Abstract
Background
Primary intracranial osteosarcoma is a extremely rare disease entity. We describe a case of primary intracerebral osteosarcoma in an adult brain.
Case description
A patient who presented with a 1-week history of headaches, and MRI examination was performed. The immunohistochemical diagnosis confirmed primary intracerebral osteosarcoma. The patient was treated with a surgical resection of the tumor.
Conclusion
Primary osteosarcomas occurring in the brain are extremely rare. The MRI images did not provide a specific pretreatment diagnosis, and the histopathology was the mainstay in establishing the diagnosis.
Similar content being viewed by others
Background
Osteosarcoma is a highly malignant neoplasm of bone and can occur anywhere in the body, but is most commonly found in the long bones. Extraskeletal osteosarcomas occurring in tissues other than bone, are rare. Primary intracranial osteosarcomas are extremely rare, developing from leptomeningeal sheats around blood vessels or from vessel walls themselves (Ashkan et al. 1998). Here we report a case of primary intracerebral osteosarcoma.
Case report
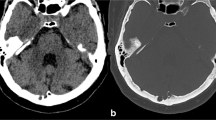
A 54-year-old female was referred to our institution with a 1-week history of headaches. Her past medical history was unremarkable. Magnetic resonance imaging (MRI) revealed a large, partially necrotic and calcified tumor in the parenchyma of the left frontal lobe with marked surrounding edema and mass effect on midline structures, but without any dural attachment. The tumor appeared hypointense on non-contrast T1-weighted images (Fig. 1a) and iso-to hyperintense on T2-weighted images (Fig. 1b). The enhancement of the tumor was irregular and most prominent at its periphery (Fig. 1c–e). The preoperative clinical diagnosis was meningioma or calcified glial tumor. She underwent incomplete resection of the tumor and histopathologic examination revealed a malignant mesenchymal neoplasm displaying a poorly differentiated spindle cells with interspersed eosinophilic osteoid production, calcification intimately associated with the malignant cells, and localized new bone formation (Fig. 1f). Immunohistochemistry was negative for epithelial membrane antigen (EMA), glial fibrillary acidic protein (GFAP), CD34, desmin and neurone specific enolase (NSE) but positive for vimentin (Fig. 1g), P53 (Fig. 1h), osteopontin (Fig. 1i) and osteonectin (Fig. 1j). Antisera against the proliferation marker Ki-67 revealed very variable immunoreactions (80%). Given the microscopic appearance a histopathologic diagnosis of primary intracerebral osteosarcoma was made.
a, b MRI brain show a large, necrotic and calcified tumor (white arrow) in the parenchyma of the left frontal lobe with marked surrounding edema and mass effect on midline structures. The tumor appeared hypointense on non-contrast T1-weighted images and iso-to hyperintense on T2-weighted images. c–e The enhancement of the tumor was irregular and most prominent at its periphery. f Histopathology shows the tumor contained many neoplastic osteoid production (black arrow) and some calcifications (red arrow) (hematoxylin and eosin, original magnification, ×200), and tumor cells strongly expressing Vimentin (g), P53 (h),osteopontin (i) and osteonectin (j). (immunohistochemistry, original magnification, ×200, black arrow)
Extraskeletal osteosarcoma is rare and is defined as a malignant mesenchymal neoplasm that produces osteoid as well as bone or chondroid material and is located in the soft tissue without any bony attachment (Chung and Enzinger 1987). Primary intracranial osteosarcoma most often represent intracranial invasion from a tumor arising from the skull (Salvati et al. 1993), and meningeal osteosarcomas which arise from the mesenchymal components of the meninges are also reported (Dagcinar et al. 2008). However, primary intracerebral osteosarcoma is rare with very few reported cases in literature.
Literature search
We performed a PubMed search for all cases of primary intracerebral osteosarcoma up to September 2016. Cases were analyzed for basic demographic features including age, sex, chief complaint, location, treatment, and clinical outcome (Table 1).
Conclusion
Primary intracerebral osteosarcoma is an extremely rare tumor and its radiological appearance is not pathognomonic. Despite their rarity, primary intracerebral osteosarcomas should be included in the differential diagnosis, especially for other tumors such as meningioma and calcified glial tumor, and histopathology is the mainstay in establishing the diagnosis.
Abbreviations
- MRI:
-
magnetic resonance imaging
- EMA:
-
epithelial membrane antigen
- GFAP:
-
glial fibrillary acidic protein
- NSE:
-
neurone specific enolase
References
Ashkan K, Pollock J, D’Arrigo C, Kitchen D (1998) Intracranial osteosarcomas: report of four cases and review of the literature. J Neurooncol 40(1):87–96
Bauman GS, Wara WM, Ciricillo SF, Davis RL, Zoger S, Edwads MSB (1997) Primary intracerebral osteosarcoma: a case report. J Neurooncol 32(3):209–213
Chung EB, Enzinger FM (1987) Extraskeletal osteosarcoma. Cancer 60(5):1132–1142
Dagcinar A, Bayrakli F, Yapicier O, Ozek M (2008) Primary meningeal osteosarcoma of the brain during childhood: case report. J Neurosurg Pediatr. 1(4):325–329
Hettmer S, Fleischhack G, Hasan C, Kral T, Meyer B, Bode U (2002) Intracanial manifestation of osteosarcoma. Pediatr Hematol Oncol 19(5):347–354
Jacques S, Freshwater DB, Shelden CH (1976) Primary osteogenic sarcoma of the brain. J Neurosurg 44(1):92–95
Ohara N, Hayashi K, Shinohara C, Kamitani M, Furuta T, Yoshino T, Takahashi K, Taguchi K, Akagi T (1994) Primary osteosarcoma of the cerebrum with immunohistochemical and ultrasructural studies: report of a case. Acta Neuopathol 88(4):384–388
Reznik M, Lenelle J (1991) Primary intracerebral osteosarcoma. Cancer 68(4):793–797
Salvati M, Ciappetta P, Raco A (1993) Osteosarcomas of the skull: clinical remarks on 19 cases. Cancer 71(7):2210–2216
Sipos EP, Tamargo RJ, Epstein JI, North RB (1997) Primary intracerebral small-cell osteosarcoma in an adolescent girl: report of a case. J Neurooncol 32(2):169–174
Authors’ contributions
XLZ: designed the study and drafted the manuscript. SPC and JLT: acquired, analysed and interpreted the data. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Patient consent
Signed consent is available from the patient for this report publication.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Chen, SP., Tang, JL. & Zhu, XL. Primary intracerebral osteosarcoma: a rare case report and review. SpringerPlus 5, 1997 (2016). https://doi.org/10.1186/s40064-016-3678-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40064-016-3678-z