are only available in well-funded trials. For illustration, it may take more than 15 min to contact a patient, deliberate, and convey adjustment in dosage. Even if a provider did nothing else but adjust weekly insulin dosage, he/she would only be able to support about 150 patients each. In the USA, there are about 7,000,000 patients who use insulin (www.cdc.gov/diabetes/statistics/meduse/fig2.htm). Thus, over 44,000 providers dedicated only to insulin dosage adjustments would be required to effectively support patients via means such as telemedicine. Currently, in the USA, there are about 15,000 providers who possess the required expertise [59] (https://www.diabeteseducator.org/about-aade), yet their time is already fully committed. Even every-other-week insulin dosage adjustments would overwhelm the healthcare system. Most importantly, the challenge is not in the collection and delivery of glucose data to the provider, for which a breadth of advanced technological solutions is available. It is not even in the deliberation process and medical decision-making. The main challenge is the need to close the loop; to deliver the recommendation to the patient in a way that he/she understands and can comfortably incorporate into daily life until the next adjustment is needed.
The prevalence of type 2 diabetes is on the rise; however, the availability of providers with expertise in insulin therapy is globally stable and low. As mentioned above, due to time constraints, providers are not able to deliver appropriate insulin dosage optimization. Accordingly, the only solution to the problem is one that provides frequent insulin dosage titrations in a way that the success of the therapy does not increase the burden on health care systems.
The d-Nav® insulin guidance service
Hygieia, Inc. was spun out of the University of Michigan and founded in 2008 by Israel Hodish, MD, PhD and Eran Bashan, PhD. The company has developed a scalable solution to the problem in the form of an integrated service that provides appropriate insulinization in insulin users. The service relies on dedicated clinicians (also called d-Nav Care Specialists) who utilize a spectrum of proprietary technological solutions. The integrated care service model follows existing models such as: dialysis services (e.g., www.davita.com), imaging services (e.g., www.flatworldsolutions.com), home infusion (e.g., www.infusionoptions.net/index.html), physical therapy, etc.
Patients referred to the service, are provided with a handheld device called d-Nav (stands for diabetes navigator) which advises them what dose of insulin to administer during each injection. This simple to use device is CE-marked and used by patients to monitor their glucose level before each injection (not yet approved by the FDA). In turn, it provides a recommended insulin dose. Following the logic of diabetes specialists and concordant with the gold standard guidelines for insulin management [60], the device assesses the patient’s response to its current insulin dosage by analyzing glucose patterns on a weekly basis (glucose readings from the on board sensor are stored in the device), then automatically adjusts the user’s insulin dosage [53, 54, 61, 62]. The device does not require any behavioral changes from the user. Adjustments are typically made weekly. Yet, if insulin requirements drop or hypoglycemia ensues, d-Nav makes immediate adjustments as often as needed, following the safety-first approach. This dynamic insulin therapy, first closes the gap between the initial prescribed total daily dose and the therapeutic one and then constantly evaluates each component of the therapy to fit the patient’s changing needs while preventing an increase in hypoglycemia. Since d-Nav provides insulin dose recommendations it is typically used before every insulin injection, i.e., from one to four times a day depending on the regimen. d-Nav adjusts most types of insulin regimens: A) once a day basal insulin; B) twice daily biphasic/premixed long- and short-acting insulin; and, C) intensive insulin therapy involving long-acting and fast-acting insulin with or without carbohydrate counting [62].
The d-Nav care specialists periodically follow-up with users through telephone calls and in-person consultations to bestow user confidence, correct usage errors, triage, and identify uncharacteristic clinical courses (example in Fig. 2c). The d-Nav care specialist team uses software solutions that analyze a device’s data to identify usage errors and recognize atypical clinical courses. For example, the software tools help to recognize if a patient requires a different insulin regimen, such as biphasic insulin therapy instead of basal insulin only [53, 63]. These software tools are available for providers during and between clinic visits. The service is linked to a wider healthcare system such that a patient’s data is always available to be reviewed by the patient’s physicians.
