Abstract
Background
Efforts to understand and address the causes of place-based health disparities have focused primarily on understanding the social determinants of health on a large geographic level, such as the region, state, or county. However, there is a growing need to assess and understand how place-based characteristics at smaller geographic areas relate to of local place-based neighborhood characteristics on population health. Therefore, the objective of this study was to evaluate the magnitude of the associations between social determinants of health and life expectancy (LE) and related measures on the community level.
Methods
LE at birth (LE0), remaining LE at age 65 (LE65), and age-specific mortality rates (ASMR) were calculated from mortality data (2009–2011) collected by the Rhode Island Department of Health (RIDoH) using abridged life table methods for each RI city/town. The city/town-specific LE and ASMR were linked to data collected by the US Census, RIDoH, the Federal Bureau of Investigation, and other databases that include information about multiple social, environmental, and demographic determinants of health. Bivariate correlations between city/town-level LE0, LE65, and ASMR and social determinants: demographics, household composition, income and poverty, education, environment, food insecurity, crime, transportation, and rural-urban status were examined.
Results
LE0 (range: 75.9–83.3 years) was strongly associated with the percent of the population with a graduate/professional degree (r = 0.687, p < 0.001), violent crime rate (r = − 0.598, p < 0.001), and per capita income (r = 0.553, p < 0.001). Similar results were observed for ASMR: ASMR was associated with the percent of the population with a graduate/professional degree (r = − 0.596, p < 0.001), violent crime rate (r = 0.450, p = 0.005), and per capita income (r = − 0.533, p < 0.001). The associations between LE65 and social determinants were more attenuated. Of note, none of the measures (LE0, LE65, or ASMR) were associated with any of the race/ethnicity variables.
Conclusions
There are several important place-based characteristics associated with mortality (LE and ASMR) among RI cities/towns. Additionally, some communities had unexpectedly high LE and low ASMR, despite poor social indicators.
Similar content being viewed by others
Background
Place matters for population health. Evidence suggests that one’s place of residence plays a substantial and important role in determining individual health status in the United States and many other nations [1]. As a result, health inequities based on geography occur [2,3,4,5]. A number of studies have demonstrated health disparities by geography, examples include, but are not limited to, cancer [6], physical activity and obesity [7], health care quality and access [8,9,10], and cancer screening [11, 12].
Research to understand and address the causes of place-based health disparities has focused primarily on social determinants of health within a large geographic level, such as a region, state, or county [13]. Recently, however, there has been growing interest in drilling down to the local level and assessing health disparities at smaller geographic areas to evaluate the influence of place-based neighborhood and municipality characteristics [14]. The reason for this is that policies, demographic characteristics, and economic conditions at the local level potentially affect availability and quality of resources, community development, and economic opportunities [15]. Increasingly, research suggests that understanding how social determinants, including education, wealth, crime, environmental factors, housing, and numerous others at a smaller geographic area influence population health is critical to ameliorating health inequities occurring within these small geographic areas [16,17,18,19,20,21,22,23].
Life expectancy is a widely used summary measure of population health, and represents the average lifespan based on current death rates, and provides a global picture of population health [24]. In the United States, differences in LE by place are substantial and have increased over time [25]. Consider, for example, the US county with the lowest LE (Oglala Lakota County in South Dakota, 66.8 years) and the county with the highest LE (Summit County in Colorado, 86.8 years), a difference of 20 years. That stark difference in LE between these two counties located only 400 miles from one another is nearly equivalent to the difference in LE between women in Ethiopia (66.7 years) and Japan (86.8).
There is a growing body of research highlighting the utility of employing LE to document health inequities, and to determine and understand what health disparities also occur at fine geographic levels that are smaller units than county, state, or nation. These include the city or town (municipality), census tract, and neighborhood levels [26,27,28,29,30]. Differences at this more granular level may be masked when LE or other health-related metrics are calculated on a larger level, such as the county or state level [31, 32], geographic levels on which most spatial research has been conducted. Nonetheless, no studies to date have quantified LE at a fine geographic level (e.g. sub-county) for a large geographic area and systematically assessed potential associations between LE and social determinants within that fine geographic level. To that end, the aims of this exploratory study were to: (1.) estimate LE and related measures of population health in all Rhode Island (RI) municipalities; (2.) compare and contrast life expectancy LE at birth with other population health measures; and (3.) explore associations between key measures of population health (LE and mortality) and an array of social determinants.
