Abstract
Background
Allergic and non-allergic rhinitis cause a lot of symptoms in everyday life. To decrease the burden more information of the preventable risk factors is needed. We assessed prevalence and risk factors for chronic nasal symptoms, exploring the effects of smoking, environmental tobacco smoke, exposure to occupational irritants, and their combinations.
Methods
In 2016, a postal survey was conducted among a random population sample of 8000 adults in Helsinki, Finland with a 50.5% response rate.
Results
Smoking was associated with a significant increase in occurrence of chronic rhinitis (longstanding nasal congestion or runny nose), but not with self-reported or physician diagnosed allergic rhinitis. The highest prevalence estimates of nasal symptoms, 55.1% for chronic rhinitis, 49.1% for nasal congestion, and 40.7% for runny nose, were found among smokers with occupational exposure to gases, fumes or dusts.
Besides active smoking, also exposure to environmental tobacco smoke combined with occupational exposure increased the risk of nasal symptoms.
Conclusions
Smoking, environmental tobacco smoke, and occupational irritants are significant risk factors for nasal symptoms with an additive pattern. The findings suggest that these factors should be systematically inquired in patients with nasal symptoms for appropriate preventive measures. (192 words).
Similar content being viewed by others
Background
It is estimated that 500 million people worldwide suffer from allergic rhinitis and in addition 200 million from non-allergic rhinitis [1, 2]]. These conditions render a considerable burden on both the patients and society in terms of life quality, disability and costs [3,4,5].
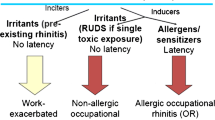
Allergic rhinitis is considered to be part of a systemic allergic condition often with comorbidities [6]. Rhinitis is a risk factor for asthma and eczema [7,8,9], and affects asthma and COPD control [10, 11]. Non-allergic rhinitis is a heterogenous group of conditions with variable etiology, e.g. hormonal, drug-induced, irritatative or idiopathic [2].
Rhinitis symptoms and chronic rhinosinusitis are significantly more common among smoking individuals than among non-smokers [12] . Smoking is also associated with the development of nasal polyposis [13]. The harmful effects of environmental tobacco smoke are also known from previous studies [14,15,16,17]. Occupational exposure to gases, dusts or fumes is a risk factor for rhinitis and sinusitis [16, 18] as well as for asthma and COPD [19], and eczema [9] . The combined effects of smoking, environmental tobacco smoke and occupational irritants on nasal symptoms have been less well estimated.
The FinEsS study is a Nordic joint project on the occurrence and risk factors of respiratory conditions in Finland, Estonia and Sweden. The present study assessed the prevalence of nasal symptoms and their association with smoking, environmental tobacco smoke, and occupational irritants in a population based cohort of 8000 Finnish adults.
Methods
Study population
In 2016, a postal questionnaire was mailed to a randomly selected sample of 8000 adults aged 20–69 years in 10-year age cohorts corresponding the gender and age distribution of the Finnish population. The genders were randomized separately. The sample was obtained from the Finnish National Population Registry (permission Dnro 254/410/15; 8.1.2015).
The invited individuals were given the possibility to respond either by mail or on the internet. Reminders were sent twice. The questionnaire was mailed in Finnish, Swedish or English, depending on the individuals` language. Of the 8000 selected, 17 refused to participate, 7 mailed an empty questionnaire and one had died. Of the 7975 invited 4026 (50.5%) responded. Twenty-eight questionnaires were excluded because they were not adequately fulfilled. For the present analysis, 510 individuals of the whole study population were excluded, because the questions about smoking habits, environmental tobacco smoke or exposure to gases, dusts or fumes at work were not answered. Thus, the final sample included 3488 individuals (1997, 57.3% women; 1491, 42.7% men).
The study was approved by the Coordinating Ethics Committee of Helsinki and Uusimaa Hospital District (200/13/03/00/2015).
Questionnaire
In Helsinki, previous postal surveys were conducted in 1996 and 2006 [17]. In 2016 we used the same questionnaire as in 1996 and 2006, but also additional questions about occupational and environmental exposure, nasal symptoms and allergy were included.