Clinical outcomes and safety
During the time this review was written, 1253 patients have been referred to the d-Nav service for an accumulated period of 1847 patient years. Most patients were referred with type 2 diabetes. Among active users, 339 have used the d-Nav service for more than 2 years. To date, patients’ average (±standard deviation) age is 60.8 ± 10.3 years, average duration of diabetes 15.8 ± 7.9 years and average duration of insulin usage 9.4 ± 7.5 years. Reduction in A1c is observed within 3 months of patients’ starting the d-Nav service. Most patients achieved and maintained glycemic goals for as long as they stayed with the service (Fig. 4). About 20% of the patients withdraw during the first year and less than 10% per year withdraw thereafter.
During the time this review was written, the frequency of severe hypoglycemia has been 2.2 per 100 patient years (in a cohort including patients with both type 2 and type 1 diabetes). For comparison, the expected frequency of severe hypoglycemia in insulin users with type 2 diabetes is 4–5 events per 100 patient years [25, 64]. In patients with type 1 diabetes, the frequency is higher [37].
Cost saving
Diabetes is one of the priciest conditions to manage and its demands are on the rise. As of 2012, the estimated US expenditure for diabetes care was $245 Billion [65]. Patients with advanced diabetes, who are more likely to require insulin therapy, consume the majority of the resources.
We believe that cost saving can be realized in 3 different areas: reductions in complications and hospitalizations; reductions in outpatient clinic costs; and, reductions in pharmaceutical expenses. While the first 2 categories may require a few years of improved patients’ glycemia in order to show cost savings, the last category may exert its savings within a few months.
It has been estimated that improved glycemic control can reduce cost, mainly due to reduction in hospital admissions [66] and enhancement in the healing of foot ulcers [67, 68]. The latter has been estimated to be prevalent in up to 25% of patients with diabetes [69]. A health-economic model evaluating the cost effectiveness of the d-Nav insulin guidance service in the United Kingdom projected savings of £1459 per patient over a 3-year period in all patients, and £4992 per patient over a 3-year period in high risk patients [68].
It has been suggested that about half of the insulin treated patients with type 2 diabetes tend to have monthly physician visits [70], likely due to high frequency of complications [67]. This can potentially be alleviated within the first few years of glycemic improvement.
Most authorities consider effective insulin therapy alongside metformin to be an adequate antidiabetic regimen [17, 60]. Yet, since most patients using insulin fail to achieve adequate glycemia, other anti-hyperglycemics are typically co-prescribed, some of which are branded and expensive. This polypharmacy increases costs and the risk for side effects, and may not achieve therapy goals [71, 72]. Although some prognostic benefit has been implicated with non-insulin anti-hyperglycemics [73,74,75,76], given the prognostic implications of successful insulin therapy [9], it is not entirely clear that other pharmacotherapy is needed if insulin therapy is effective. In a health economic evaluation, 217 patients were enrolled in to the d-Nav Insulin Guidance Service through a participating insurance group. In the 192 patients who completed the first 90 days of follow up, projected direct savings from medication elimination was estimated at $1736 per patient per year for all patients, and a projected saving of $6172 per patient per year for patient who used branded medications [77].
Competing solutions
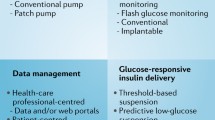
The d-Nav Insulin Guidance Service provides insulin management, yet it by no means competes with primary care or endocrine services. Those are absolutely critical for the holistic management of the patients who often experience comorbidities and complications. There are currently 4 categories of alternative approaches for the purpose of insulin therapy optimization: data delivery platforms, insulin dose calculators, decision support systems and closed loop insulin delivery devices.
Data delivery platforms
As digital communication technology is advancing; a multitude of data delivery systems are becoming available. They enable real-time delivery of glucose readings from patients’ glucose monitoring devices to their physicians (e.g., http://telcare.com, https://www.livongo.com, Accu-Check® [78]). With telemedicine, physicians and their staff can talk to patients face-to-face (e.g., https://evisit.com) to provide as many medications adjustments as they see fit. However, the rate-limiting factor is the large number of patients and the frequency of dosage adjustments that they need. Therefore, data delivery platforms are unlikely to provide a solution for insulin therapy.
