Abstract
Background
Epithelioid sarcoma (ES) is a rare variant of soft tissue sarcoma. The proximal type of ES occurs in various locations. We present a resected case with proximal-type ES that occurred in the chest wall and discuss the relevant literature.
Case presentation
A 47-year-old woman was referred for a 6-month history of a right anterior chest mass with tenderness. Chest computed tomography showed an invasive chest wall mass with calcification surrounding the third rib. Aspiration biopsy cytology suggested malignancy. We performed wide resection, including the middle part of the pectoralis major muscle, the pectoralis minor muscle, the third and fourth ribs, and reconstruction of the chest wall, using a 2-mm polytetrafluoroethylene patch. Severe deformation of the chest wall was avoided. Postoperative physical therapy of the shoulder was effective for the continuous pain and weakness of the arm. She has remained alive for 1 year and 10 months without recurrence. Our literature review showed five previously reported cases of ES in the chest wall, and all of these were surgically resected. Two of these patients suffered from frequent local recurrence and died of disease.
Conclusions
ES in the chest wall is rare. Previous reports have indicated that surgical resection with tumor-free margins is essential for treatment. We performed complete resection of the tumor in our case, and a polytetrafluoroethylene patch was effective for reconstructing the deficit in the chest wall.
Similar content being viewed by others
Background
Epithelioid sarcoma (ES) was first described by Enzinger in 1970 [1]. ES represents less than 1.0% of all sarcomas [2]. Two subtypes of ES are currently recognized, including (i) the conventional/ classic type and (ii) the proximal type. The proximal type of ES occurs in various locations, such as truncal tissue, and the buttocks, thighs, head, and neck [3].
Case presentation
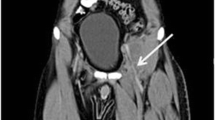
A 47-year-old woman was referred with a 6-month history of a right anterior chest mass. A physical examination showed a palpable firm mass with tenderness in the right anterior chest. Her routine laboratory investigations were within the biological reference range. Enhanced chest computed tomography (CT) showed a dumbbell-shaped mass with calcification, and its anterior portion was located under the pectoralis minor muscle and the posterior portion projected to the thoracic cavity (Fig. 1a). Chest magnetic resonance imaging (MRI) showed an invasive tumor, which was isointense on T1-weighted images and heterogeneously hyperintense on T2-weighted images (Fig. 1b, c). Aspiration biopsy cytology performed by a previous physician had shown malignancy, and no evidence of distant metastasis was found. Therefore, we planned surgical resection of the tumor with chest reconstruction. The patient was placed in the supine position. We first examined inside the thoracic cavity with thoracoscopy through the seventh intercostal space and found no lung invasion of the tumor. Wide resection, including the middle part of the pectoralis major muscle, the pectoralis minor muscle, and the third and fourth ribs, was performed. A negative margin of the tumor was identified by frozen sections. We used a 2-mm expanded polytetrafluoroethylene (ePTFE) patch (Gore Dualmesh; W.L. Gore & Associates, Flagstaff, AZ, USA) for chest wall reconstruction and covered it with spared skin and breast (Fig. 4). The operation time was 3 h and 33 min, and intraoperative blood loss was 64 ml.
The resected specimen was a firm tumor that surrounded the third rib (7.5 cm) (Fig. 2). Microscopically, the tumor cells showed an epithelioid appearance with cytoplasmic eosinophilia. The epithelioid cells had large vesicular nuclei and were arranged in sheet-like pattern. In some locations, scattered microcalcification was observed (Fig. 3a, b). Immunohistochemical staining showed expression of CD34 and cytokeratin (AE1/AE3) (Fig. 3c, d), but no expression of CD31, Sox10, Stat6, and integrase interactor 1 (INI1) in tumor cells. The diagnosis was proximal-type ES in the right chest wall. The French Fédération Nationale des Centres de Lutte Contre Le Cancer grading system was grade 2.
We started physical therapy on postoperative day 6 for local pain and limitation of shoulder motion. These symptoms improved by physical therapy, and she was discharged on postoperative day 18. Although weakness of the arm and chronic pain had been persistent, she could be reinstated in former factory work. We did not perform postoperative adjuvant chemotherapy or radiation therapy. She has remained alive for 1 year and 10 months without recurrence.
Discussion and conclusions
Primary chest wall sarcomas are rare in all malignant neoplasms. More than half of malignant tumors of the chest wall are metastatic lesions from distant organs or invasion from contiguous structures [4]. In a large series of patients with soft tissue sarcoma without metastases, tumors of only 3.8% of patients were located in the chest wall [5, 6]. The chest wall is also a well-known site of radiation-induced sarcomas [7].