Methods
Outcome measures: life expectancy and age-standardized mortality rates
LE for this study was calculated using methods adapted from the CDC’s methodology for calculating LE on a small geographic scale [33]. All de-identified death records for 2009, 2010, and 2011 from the RI Department of Health Center for Vital Records were geocoded to each of the 39 RI cities and towns (“municipality”). All deaths during this same time period were summed to create tables of total deaths in each RI municipality by 5-year age groups. These data were then paired with detailed population counts for each of the 5-year age groups for all RI municipalities and then used to obtain age-specific death rates using population data from the 2010 US Decennial Census. From this information, LE at birth (LE0) and at age 65 (LE65) were calculated with associated standard errors and 95% confidence intervals for each municipality. In total, 13% of the 663 cells had zero deaths. In these cases, the RI age-specific death rate was used to calculate LE. As a result, the calculated LEs for these municipalities may be slightly biased toward the mean LE [34, 35]. Age-standardized mortality rates (ASMRs) for each RI municipality also were derived using the calculated age-specific death rates with the same substitution method applied for cells with zero death counts.
Exposure measures: social determinants of health
A set of 55 social determinants of health and related measures was obtained from the most recent (2010) US Decennial Census and American Community Survey and other sources (e.g. RI Kids Count, Youth Risk Behavior Surveillance System, the Federal Bureau of Investigation) to create a database of 89 social determinants that included measures of education, income and wealth, poverty, green space, crime, demographics, housing, household composition, rural/urban characteristics, environment, food insecurity, land use, transportation, commuting, and age distribution. A detailed list of all examined determinants is provided in the Results section.
Data analysis
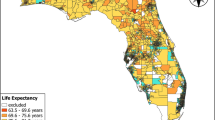
Descriptive statistics were obtained for the three main summary measures of population health—LE at birth (LE0), LE at age 65, (LE65), and ASMR—and for each of the social determinants for each RI municipality, including means, standard deviations, minima, and maxima for all continuous and discrete variables, and frequency distributions for all categorical variables. Shapefiles for all municipalities were obtained and downloaded for use in mapping from the RI Geographic Information System [36]. Using geographic information systems (GIS) software, detailed choropleth maps of LE0, LE65, ASMR, and the examined social determinants for all RI municipalities were created.
Pearson and Spearman correlations were used to estimate the bivariate associations between the three outcome measures (LE0, LE65, and ASMR) and the examined social determinants. Rank order variables (e.g. school ranking, etc.) had identical Pearson and Spearman correlation values. Linear regression models were constructed to estimate associations and determine which factors are predictive of LE0, LE65, and ASMR using forward stepwise methods. Model assumptions for linear regression were checked for the statistical “best” model for each of the outcome measures. Resultant associations between the health outcomes (LE0, LE65, and ASMR) and the social determinants were then examined using meta-regression [37], employing permutation tests and bootstrapping to adjust the p-values for multiplicity [38]. Although there is possible geo-spatial autocorrelation, for purposes of modeling, each municipality was considered to be independent of the other municipalities [39]. IBM SPSS version 26 (Armonk, NY) and SAS version 9.4 (Cary, NC) were used for all data management and analysis. ArcGIS version 10.1 (Redlands, WA) was used for all mapping and geospatial analysis. SPSS and Microsoft Excel were used for graphing. Statistical significance was set at alpha < 0.05. This study was approved by the University of Rhode Island Institutional Review Board (protocol #1259971–2).
Results
Information on LE0, LE65, and ASMR for all RI municipalities can be found in Table 1. The average LE0 in RI was 79.92 years, with a standard deviation of 1.60. There was a 7.3-year difference between the town with the highest LE0 (Barrington, 83.13 years) and the lowest LE0 (Woonsocket, 75.85 years). Barrington also had the lowest ASMR (722.0 per 100,000), while the highest ASMR (1127.6 per 100,000) was found in Woonsocket. New Shoreham had the highest LE65 (21.92 years), while Richmond had the lowest LE65 (17.59 years).