Dose calculators
A breadth of titration guidelines has been used by studies who supervised insulin therapy and some were compared [39, 79]. The similarity in success rates and the minor differences between them [49], implies that a key element in their respective success is likely related to the frequency in which they were applied. Many of the titration guidelines have been transformed into commercially available tools or apps of which some are FDA approved (e.g., https://isageapp.com, http://voluntis.com, My Dose Coach from Sanofi-Aventis). Apps can be used by patients and can enable patients to titrate their own insulin dosage with their phone. However, these apps currently require the prescribing provider to select or design an appropriate titration algorithm for each patient and to assume full responsibility for the process of dose titration. Accordingly, they still significantly increase the burden of prescribing providers.
Decision support systems
The process of insulin dosage titration is better managed if expertise is available. On the other hand, the number of providers who are versed in managing insulin therapy is limited and not expected to grow significantly. Existing solutions including decision support for insulin titration that can be accessed by providers (e.g., www.insulinalgorithms.com, http://www.glytecsystems.com). However, such solutions still leave the burden of conveying the new dosage to the patients on the providers side. As mentioned above, we believe that any solution that increase providers’ workload is unlikely to be successful due to the limited available time of healthcare providers.
Closed loop insulin delivery devices or artificial pancreas
A great deal of research have been invested to develop a closed loop system combing an insulin pump and a continuous glucose monitor to form an “artificial pancreas [80].” These systems can continuously adjust ongoing insulin delivery based on prevailing glucose (www.medtronicdiabetes.com). The main impediments to this approach is complexity. Although insulin pumps were first available in the 1980s, they are currently used by about 50% of individuals with type 1 diabetes in the US [81] and by only about 1 million users globally [82]. Continuous glucose monitor devices (CGM) were introduced over a decade ago and are currently used by a few hundred-thousand patients (e.g., Dexcom about 200,000 globally in 2016, http://investor.shareholder.com/dexcom/releasedetail.cfm?ReleaseID=1014972).
Currently, the main users of these systems are patients with type 1 diabetes. This chronic condition is hard on patients and providers alike, but relatively uncommon. Among patients with type 1 diabetes, many have stopped using either devices due to their complexity and intense requirements. It is not clear that the 7,000,000 insulin users with type 2 diabetes in the US, who are generally older than the average insulin user with type 1 diabetes, would be willing to adopt the complexity of using an insulin pump and a CGM.
Proof of concept
Whatever solution used to improve the care of patients using insulin, enhanced clinical outcomes and reduced cost can only be realized if clinical goals are actually achieved. Hence, proof of concept is critical. It should demonstrate not only efficacy and safety in short-term clinical trials, but also durable effect in real-life over a long period of time.
Conclusion
Despite insulin’s long-term availability and still disappointing outcomes, we believe that achieving glycemic goals in insulin users with type 2 diabetes is within reach. When provided with frequent titration to optimize insulin dosage, the majority of patients using insulin could be maintained in a good quality of life for a longer time, while saving health care system resources.
Abbreviations
- A1c:
-
glycated hemoglobin
- CGM:
-
Continuous glucose monitor devices
References
Williams KJ, Wu X. Imbalanced insulin action in chronic over nutrition: clinical harm, molecular mechanisms, and a way forward. Atherosclerosis. 2016;247:225–82.
Kodama K, Tojjar D, Yamada S, Toda K, Patel CJ, Butte AJ. Ethnic differences in the relationship between insulin sensitivity and insulin response: a systematic review and meta-analysis. Diabetes Care. 2013;36(6):1789–96.
Bergman RN, Cobelli C. Minimal modeling, partition analysis, and the estimation of insulin sensitivity. Fed Proc. 1980;39(1):110–5.
Goodarzi MO, Langefeld CD, Xiang AH, et al. Insulin sensitivity and insulin clearance are heritable and have strong genetic correlation in Mexican Americans. Obesity (Silver Spring). 2014;22(4):1157–64.
UCFHR M. The Unitied States of Diabetes: Challenges and opportunities in the decade ahead. http://www.unitedhealthgroup.com/~/media/uhg/pdf/2010/unh-working-paper-5.ashx. 2010.