Questions and definitions
Chronic rhinitis. A positive answer to either having longstanding nasal congestion or runny nose or both.
Nasal congestion. Have you had longstanding nasal congestion?
Runny nose. Have you had longstanding rhinitis?
Self-reported allergic rhinitis. Do you have now or have you had previously allergic rhinitis (e.g. hay fever) or allergic eye symptoms?
Physician diagnosed allergic rhinitis. Have you been diagnosed by a doctor as having allergic rhinitis?
Smoker. Current smoker or having stopped smoking during the last year.
Ex-smoker. Stopped smoking more than 12 months prior to the study.
Non-smoker. Neither current smoker nor ex-smoker.
Exposure to tobacco smoke at work. Are you now or have you been heavily exposed to tobacco smoke at work?
Exposure to tobacco smoke at home. Are you now or have you been heavily exposed to tobacco smoke at home?
Exposure to environmental tobacco smoke. A positive answer to either exposure to tobacco smoke at work or at home.
Exposure to gases, dusts or fumes at work (occupational irritants). Are you now or have you been heavily exposed to gases, dusts or fumes at work?
Statistical analysis
All analyses were performed using SPSS version 23.0. Comparisons of proportions were tested with the Mann-Whitney U-test. p < 0.05 was regarded as statistically significant. Multiple logistic regression models were performed using smoking, exposure to tobacco smoke, and exposure to gases, dusts or fumes at work as risk factors for chronic nasal symptoms. Odds ratios (ORs) are presented with 95% confidence intervals (95%CI).
Results
The characteristics of the study population are shown in Table 1. In total, 26.6% of the responders were smokers, and 26% ex-smokers. Smoking was more common among younger individuals, 31.6% of the responders aged 20–29 years were smokers compared to 21.4% of those aged 60–69 years (p = 0.00). Exposure to gases, dusts or fumes was reported by 26.8% of the responders. Exposure to these irritants was slightly less frequent among younger individuals, 24.7% of those aged 20–29 years had been exposed compared to 28.6% of those aged 60–69 years (p = 0.068).
In the whole study sample, prevalence of chronic rhinitis (longstanding nasal congestion or runny nose) was 36.9%, of nasal congestion 29.8%, and of runny nose 27.9%. Smoking, environmental tobacco smoke and occupational irritants increased the prevalence in an additive manner (Fig. 1, Table 2). Smoking alone increased slightly the nasal symptoms, but was not associated with self-reported allergic rhinitis or physician-diagnosed allergic rhinitis. However, if a smoker was also exposed to occupational irritants, the prevalence of nasal symptoms was the highest. This additive effect of exposure to tobacco smoke and occupational irritants on chronic nasal symptoms remained when data were stratified by physician diagnosed allergic rhinitis (Table 2).
The prevalence of physician diagnosed allergic rhinitis was 27.9% in the whole study sample. It was reported by 26.9% of smokers, by 28.9% of ex-smokers and by 27.8% of non-smokers (p = 0.072). In men, environmental tobacco smoke or occupational irritants did not associate with physician diagnosed allergic rhinitis. Among women, however, 33.7% of those exposed to occupational irritants had physician diagnosed allergic rhinitis compared with 26.1% among the non-exposed (p = 0.032). Also in women, if occupational exposure was combined with environmental tobacco exposure the prevalence increased from 26.1% in non-exposed to 41.3% among exposed (p = 0.024).
The prevalence of longstanding nasal symptoms was high also in those responders who did not report physician diagnosed allergic rhinitis, as 30.8% of them reported chronic rhinitis, 25% nasal congestion, and 21.4% runny nose.
Results of the multiple logistic regression analysis are given in Table 3. Current smoking, without exposure to occupational irritants, yielded an odds ratio (OR) 1.22 (95%CI 1.00–1.49) for chronic rhinitis, and 1.26 (95%CI 1.01–1.56) for nasal congestion. Exposure to environmental tobacco smoke at home or at work did not, as such, increase the risk significantly in our model due to collinearity.
Occupational irritants were associated almost significantly with chronic rhinitis OR 1.28 (95%CI 0.97–1.69), with nasal congestion OR 1.20 (95%CI 0.90–1.60), and significantly with runny nose OR 1.49 (95%CI 1.11–1.99). The risk was not further increased, if the responders were also exposed to environmental tobacco smoke.