Descriptive statistics for the major population health measures and examined social determinants can be found in Table 2. There was a wide range of values for several demographic variables, including population density, which ranged from 91 people per square mile in Foster to 16,172 people per square mile in Central Falls. Likewise, the percent of population that is Hispanic/Latino/a ranged from 0.3% in Glocester to 87.4% in Central Falls. Descriptive statistics for crime, economic, education, environmental and recreational, and retirement-based measures are also provided in Table 2. The economic variable “median home value”, cannot exceed the maximum of $1000,000 as measured by the US Census, found in New Shoreham, so the actual value in New Shoreham may be higher. The percent of family households headed by females alone ranged from 3.4% in New Shoreham to 21.7% in Providence. Maps for key population health measures and social determinants are located in the Supplementary Material).
The bivariate associations among the three primary measures of population health (LE0, LE65, and ASMR) were moderate to strong; the Pearson correlation between LE0 and LE65 was 0.578 (p < 0.001). There were several outliers of note (see Fig. 1, Panel A), including New Shoreham and Richmond. Although New Shoreham has the second-lowest LE0 in RI (76.8 years), it had the highest LE65 (21.9 years). Richmond had the lowest LE65 (17.6 years), and was ranked 33rd highest out of all 39 RI municipalities for LE0 (78.4 years). The Pearson correlation between LE0 and ASMR was − 0.872 (p < 0.001), and between LE65 and ASMR was − 0.863 (p < 0.001) (Fig. 1, Panels B and C).
Correlations between LE0, LE65, and ASMR and each of the exposure measures are shown in Fig. 2. In this figure, the measures are categorical, and ranked within category by magnitude and direction of correlation (smallest to largest) between the measure and LE0. For the demographic variables, the percent of family households headed by a single female was negatively associated with LE0 (r = − 0.332, p = 0.039), and positively correlated with the percent of population aged 65+ (r = 0.330, p = 0.040), the percent of family households headed by a married couple (r = 0.394, p = 0.013), and the Black/White Index of Dissimilarity, a measure of segregation (r = 0.675, p < 0.001). For example, a city or town with an index of dissimilarity of 0.55 indicates that 55% of White people would need to move to another census tract within that city or town to distribute Whites and Blacks evenly across all census tracts in that city or town. Similar results, but in the opposite direction, were found for these measures and ASMR. People per housing unit was negatively correlated with LE65 (r = − 0.439, p = 0.005). LE0 and ASMR were significantly associated with the six examined education variables, but the associations between LE65 and ASMR were only significant for the percent of adults with at least a bachelor’s degree (r = 0.512, p = 0.001) and with a graduate degree (r = 0.467, p = 0.003).
Pearson correlation between LE0, LE65, and ASMR and each of the social determinants examined. The magnitude and direction of the correlation is shown by color: red and pink indicate positive correlations, while blue indicates negative correlations. The darker the color, the stronger the correlation. Boldface = significant at p < 0.05
The results of this analysis examining economic factors were more varied. Percent unemployed was strongly and negatively associated with LE0 (r = − 0.572, p < 0.001), but was not significantly associated with either LE65 or ASMR. Percent of population on public assistance, median rent, and median household income were all significantly associated with LE0, LE65, and ASMR. Poverty rate was associated with LE0 (r = − 0.389, p = 0.014) and ASMR (r = 0.418, p = 0.008), but not with LE65 (r = − 0.245, p = 0.113). LE65, however, was significantly associated with median home value (r = 0.527, p = 0.001) while LE0 and ASMR were not. LE0 and ASMR were significantly associated with all of the seven examined individual crime rate measures, as well as overall violent crime and property crime rates, while LE65 was not significantly associated with any of these measures.
Fast food and convenience stores per square mile was significantly associated with decreased LE0 (r = − 0.348, p = 0.030), while the percent of total area of the city or town comprised of water (lakes, ponds, bay, ocean, etc.) was significantly associated with both LE65 (r = 0.525, p = 0.001) and ASMR (r = − 0.356, p = 0.026), but not with LE0 (r = − 0.251, p = 0.122). Mean per capita retirement income was the only retirement measure that was significantly associated with LE0, LE65, and ASMR.