Holman RR, Farmer AJ, Davies MJ, et al. Three-year efficacy of complex insulin regimens in type 2 diabetes. N Engl J Med. 2009;361(18):1736–47.
McBrien KA, Manns BJ, Chui B, et al. Health care costs in people with diabetes and their association with glycemic control and kidney function. Diabetes Care. 2013;36(5):1172–80.
Wu X, Williams KJ. NOX4 pathway as a source of selective insulin resistance and responsiveness. Arterioscler Thromb Vasc Biol. 2012;32(5):1236–45.
Freemantle N, Danchin N, Calvi-Gries F, Vincent M, Home PD. Relationship of glycaemic control and hypoglycaemic episodes to 4-year cardiovascular outcomes in people with type 2 diabetes starting insulin. Diabetes Obes Metab. 2016;18(2):152–8.
Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359(15):1577–89.
Gaede P, Lund-Andersen H, Parving HH, Pedersen O. Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med. 2008;358(6):580–91.
Piarulli F, Sartore G, Lapolla A. Glyco-oxidation and cardiovascular complications in type 2 diabetes: a clinical update. Acta Diabetol. 2013;50(2):101–10.
Rask-Madsen C, Li Q, Freund B, et al. Loss of insulin signaling in vascular endothelial cells accelerates atherosclerosis in apolipoprotein E null mice. Cell Metab. 2010;11(5):379–89.
Han S, Liang CP, DeVries-Seimon T, et al. Macrophage insulin receptor deficiency increases ER stress-induced apoptosis and necrotic core formation in advanced atherosclerotic lesions. Cell Metab. 2006;3(4):257–66.
Welsh GI, Hale LJ, Eremina V, et al. Insulin signaling to the glomerular podocyte is critical for normal kidney function. Cell Metab. 2010;12(4):329–40.
American Diabetes A. 6. Glycemic Targets. Diabetes Care. 2017;40(Suppl 1):S48–56.
Garber AJ, Abrahamson MJ, Barzilay JI, et al. Consensus statement by the American Association of Clinical Endocrinologists and American College of endocrinology on the comprehensive type 2 diabetes management algorithm - 2017 executive summary. Endocr Pract. 2017;23(2):207–38.
NHS. Diabetes in adults quality standard (NICE quality standard). 2011.
Chen Y, Abbott S, Nguyen M, Grabner M, Quimbo R. Glycemic Control of Insulin Treated Patients Across the U.S.: Epidemiologic Analysis of a Commercially Insured Population. American Diabetes Association Meeting. 2013;2765-PO.
Hoerger TJ, Segel JE, Gregg EW, Saaddine JB. Is glycemic control improving in U.S. adults? Diabetes Care. 2008;31(1):81–6.
Selvin E, Parrinello CM, Daya N, Bergenstal RM. Trends in Insulin Use and Diabetes Control in the U.S.: 1988-1994 and 1999-2012. Diabetes Care. 2016;39(3):e33–5.
Gerstein HC, Bosch J, Dagenais GR, et al. Basal insulin and cardiovascular and other outcomes in dysglycemia. N Engl J Med. 2012;367(4):319–28.
Malmberg K, Norhammar A, Wedel H, Ryden L. Glycometabolic state at admission: important risk marker of mortality in conventionally treated patients with diabetes mellitus and acute myocardial infarction: long-term results from the diabetes and insulin-glucose infusion in acute myocardial infarction (DIGAMI) study. Circulation. 1999;99(20):2626–32.
Beck RW, Riddlesworth TD, Ruedy K, et al. Continuous glucose monitoring versus usual Care in Patients with Type 2 diabetes receiving multiple daily insulin injections: a randomized trial. Ann Intern Med. 2017;167(6):365–74.
Pathak RD, Schroeder EB, Seaquist ER, et al. Severe hypoglycemia requiring medical intervention in a large cohort of adults with diabetes receiving Care in U.S. integrated health care delivery systems: 2005-2011. Diabetes Care. 2016;39(3):363–70.
Gerstein HC, Miller ME, Byington RP, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358(24):2545–59.