Current smoking combined with exposure to occupational irritants gave the highest risk estimates for nasal symptoms: OR 1.80 (95%CI 1.39–2.33) for chronic rhinitis, 1.82 (95%CI 1.40–2.35) for nasal congestion, and 1.68 (95%CI 1.28–2.19) for runny nose.
Discussion
Current smoking in combination with occupational exposure to gases, dusts or fumes resulted in increased occurrence of chronic nasal symptoms in both genders suggesting an additive harmful effect. Smoking alone was associated with chronic rhinitis and nasal congestion. Occupational irritants were associated with runny nose in both genders, and among women also with chronic rhinitis and nasal congestion. The risk increase is modest but obviously becomes significant in large populations.
The prevalence of longstanding nasal symptoms was high: 36.9% reported chronic rhinitis, 29.8% nasal congestion, and 27.9% runny nose. These symptoms were even more common than previously reported in Sweden [20, 21], but comparable to recent studies from Finland and Sweden [14, 18] .
We found exposure to occupational irritants to be a significant risk factor for chronic nasal symptoms, which is consistent with previous observations [20, 22, 23]. However, in a recent Swedish study occupational exposure to gases, dust or fumes was not associated with current rhinitis [18]. As their definition of current rhinitis included individuals with allergic rhinitis or chronic nasal symptoms, the results are not fully comparable.
Chronic nasal symptoms were more frequent among smokers and ex-smokers in the whole study group as found also in Sweden [20, 21] In the earlier report from FinEsS studies from 1997 to 2003, smoking was not associated with rhinitis symptoms [14]. In that report, however, the definition of rhinitis symptoms included also individuals with self-reported allergic rhinitis, which may explain the difference. In a study from Vietnam, using the same FinEsS-questionnaire, smoking was not a risk factor for nasal symptoms [24]. The results may be confounded by the much higher exposure to air pollution in Vietnam.
In our study, the prevalence of physician diagnosed allergic rhinitis was the same among non-smokers (27.1%) compared to current smokers (26.6%). Current smoking did not either increase the prevalence of nasal symptoms in those with physician diagnosed allergic rhinitis. However, smoking was associated with chronic nasal symptoms in the whole study sample, and increased the risk of nasal congestion significantly among those without physician diagnosed allergic rhinitis (p = 0.007). Our findings are in line with previous findings from U.S. [25] and suggest that the association between nasal symptoms and tobacco exposure might be independent of allergy.
The possible association between tobacco smoke and allergy has been studied previously. Smoking has been associated with an increased risk of allergic disease [26, 27] There is also evidence that tobacco smoke exposure would prevent from allergic sensitization [25, 28]. In a study from The Netherlands Vonk et al. [29] found that prenatal smoke exposure was associated with a decreased risk for the development of atopy. In another study from Canada Hancox et al. present that personal and parental smoking is associated with a lower risk of allergic sensitization in people with a family history of atopy [30]. In our study the prevalence of allergic rhinitis was independent of the smoking status.
Environmental tobacco smoke is known to be a modest risk factor for chronic nasal symptoms. Our results are in accordance with earlier findings [14] This association has also been confirmed in children [31]. We observed that environmental tobacco smoke both at home and at work slightly increased the occurrence of chronic nasal symptoms, which is in line with previous observations [32]. Environmental tobacco smoke has also predisposed to sinusitis [16].
In our study, exposure to environmental tobacco smoke at home did not increase the prevalence of chronic nasal symptoms in responders with or without physician diagnosed allergic rhinitis. Our findings are in line with previous results from Estonia; Larsson et al. found no significant association between ETS exposure at home and respiratory symptoms [33]. It is likely that our study group includes individuals that have been exposed to ETS at home in the past as smoking inside is not as common anymore as it has been in previous decades. Family members may also quit or reduce smoking inside the home more easily if one in their family develops respiratory symptoms. The lack of association might at least partly be explained by these mechanisms.
