Abstract
Background
An atypical type A thymoma variant was newly added to the WHO classification of type A thymoma family in 2015.
Case presentation
A 72-year-old female was present a large round mass in the anterior mediastinum. The radiological examination led to a preoperative diagnosis of non-invasive thymoma. Tumor resection was undertaken via median sternotomy. Complete removal of the mediastinal tumor was achieved. Pathological examination revealed that the tumor cells were spindle- and oval-shaped with atypia. Immunohistochemical work-up revealed that the tumor was type A thymoma. On the basis of these findings, the tumor was finally diagnosed to be an atypical type A thymoma variant.
Conclusions
Preoperative diagnosis as atypical type A thymoma variant based on radiological examination is difficult. In case of atypical type A thymoma variant, a careful postoperative systemic follow-up should be done.
Similar content being viewed by others
Background
In general, type A thymoma is recognized as a benign tumor with excellent prognosis [1]. However, several authors have reported type A thymoma showing atypical features with postoperative tumor relapse [2–4]. On the basis of these reports, atypical type A thymoma variant was added to the type A thymoma family as a small subset of aggressive tumors [5, 6]. Here, we present the case of an atypical type A thymoma variant.
Case presentation
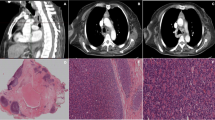
A 72-year-old female presented with a mediastinal mass that was incidentally detected on chest X-ray (Fig. 1a). Chest computed tomography (CT) revealed a large round mass of 7.7 cm in diameter in the anterior mediastinum. Contrast-enhanced CT (CE-CT) revealed that the mediastinal mass was not invading the surrounding organs (Fig. 1b). Fluorodeoxyglucose positron emission tomography (FDG-PET) showed mild uptake, with a maximum standardized uptake value (SUVmax) of 3.5 at the mediastinal mass (Fig. 1c). Abnormal uptake in other organs, which may lead to a suspicion of distant metastasis, was not detected. She did not present with myasthenia gravis or any other autoimmune diseases.
Chest X-ray showing an abnormal shadow in the mediastinum (a). Contrast-enhanced chest computed tomography showing a large round mass not invading the surrounding organs in the anterior mediastinum (b). Fluorodeoxyglucose positron emission tomography showing a mild hypermetabolic mass in the anterior mediastinum (c)
Our preoperative diagnosis was a non-invasive thymoma, and she underwent tumor resection via median sternotomy. The operative findings revealed that the tumor did not invade the surrounding organs, and we could easily dissect the tumor.
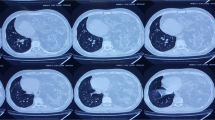
Pathological findings showed that the tumor was surrounded by a fibrous capsule (Fig. 2a), and its cells were spindle- and oval-shaped (Fig. 2b). A hemangiopericytoma-like vascular pattern was present. The tumor cells showed mild atypia, hypercellularity, and moderate mitotic activity (8–10 mitoses per 2 mm2). Necrosis was absent (Fig. 2c). A significant reticulin network was found around individual tumor cells. In the immunohistochemical work-up, the tumor cell was positive for AE1/AE3, p40, and CK5/6 and negative for CD5 and c-kit. CD20 expression was detected in some tumor cells (Fig. 3a). In the terminal deoxynucleotidyl transferase (TdT) staining, a few TdT + T cells were found in the tumor (Fig. 3b). The Ki-67 labeling index was 23.3 % (Fig. 3c). On the basis of these findings, the tumor was finally diagnosed to be an atypical type A thymoma variant.
Her postoperative course was uneventful, and she was discharged on foot 12 days after surgery. She is doing well without recurrence until last follow-up at 15 months after operation. We continue to conduct careful postoperative follow-up.
Discussion
An atypical type A thymoma variant was added to the WHO classification of type A thymoma family in 2015 [5] based on several reports about type A thymoma with oncological aggressive behavior and tumor relapses [2–4]. Pathological findings present the most specific feature of atypical type A thymoma. These are as follows: (1) mild to moderate nuclear atypia, (2) increase in mitotic activity, and (3) a scattered foci of necrosis. These findings are usually present in type B3 thymoma rather than the conventional type A thymoma. Vladislav and coworkers described that the frequency of type A thymoma with these aggressive behavior was 3.8 % (23/600 cases) [2]. In this case, the patient presented with mild atypia, hypercellularity, and high mitotic activity, which was 8–10 mitoses per 2 mm2. This distribution was denser than conventional type A thymoma where the count is usually <4 mitoses per 2 mm2.
On the other hand, specific finding of radiological examination was still unknown. CECT could show the possibility of tumor invasiveness to surrounding organ, but it would not reflect of morphological behavior. Recently, PET-CT has been known as a useful examination about thymic epithelial tumors, especially thymoma [7, 8]. Park and coworkers showed that significant relationship was observed between SUVmax and WHO classification, mean SUVmax in low-risk thymoma (A, AB, and B1) was 3.43, and high-risk thymoma (B2 and B3) was 4.42 [7]. However, in this case, SUVmax was 3.5; it might not be able to predict the morphological behavior. As these results, neither CECT nor PET-CT contributes preoperative definitive diagnosis of atypical type A thymoma variant.