Patel A, MacMahon S, Chalmers J, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008;358(24):2560–72.
Schmittdiel JA, Uratsu CS, Karter AJ, et al. Why don't diabetes patients achieve recommended risk factor targets? Poor adherence versus lack of treatment intensification. J Gen Intern Med. 2008;23(5):588–94.
Schifferdecker E, Schmidt K, Boehm BO, Schatz H. Long-term compliance of intensified insulin therapy. Diabetes Res Clin Pract. 1994;23(1):17–23.
Spoelstra JA, Stolk RP, Heerdink ER, et al. Refill compliance in type 2 diabetes mellitus: a predictor of switching to insulin therapy? Pharmacoepidemiol Drug Saf. 2003;12(2):121–7.
Waldhausl W, Bratusch-Marrain P, Gasic S, Korn A, Nowotny P. Insulin production rate following glucose ingestion estimated by splanchnic C-peptide output in normal man. Diabetologia. 1979;17(4):221–7.
Polonsky KS, Given BD, Van Cauter E. Twenty-four-hour profiles and pulsatile patterns of insulin secretion in normal and obese subjects. J Clin Invest. 1988;81(2):442–8.
Polonsky KS, Given BD, Hirsch L, et al. Quantitative study of insulin secretion and clearance in normal and obese subjects. J Clin Invest. 1988;81(2):435–41.
Fesinmeyer MD, Meigs JB, North KE, et al. Genetic variants associated with fasting glucose and insulin concentrations in an ethnically diverse population: results from the population architecture using genomics and epidemiology (PAGE) study. BMC Med Genet. 2013;14:98.
Ishida T, Chap Z, Chou J, et al. Effects of portal and peripheral venous insulin infusion on glucose production and utilization in depancreatized, conscious dogs. Diabetes. 1984;33(10):984–90.
Freidenberg GR, White N, Cataland S, O'Dorisio TM, Sotos JF, Santiago JV. Diabetes responsive to intravenous but not subcutaneous insulin: effectiveness of aprotinin. N Engl J Med. 1981;305(7):363–8.
Group UKHS. Risk of hypoglycaemia in types 1 and 2 diabetes: effects of treatment modalities and their duration. Diabetologia. 2007;50(6):1140–7.
Riddle MC, Bolli GB, Ziemen M, et al. New insulin glargine 300 units/mL versus glargine 100 units/mL in people with type 2 diabetes using basal and mealtime insulin: glucose control and hypoglycemia in a 6-month randomized controlled trial (EDITION 1). Diabetes Care. 2014;37(10):2755–62.
Bergenstal RM, Johnson M, Powers MA, et al. Adjust to target in type 2 diabetes: comparison of a simple algorithm with carbohydrate counting for adjustment of mealtime insulin glulisine. Diabetes Care. 2008;31(7):1305–10.
Reutrakul S, Wroblewski K, Brown RL. Clinical use of U-500 regular insulin: review and meta-analysis. J Diabetes Sci Technol. 2012;6(2):412–20.
Henderson JN, Allen KV, Deary IJ, Frier BM. Hypoglycaemia in insulin-treated type 2 diabetes: frequency, symptoms and impaired awareness. Diabet Med. 2003;20(12):1016–21.
Ruan Y, Thabit H, Leelarathna L, et al. Variability of insulin requirements over 12 weeks of closed-loop insulin delivery in adults with type 1 diabetes. Diabetes Care. 2016;39(5):830–2.
The_writing_team_of_the_DCCT. Effect of intensive therapy on residual beta-cell function in patients with type 1 diabetes in the diabetes control and complications trial. A randomized, controlled trial. The Diabetes Control and Complications Trial Research Group. Ann Intern Med. 1998;128(7):517–23.
Diabetes C. Complications trial research G, Nathan DM, et al. the effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329(14):977–86.
Holman RR, Thorne KI, Farmer AJ, et al. Addition of biphasic, prandial, or basal insulin to oral therapy in type 2 diabetes. N Engl J Med. 2007;357(17):1716–30.