Responders who have been exposed to environmental tobacco smoke at work reported to have nasal congestion significantly more often in both groups. However, second hand smoke neither at home nor at work was a significant risk factor in our logistic regression model. Our results are in agreement with a study from Switzerland showing that second hand smoke was not independently associated with rhinitis symptoms [33].
We have found earlier, that smoking and occupational irritants have an additive effect on the incidence of COPD [19]. In the present study, we suggest that this additive exposure is also a risk factor for chronic nasal symptoms. The combined effect was seen in all age groups and whether or not allergic rhinitis was present.
Non-allergic rhinitis is divided into several subgroups. Half of the patients with non-allergic rhinitis does not have a clear etiology for their symptoms (e.g. occupational, hormonal, drug-induced) and are sometimes classified as having an idiopathic rhinitis [2]. Our results suggest that these symptoms are, at least partly, explained by smoking, environmental tobacco smoke or exposure to occupational irritants. These risks are preventable by anti-smoking efforts and reduction of occupational exposure.
Study limitations
The observations are derived from a questionnaire survey based on a random population sample with a participation rate of 51%. With two reminders, we find the representativeness satisfactory. Participation rates have decreased by time in epidemiological studies which is a general problem. The response rate has been about the same in other epidemiological studies as in our study, for example 55% in Copenhagen City Heart Study. [34] and 53% in a Swedish follow up study on the prevalence of asthma [35].
The FinEsS questionnaire has been used in several other studies. Some new questions of nasal symptoms were added, which improved the detection of the nasal conditions. An obvious limitation of the present survey is the lack of individual clinical evaluation of the responders. We did not take into account ambient air pollution, which could potentially confound our findings. However, in Finland air pollution is minimal and well controlled, even in cities.
Conclusions
In conclusion, smoking, environmental tobacco smoke and occupational exposure to gases, dusts or fumes increase significantly the prevalence of chronic nasal symptoms both in men and women. The combined effect of smoking and occupational exposure was the most marked risk factor yielding the highest prevalence estimates. Thus, anti-smoking efforts at population level and measures to stop smoking and irritant exposure at work may reduce nasal symptoms. The campaign for Tobacco-Free Finland at 2030 [30] and the Healthy Workplaces Campaign [31] have been launched and should be strongly promoted.
References
Bousquet J, Khaltaev N, Cruz AA, Denburg J, Fokkens WJ, Togias A, et al. Allergic rhinitis and its impact on asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA(2)LEN and AllerGen). Allergy. 2008 Apr;63(Suppl 86):8–160.
Hellings PW, Klimek L, Cingi C, Agache I, Akdis C, Bachert C, et al. Non-allergic rhinitis: position paper of the European academy of Allergology and clinical immunology. Allergy. 2017 May 5;
Bousquet PJ, Demoly P, Devillier P, Mesbah K, Bousquet J. Impact of allergic rhinitis symptoms on quality of life in primary care. Int Arch Allergy Immunol. 2013;160(4):393–400.
Axelsson M, Lindberg A, Kainu A, Ronmark E, Jansson SA. Respiratory symptoms increase health care consumption and affect everyday life - a cross-sectional population-based study from Finland, Estonia, and Sweden. Eur Clin Respir J. 2016 May 27;3:31024.
Smith P, Price D, Harvey R, Carney AS, Kritikos V, Bosnic-Anticevich SZ, et al. Medication-related costs of rhinitis in Australia: a NostraData cross-sectional study of pharmacy purchases. J Asthma Allergy. 2017 May 9;10:153–61.
Cingi C, Gevaert P, Mosges R, Rondon C, Hox V, Rudenko M, et al. Multi-morbidities of allergic rhinitis in adults: European Academy of Allergy and Clinical Immunology Task Force Report. Clin Transl Allergy 2017 Jun 1;7:17–017-0153-z. eCollection 2017.
Pallasaho P, Juusela M, Lindqvist A, Sovijarvi A, Lundback B, Ronmark E. Allergic rhinoconjunctivitis doubles the risk for incident asthma--results from a population study in Helsinki, Finland. Respir Med. 2011 Oct;105(10):1449–56.