For diagnosis of ES, any imaging system is not helpful because CT or MRI findings are nonspecific [8]. Proximal-type ES tends to affect the older population and has a worse prognosis than the conventional/classic type [9, 10]. Surgical resection with a tumor-free margin is essential in malignant soft tissue tumors, including ES, to prevent recurrence [2]. The effect of adjuvant therapy remains unclear [11, 12]. ES in the chest wall is rare. A literature review showed five cases of ES in the chest wall, including the present case (Table 1) [10, 13, 14]. All cases were reported from Asia, and none of them were from other areas [9, 15]. The age range of these cases was from 24 to 64 years old. There was one case with local metastasis, and none with distant metastasis at presentation. All of these cases underwent surgical resection. Two of five patients suffered from multiple times of local recurrence and finally died of disease. Although adjuvant therapy was performed in two cases, the effect was not clearly described. The present case was also followed up without any adjuvant therapy.
ES is defined as a malignant mesenchymal neoplasm that exhibits epithelioid cytomorphology and is predominantly an epithelioid phenotype. Pathologically, ES characteristically shows diffuse expression of epithelial membrane antigen and cytokeratins, which is similar to metastatic carcinoma. Therefore, ES (especially the proximal type) is often confused with metastatic carcinomas [3]. However, CD34 is expressed in half of ES cases and INI1 (also known as hSNF5, SMARCB1, and BAF47) is deficient in approximately 90% of ES cases in contrast to metastatic carcinoma [3, 13, 16, 17]. INI1-deficient tumors have also been reported, such as rhabdoid tumor of the kidney, renal medullary carcinoma, epithelioid malignant peripheral nerve sheath tumor, myoepithelial carcinoma, and extraskeletal myxoid chondrosarcoma [18]. In the present case, no expression of CD31, Sox10, and Stat6 contradict the diagnosis of angiogenic, neurogenic, or solitary fibrous tumor [19,20,21]. Therefore, these immunohistochemical stains were helpful for diagnosing ES.
The goals of reconstruction of the chest wall are adequate stability in respiration (prevention of paradoxical movement), water- and airtight closure, and an acceptable cosmetic appearance [22]. The use of alloplastic and/or xenogenic materials, as well as muscle flap repair, is well established [23,24,25,26]. However, Dingemann and colleagues reported one of eight pediatric cases suffered from rigid prosthetic material dislocation as a long-term complication in surgical reconstruction of the chest wall [27]. We used a 2-mm ePTFE patch for stabilization of the chest wall because it enabled us to reconstruct the chest wall safely and easily [27, 28]. Severe deformation was avoided by covering with the pared skin and breast (Fig. 4). However, loss of the middle part of the pectoralis major muscle induced continuous weakness in adduction, horizontal flexion, and internal rotation of the arm. Stretching and training of residual muscles may improve regional pain and prevent contracture of the shoulder.
In conclusion, we describe the clinical course and surgical treatment of a patient presenting with ES in the chest wall, which is a rare condition.
Abbreviations
- CT:
-
Computed tomography
- ePTFE:
-
Expanded polytetrafluoroethylene
- ES:
-
Epithelioid sarcoma
- INI1:
-
Integrase interactor 1
- MRI:
-
Magnetic resonance imaging
References
Enzinger FM. Epitheloid sarcoma: a sarcoma simulating a granuloma or a carcinoma. Cancer. 1970;26:1029–41.
Jawad MU, Extein J, Min ES, Scully SP. Prognostic factors for survival in patients with epithelioid sarcoma: 441 cases from the SEER database. Clin Orthop Relat Res. 2009;467:2939–48.
Guillou L, Wadden C, Coindre JM, Krausz T, Fletcher CD. “Proximal-type” epithelioid sarcoma, a distinctive aggressive neoplasm showing rhabdoid features: clinicopathologic, immunohistochemical, and ultrastructural study of a series. Am J Surg Pathol. 1997;21:130–46.
Pairolero PC, Arnold PG. Chest wall tumors: experience with 100 consecutive patients. J Thorac Cardiovasc Surg. 1985;90:367–72.
Torosian MH, Friedrich C, Godbold J, Hajdu SI, Brennan MF. Soft-tissue sarcoma: initial characteristics and prognostic factors in patients with and without metastatic disease. Semin Surg Oncol. 1988;4:13–9.
van Geel AN, Wouters MW, Lans TE, Schmitz PI, Verhoef C. Chest wall resection for adult soft tissue sarcomas and chondrosarcomas: analysis of prognostic factors. World J Surg. 2011;35:63–9.
Wiklund TA, Blomqvist CP, Raty J, Elomaa I, Rissanen P, Miettinen M. Postirradiation sarcoma: analysis of a nationwide cancer registry material. Cancer. 1991;68:524–31.
Tateishi U, Hasegawa T, Kusumoto M, Yokoyama R, Moriyama N. Radiologic manifestations of proximal-type epithelioid sarcoma of the soft tissues. AJR Am J Roentgenol. 2002;179:973–7.