Herman WH, Ilag LL, Johnson SL, et al. A clinical trial of continuous subcutaneous insulin infusion versus multiple daily injections in older adults with type 2 diabetes. Diabetes Care. 2005;28(7):1568–73.
Janka HU, Plewe G, Riddle MC, Kliebe-Frisch C, Schweitzer MA, Yki-Jarvinen H. Comparison of basal insulin added to oral agents versus twice-daily premixed insulin as initial insulin therapy for type 2 diabetes. Diabetes Care. 2005;28(2):254–9.
Buse JB, Wolffenbuttel BH, Herman WH, et al. DURAbility of basal versus lispro mix 75/25 insulin efficacy (DURABLE) trial 24-week results: safety and efficacy of insulin lispro mix 75/25 versus insulin glargine added to oral antihyperglycemic drugs in patients with type 2 diabetes. Diabetes Care. 2009;32(6):1007–13.
Strange P. Treat-to-target insulin titration algorithms when initiating long or intermediate acting insulin in type 2 diabetes. J Diabetes Sci Technol. 2007;1(4):540–8.
Riddle MC, Yki-Jarvinen H, Bolli GB, et al. One year sustained glycaemic control and less hypoglycaemia with new insulin glargine 300 U/mL compared with 100 U/mL in people with type 2 diabetes using basal + meal-time insulin (EDITION 1 12-month randomized trial including 6-month extension). Diabetes Obes Metab. 2015;
Bastyr EJ 3rd, Zhang S, Mou J, Hackett AP, Raymond SA, Chang AM. Performance of an electronic diary system for intensive insulin Management in Global Diabetes Clinical Trials. Diabetes Technol Ther. 2015;17(8):571–9.
Harper R, Donnelly R, Bi Y, Bashan E, Minhas R, Hodish I. Dynamics in insulin requirements and treatment safety. J Diabetes Complicat. 2016;30(7):1333–8.
Bashan E, Herman WH, Hodish I. Are glucose readings sufficient to adjust insulin dosage? Diabetes Technol Ther. 2011;13(1):85–92.
Rosenthal ES, Bashan E, Herman WH, Hodish I. The effort required to achieve and maintain optimal glycemic control. J Diabetes Complications. 2011;25(5):283–8.
Davidson MB. How our current medical care system fails people with diabetes: lack of timely, appropriate clinical decisions. Diabetes Care. 2009;32(2):370–2.
Hodish I. Can the current healthcare delivery model cope with advanced type 2 diabetes? J Diabetes Complicat. 2015;29(3):321–2.
The_writing_team_of_the_DCCT. Effect of intensive therapy on the microvascular complications of type 1 diabetes mellitus. JAMA. 2002;287(19):2563–9.
Hayward RA, Reaven PD, Wiitala WL, et al. Follow-up of glycemic control and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2015;372(23):2197–206.
Lu H, Holt JB, Cheng YJ, Zhang X, Onufrak S, Croft JB. Population-based geographic access to endocrinologists in the United States, 2012. BMC Health Serv Res. 2015;15:541.
American Diabetes A. 8. Pharmacologic approaches to glycemic treatment. Diabetes Care. 2017;40(Suppl 1):S64–74.
Bashan E, Hodish I. Frequent insulin dosage adjustments based on glucose readings alone are sufficient for a safe and effective therapy. J Diabetes Complicat. 2012;
Bergenstal RM, Bashan E, McShane M, Johnson M, Hodish I. Can a tool that automates insulin titration be a key to diabetes management? Diabetes Technol Ther. 2012;
Bashan E, Harper R, Bi Y, Hodish I. A novel approach to optimize glycaemic control in insulin users. BMJ Case Rep. 2015;2015.
Ganz ML, Wintfeld NS, Li Q, Lee YC, Gatt E, Huang JC. Severe hypoglycemia rates and associated costs among type 2 diabetics starting basal insulin therapy in the United States. Curr Med Res Opin. 2014;30(10):1991–2000.
American Diabetes A. Economic costs of diabetes in the U.S. in 2012. Diabetes Care. 2013;36(4):1033–46.
Menzin J, Langley-Hawthorne C, Friedman M, Boulanger L, Cavanaugh R. Potential short-term economic benefits of improved glycemic control: a managed care perspective. Diabetes Care. 2001;24(1):51–5.