Shaaban R, Zureik M, Soussan D, Neukirch C, Heinrich J, Sunyer J, et al. Rhinitis and onset of asthma: a longitudinal population-based study. Lancet. 2008 Sep 20;372(9643):1049–57.
Ronmark EP, Ekerljung L, Lotvall J, Wennergren G, Ronmark E, Toren K, et al. Eczema among adults: prevalence, risk factors and relation to airway diseases. Results from a large-scale population survey in Sweden. Br J Dermatol. 2012 Jun;166(6):1301–8.
Pongracic JA, Krouse RZ, Babineau DC, Zoratti EM, Cohen RT, Wood RA, et al. Distinguishing characteristics of difficult-to-control asthma in inner-city children and adolescents. J Allergy Clin Immunol. 2016 Oct;138(4):1030–41.
Kim JK, Lee SH, Lee BH, Lee CY. Kim do J, min KH, et al. factors associated with exacerbation in mild- to-moderate COPD patients. Int J Chron Obstruct Pulmon Dis. 2016 Jun 16;11:1327–33.
Lee WH, Hong SN, Kim HJ, Ahn S, Rhee CS, Lee CH, et al. Effects of cigarette smoking on rhinologic diseases: Korean National Health and nutrition examination survey 2008-2011. Int Forum Allergy Rhinol. 2015 Oct;5(10):937–43.
Houser SM, Keen KJ. The role of allergy and smoking in chronic rhinosinusitis and polyposis. Laryngoscope. 2008 Sep;118(9):1521–7.
Pallasaho P, Kainu A, Juusela M, Meren M, Sovijarvi A. High prevalence of rhinitis symptoms without allergic sensitization in Estonia and Finland. Eur Clin Respir J 2015 Apr 8;2:https://doi.org/10.3402/ecrj.v2.25401. eCollection 2015.
Hung HJ, Chen CY, Wang SL, Wu TN, Lee CH, Cheng SY. Environmental tobacco smoke: relationship to early pregnancy discomforts. Am J Health Behav. 2017 May 1;41(3):320–8.
Hur K, Liang J, Lin SY. The role of secondhand smoke in sinusitis: a systematic review. Int Forum Allergy Rhinol. 2014 Jan;4(1):22–8.
White AJ, D'Aloisio AA, Nichols HB, DeRoo LA, Sandler DP. Breast cancer and exposure to tobacco smoke during potential windows of susceptibility. Cancer Causes Control. 2017 May 18;
Ronmark EP, Ekerljung L, Mincheva R, Sjolander S, Hagstad S, Wennergren G, et al. Different risk factor patterns for adult asthma, rhinitis and eczema: results from West Sweden Asthma Study. Clin Transl Allergy 2016 Aug 4;6:28–016–0112-0. eCollection 2016.
Pallasaho P, Kainu A, Sovijarvi A, Lindqvist A, Piirila PL. Combined effect of smoking and occupational exposure to dusts, gases or fumes on the incidence of COPD. COPD 2014 Feb;11(1):88–95.
Eriksson J, Ekerljung L, Pullerits T, Holmberg K, Ronmark E, Lotvall J, et al. Prevalence of chronic nasal symptoms in West Sweden: risk factors and relation to self-reported allergic rhinitis and lower respiratory symptoms. Int Arch Allergy Immunol. 2011;154(2):155–63.
Eriksson J, Ekerljung L, Ronmark E, Dahlen B, Ahlstedt S, Dahlen SE, et al. Update of prevalence of self-reported allergic rhinitis and chronic nasal symptoms among adults in Sweden. Clin Respir J. 2012 Jul;6(3):159–68.
Thilsing T, Rasmussen J, Lange B, Kjeldsen AD, Al-Kalemji A, Baelum J. Chronic rhinosinusitis and occupational risk factors among 20- to 75-year-old Danes-a GA(2) LEN-based study. Am J Ind Med. 2012 Nov;55(11):1037–43.
Schyllert C, Ronmark E, Andersson M, Hedlund U, Lundback B, Hedman L, et al. Occupational exposure to chemicals drives the increased risk of asthma and rhinitis observed for exposure to vapours, gas, dust and fumes: a cross-sectional population-based study. Occup Environ Med. 2016 Oct;73(10):663–9.