Gasparini P, Facchinetti F, Boeri M, Lorenzetto E, Livio A, Gronchi A, et al. Prognostic determinants in epithelioid sarcoma. Eur J Cancer. 2011;47:287–95.
Rekhi B, Gorad BD, Chinoy RF. Clinicopathological features with outcomes of a series of conventional and proximal-type epithelioid sarcomas, diagnosed over a period of 10 years at a tertiary cancer hospital in India. Virchows Arch. 2008;453:141–53.
Wolf PS, Flum DR, Tanas MR, Rubin BP, Mann GN. Epithelioid sarcoma: the University of Washington experience. Am J Surg. 2008;196:407–12.
Asano N, Yoshida A, Ogura K, Kobayashi E, Susa M, Morioka H, et al. Prognostic value of relevant clinicopathologic variables in epithelioid sarcoma: a multi-institutional retrospective study of 44 patients. Ann Surg Oncol. 2015;22:2624–32.
Hasegawa T, Matsuno Y, Shimoda T, Umeda T, Yokoyama R, Hirohashi S. Proximal-type epithelioid sarcoma: a clinicopathologic study of 20 cases. Mod Pathol. 2001;14:655–63.
Aizawa K, Endo S, Yamamoto S, Saito N, Otani S, Hasegawa T, et al. Chest wall epithelioid sarcoma. Kyobu Geka. 2004;57:957–60.
Chbani L, Guillou L, Terrier P, Decouvelaere AV, Gregoire F, Terrier-Lacombe MJ, et al. Epithelioid sarcoma: a clinicopathologic and immunohistochemical analysis of 106 cases from the French sarcoma group. Am J Clin Pathol. 2009;131:222–7.
Fisher C. Epithelioid sarcoma of Enzinger. Adv Anat Pathol. 2006;13:114–21.
Hornick JL, Dal Cin P, Fletcher CD. Loss of INI1 expression is characteristic of both conventional and proximal-type epithelioid sarcoma. Am J Surg Pathol. 2009;33:542–50.
Hollmann TJ, Hornick JL. INI1-deficient tumors: diagnostic features and molecular genetics. Am J Surg Pathol. 2011;35:e47–63.
McKenney JK, Weiss SW, Folpe AL. CD31 expression in intratumoral macrophages: a potential diagnostic pitfall. Am J Surg Pathol. 2001;25:1167–73.
Nonaka D, Chiriboga L, Rubin BP. Sox10: a pan-schwannian and melanocytic marker. Am J Surg Pathol. 2008;32:1291–8.
Yoshida A, Tsuta K, Ohno M, Yoshida M, Narita Y, Kawai A, et al. STAT6 immunohistochemistry is helpful in the diagnosis of solitary fibrous tumors. Am J Surg Pathol. 2014;38:552–9.
Tukiainen E. Chest wall reconstruction after oncological resections. Scand J Surg. 2013;102:9–13.
Arnold PG, Pairolero PC. Chest-wall reconstruction: an account of 500 consecutive patients. Plast Reconstr Surg. 1996;98:804–10.
Gonfiotti A, Santini PF, Campanacci D, Innocenti M, Ferrarello S, Caldarella A, et al. Malignant primary chest-wall tumours: techniques of reconstruction and survival. Eur J Cardiothorac Surg. 2010;38:39–45.
Incarbone M, Pastorino U. Surgical treatment of chest wall tumors. World J Surg. 2001;25:218–30.
Kroll SS, Walsh G, Ryan B, King RC. Risks and benefits of using Marlex mesh in chest wall reconstruction. Ann Plast Surg. 1993;31:303–6.
Dingemann C, Linderkamp C, Weidemann J, Bataineh ZA, Ure B, Nustede R. Thoracic wall reconstruction for primary malignancies in children: short- and long-term results. Eur J Pediatr Surg. 2012;22:34–9.
Mansour KA, Thourani VH, Losken A, Reeves JG, Miller JI Jr, Carlson GW, et al. Chest wall resections and reconstruction: a 25-year experience. Ann Thorac Surg. 2002;73:1720–5.
Acknowledgements
We thank Ellen Knapp, Ph.D., from Edanz Group (http://www.edanzediting.com/) for editing a draft of this manuscript.
Availability of data and materials
The dataset supporting the conclusions of this article is included within the article.
Author information
Authors and Affiliations
Contributions
TS drafted the manuscript. TS and HS performed the operation, and HK followed up the patient. TW, YO, and EK diagnosed the disease as pathologists. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for the publication of this case report and related images.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Sakurai, T., Kusumoto, H., Wakasa, T. et al. Epithelioid sarcoma in the chest wall: a case report and literature review. surg case rep 4, 77 (2018). https://doi.org/10.1186/s40792-018-0483-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40792-018-0483-7