Christman AL, Selvin E, Margolis DJ, Lazarus GS, Garza LA. Hemoglobin A1c predicts healing rate in diabetic wounds. J Invest Dermatol. 2011;131(10):2121–7.
Green W, Taylor M. Cost-effectiveness analysis of d-Nav for people with diabetes at high risk of neuropathic foot ulcers. Diabetes Ther. 2016;7(3):511–25.
Singh N, Armstrong DG, Lipsky BA. Preventing foot ulcers in patients with diabetes. JAMA. 2005;293(2):217–28.
Gamble JM, Chibrikov E, Twells LK, et al. Association of insulin dosage with mortality or major adverse cardiovascular events: a retrospective cohort study. Lancet Diabetes Endocrinol. 2017;5(1):43–52.
Fadini GP, Bonora BM, Avogaro A. SGLT2 inhibitors and diabetic ketoacidosis: data from the FDA adverse event reporting system. Diabetologia. 2017;60(8):1385–9.
Elashoff M, Matveyenko AV, Gier B, Elashoff R, Butler PC. Pancreatitis, pancreatic, and thyroid cancer with glucagon-like peptide-1-based therapies. Gastroenterology. 2011;141(1):150–6.
Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373(22):2117–28.
Neal B, Perkovic V, Mahaffey KW, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377(7):644–57.
Marso SP, Daniels GH, Brown-Frandsen K, et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2016;375(4):311–22.
Gaziano JM, Cincotta AH, Vinik A, Blonde L, Bohannon N, Scranton R. Effect of bromocriptine-QR (a quick-release formulation of bromocriptine mesylate) on major adverse cardiovascular events in type 2 diabetes subjects. J Am Heart Assoc. 2012;1(5):e002279.
Schneider JE, Parikh A, Stojanovic I. Impact of a Novel Insulin Management Service on Non-insulin Pharmaceutical Expenses. J Health Econ Outcomes Res. 2018;6(1)
Mora P, Buskirk A, Lyden M, Parkin CG, Borsa L, Petersen B. Use of a novel, remotely connected diabetes management system is associated with increased treatment satisfaction, reduced diabetes distress, and improved glycemic control in individuals with insulin-treated diabetes: first results from the personal diabetes management study. Diabetes Technol Ther. 2017;19(12):715–22.
Kennedy L, Herman WH, Strange P, Harris A. Impact of active versus usual algorithmic titration of basal insulin and point-of-care versus laboratory measurement of HbA1c on glycemic control in patients with type 2 diabetes: the glycemic optimization with algorithms and labs at point of care (GOAL A1C) trial. Diabetes Care. 2006;29(1):1–8.
Thabit H, Tauschmann M, Allen JM, et al. Home use of an artificial Beta cell in type 1 diabetes. N Engl J Med. 2015;373(22):2129–40.
Sherr JL, Hermann JM, Campbell F, et al. Use of insulin pump therapy in children and adolescents with type 1 diabetes and its impact on metabolic control: comparison of results from three large, transatlantic paediatric registries. Diabetologia. 2016;59(1):87–91.
Heinemann L, Fleming GA, Petrie JR, Holl RW, Bergenstal RM, Peters AL. Insulin pump risks and benefits: a clinical appraisal of pump safety standards, adverse event reporting and research needs. A joint statement of the European Association for the Study of diabetes and the American Diabetes Association diabetes technology working group. Diabetologia. 2015;58(5):862–70.
Acknowledgements
Not applicable.
Funding
Hygieia Inc.
Availability of data and materials
Not applicable.
Author information
Authors and Affiliations
Contributions
IH wrote the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
The three index patients have already signed the forms.
Competing interests
Israel Hodish is a co-founder of Hygieia Inc. and own stocks of the same. He is a co-inventor of patents related to the presented technology.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Hodish, I. Insulin therapy for type 2 diabetes – are we there yet? The d-Nav® story. Clin Diabetes Endocrinol 4, 8 (2018). https://doi.org/10.1186/s40842-018-0056-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40842-018-0056-5