Lam HT, Van T Tng N, Ekerljung L, Ronmark E, Lundback B. Allergic rhinitis in northern vietnam: increased risk of urban living according to a large population survey. Clin Transl Allergy 2011 Aug 11;1(1):7-7022-1-7.
Shargorodsky J, Garcia-Esquinas E, Navas-Acien A, Lin SY. Allergic sensitization, rhinitis, and tobacco smoke exposure in U.S. children and adolescents. Int Forum Allergy Rhinol. 2015 Jun;5(6):471–6.
Noakes PS, Hale J, Thomas R, Lane C, Devadason SG, Prescott SL. Maternal smoking is associated with impaired neonatal toll-like-receptor-mediated immune responses. Eur Respir J. 2006 Oct;28(4):721–9.
Kim SY, Sim S, Choi HG. Atopic dermatitis is associated with active and passive cigarette smoking in adolescents. PLoS One. 2017 Nov 1;12(11):e0187453.
Bottema RW, Reijmerink NE, Kerkhof M, Koppelman GH, Stelma FF, Gerritsen J, et al. Interleukin 13, CD14, pet and tobacco smoke influence atopy in three Dutch cohorts: the allergenic study. Eur Respir J. 2008 Sep;32(3):593–602.
Vonk JM, Boezen HM, Postma DS, Schouten JP, van Aalderen WM, Boersma ER. Perinatal risk factors for bronchial hyperresponsiveness and atopy after a follow-up of 20 years. J Allergy Clin Immunol. 2004 Aug;114(2):270–6.
Hancox RJ, Welch D, Poulton R, Taylor DR, McLachlan CR, Greene JM, et al. Cigarette smoking and allergic sensitization: a 32-year population-based cohort study. J Allergy Clin Immunol. 2008 Jan;121(1):38–42.e3.
Faraldo-Garcia A, Lopez-Silvarrey A, Pertega S, Cruz MJ, Sampedro M, Sanchez-Lastres J, et al. Cross-sectional study about impact of parental smoking on rhinitis symptoms in children. Clin Otolaryngol. 2017 Mar 17;
Tammemagi CM, Davis RM, Benninger MS, Holm AL, Krajenta R. Secondhand smoke as a potential cause of chronic rhinosinusitis: a case-control study. Arch Otolaryngol Head Neck Surg. 2010 Apr;136(4):327–34.
Larsson ML, Loit HM, Meren M, Polluste J, Magnusson A, Larsson K, et al. Passive smoking and respiratory symptoms in the FinEsS study. Eur Respir J. 2003 Apr;21(4):672–6.
Browatzki A, Ulrik CS, Lange P. Prevalence and severity of self-reported asthma in young adults, 1976-2004. Eur Respir J. 2009 Nov;34(5):1046–51.
Backman H, Raisanen P, Hedman L, Stridsman C, Andersson M, Lindberg A, et al. Increased prevalence of allergic asthma from 1996 to 2006 and further to 2016-results from three population surveys. Clin Exp Allergy. 2017 Nov;47(11):1426–35.
Acknowledgements
Not applicable.
Ethical approval and consent to participate
The study was approved by the Coordinating Ethics Committee of Helsinki and Uusimaa Hospital District (200/13/03/00/2015). All participants consented.
Funding
This study was supported by a special governmental subsidy for health sciences research (Helsinki University Central Hospital project grants TYH 2013354 and Y2017SK004), Nummela Sanatorium Foundation, Research Foundation for Pulmonary Diseases (Heli), Väinö and Laina Kivi Foundation, and Ida Montin Foundation.
Availability of data and materials
The datasets supporting the conclusions of this article are included within the article.
Author information
Authors and Affiliations
Contributions
All authors were involved in the discussions and contributed to writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Consent for publication
Not applicable.
Competing interests
The authors declare that they do not have any competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Hisinger-Mölkänen, H., Piirilä, P., Haahtela, T. et al. Smoking, environmental tobacco smoke and occupational irritants increase the risk of chronic rhinitis. World Allergy Organ J 11, 6 (2018). https://doi.org/10.1186/s40413-018-0184-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40413-018-0184-5