Vladislav and coworkers showed that tumor relapse, including distant metastases, occurred in 43 % (10/23 patients) cases of type A thymoma showing atypical features [2]. This relapse rate is much higher than that of conventional type A thymoma.
The mean duration of time to metastases was 39.7 months (7–107 months). Of these 10 patients, lung metastasis was found in 5, and liver metastasis in 4. Regarding surgical margin and postoperative tumor metastasis, contrary to logic, development of metastatic disease was observed more frequently in the patients with negative surgical margin than positive or close (<1 mm) surgical margin. And they also described that only the presence of necrosis is a predictive factor of tumor relapse, including distant metastases, and no other factors such as the stage of diagnosis, tumor size, nuclear shape, nuclear variability, and mitotic activity correlate with tumor relapse. These suggested that postoperative follow-up about not only intrathoracic cavity but also extrathoracic cavity is essential.
Ki-67 is a well-known histological marker of proliferation used as an index of biological aggressiveness in various solid tumors. It has already been reported that Ki-67 labeling index (LI) correlates with the tumor aggressiveness in thymic epithelial neoplasm [9]. In that report, Ki-67 LI in type A thymoma was 0.3–11.0 % (median 3.0) and in thymic carcinoma was 12.2–43.3 % (median 23.2 %) [9]. Ki-67 LI in the present case was 23.3 %, which suggests that the aggressiveness of this tumor is similar to that of thymic carcinoma. The correlation between Ki-67 LI and tumor relapse in thymoma is not confirmed, but careful postoperative follow-up may be essential in atypical type A thymoma variant.
Conclusions
Here, we presented the case of an atypical type A thymoma variant. It is notable that radiological examination did not contribute to the definitive diagnosis of the atypical type A thymoma variant. When we encounter the case of atypical type A thymoma variant, careful postoperative systemic follow-up should be conducted.
Abbreviations
- CT:
-
Computed tomography
- TdT:
-
Terminal deoxynucleotidyl transferase
References
Okumura M, Ohta M, Tateyama H, Nakagawa K, Matsumura A, Maeda H, et al. The World Health Organization histologic classification system reflects the oncologic behavior of thymoma: a clinical study of 273 patients. Cancer. 2002;94:624–32.
Vladislav IT, Gokmen-Polar Y, Kesler KA, Loehrer Sr PJ, Badve S. The role of histology in predicting recurrence of type A thymomas: a clinicopathologic correlation of 23 cases. Mod Pathol. 2013;26:1059–64.
Nonaka D, Rosai J. Is there a spectrum of cytologic atypia in type a thymomas analogous to that seen in type B thymomas? A pilot study of 13 cases. Am J Surg Pathol. 2012;36:889–94.
Green AC, Marx A, Strobel P, Mason M, Lim E, Jordan S, et al. Type A and AB thymomas: histological features associated with increased stage. Histopathology. 2015;66:884–91.
Marx A, Strobel P, Badve SS, Chalabreysse L, Chan JK, Chen G, et al. ITMIG consensus statement on the use of the WHO histological classification of thymoma and thymic carcinoma: refined definitions, histological criteria, and reporting. J Thorac Oncol. 2014;9:596–611.
Marx A, Chan J, Coindre JM, Detterbeck F, Girard N, Harris NL, et al. The 2015 World Health Organization Classification of Tumors of the Thymus: continuity and changes. J Thorac Oncol. 2015;10:1383–95.
Park SY, Cho A, Bae MK, Lee CY, Kim DJ, Chung KY. Value of 18F-FDG PET/CT for predicting the World Health Organization malignant grade of thymic epithelial tumors: focused in volume-dependent parameters. Clin Nucl Med. 2016;41:15–20.
Fukumoto K, Taniguchi T, Ishikawa Y, Kawaguchi K, Fukui T, Kato K, et al. The utility of [18F]-fluorodeoxyglucose positron emission tomography-computed tomography in thymic epithelial tumours. Eur J Cardiothorac Surg. 2012;42:e152–6.
Roden AC, Yi ES, Jenkins SM, Donovan JL, Cassivi SD, Garces Y, et al. Diagnostic significance of cell kinetic parameters in World Health Organization type A and B3 thymomas and thymic carcinomas. Hum Pathol. 2015;46:17.25.
Acknowledgements
The authors would like to thank Enago (http://www.enago.jp) for the English language review.
Authors’ contributions
MH, SS, TT (Takuwa), and SH conceived and designed this study. SS, YT, and TT (Tsujimura) evaluated the pathological findings. MH and SS drafted the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Hashimoto, M., Shimizu, S., Takuwa, T. et al. A case of atypical type A thymoma variant. surg case rep 2, 116 (2016). https://doi.org/10.1186/s40792-016-0245-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40792-016-0245-3