For LE0, three social determinants remained significant in the forward stepwise linear regression model (Table 3): increasing percentages of adults with at least a bachelor’s degree (beta = 0.11, p < 0.001), percentage of the population aged 65+ (beta = 0.23, p = 0.001), and percentage of multigenerational households (beta = 0.43, p = 0.024) were all significant predictors of LE0, and remained so in the meta-regression models. Only median rent (beta = 0.003, p = 0.001) remained significantly associated with LE65, but was not significant in the meta-regression model. Median rent also was significantly associated with ASMR, and with five other social determinants: percentage of adults with a graduate degree, percentage of population aged 65+, average commuting time (minutes), percentage foreign born, and percentage on public assistance, although percent 65+, commuting time, and median rent were not significant in the meta-regression models. The model parameters explained 70.9, 28.7, and 78.2% of the variability in LE0, LE65, and ASMR, respectively.
Discussion
Education and crime were consistent correlates of both LE0 and ASMR, although several other social determinants were associated with these measures. Social determinants, in general, explained a substantial portion of the variability in LE0 and ASMR, but explained substantially less variability in LE65. Study findings validate previous research showing that population health is associated with a variety of social determinants, including education, wealth, crime, and household composition. Although the same age-specific mortality rates were used to calculate LE0 and ASMR, there are some discrepancies between the two measures of population health, as there also were differences with respect to the social determinants that were closely correlated with each determinant. These differences could be due to slight differences in how these variables are calculated. LE0 is affected more by variability in mortality rates at younger ages than ASMR, which weights age-specific mortality based on the standard used, in this case, the RI state population. However, correlations between LE0 and ASMR were stronger than correlations between LE0 and LE65 and between ASMR and LE65.
At the national level, the association between education and LE0 is well documented, with several studies finding substantial differences between those with higher education compared to those with less education [25, 40, 41]. Furthermore, one study found that temporal improvements in LE occurred only in more educated population subgroups [42]. The present study’s correlational findings extends prior research by highlighting that the education-LE association exists at a finer geographic level. Many other findings from the present study corroborate prior research on other social determinants, including food insecurity [43], income and wealth [44,45,46], and crime [47, 48]. Conversely, study findings suggest that, although there were no associations between any of the demographic characteristics (e.g. percent Black, percent Asian, etc.) and LE or ASMR, higher levels of Black-White isolation as measured by the Black-White Index of Dissimilarity, were associated with higher LE0 and lower ASMR. This finding counters the preponderance of evidence suggesting that higher residential segregation worsens population health [49,50,51,52]. The differences identified in this study may be due to the estimation of LE and ASMR, which was for the entire population of each RI city or town, irrespective of race/ethnicity. Similar methods have been used in prior studies [53, 54]. Nonetheless, further research is needed to understand the possible reasons for this contradictory finding.
The interpretation of study results should be considered in the context of several important limitations. First, these are cross-sectional data; therefore causality cannot be inferred. Second, study results refer to mortality data from the 2009–2011 timeframe. Patterns of mortality, as well as social determinants, may have changed somewhat between this timeframe and the present. Although more recent mortality data are available from the Rhode Island Department of Health, data from this period were used to correspond closest to the timing of the 2010 US Census data, which was one of the main data sources of social determinants. The 2010 Census is the most recent decennial census, and population data used from the decennial census is more accurate than more recent inter-censal estimates [55]. Third, although 55 social determinants were examined in this correlational analysis, the list of examined social determinants and population health measures (LE0, LE65, and ASMR) are not exhaustive. There are numerous other summary measures of population health, including specific health conditions, healthcare services utilization, and general health indices, that can be assessed, if available, in future studies. Next, spatial autocorrelation is another potential limitation. In this study, each RI municipality was considered to be an independent observation. However, municipalities that are close together may have more in common with each other than those that are further apart. Similarly, study findings are valid only on the geographic level analyzed in this analysis—the municipality level. Findings may be different if analyzed on smaller (e.g. census tract, block group) or larger (e.g. county) scales. Furthermore, small-area LE calculations are subject to substantial error [30, 56, 57]. In the calculation of LE and ASMR, many of the cells (13%) used contained a death count of zero. The state age-specific death rates were used as substitutes for cells with zero death count, which would bias the results toward the mean. Minor changes in the number of deaths, particularly for cities and towns with low death counts in the younger ages, can have a sizeable impact on the calculation of LE and ASMR. Lastly, the small sample size of RI Island municipalities (n = 39) limits the overall power of the study, especially with respect to multivariable analyses.
Despite these limitations, this exploratory study has several important strengths. This study is among the first to explore municipal-level social determinants of three measures of population health in a state across an entire state. In RI, as is the case with other northeastern states, local governance is conducted at the municipality (city or town) level. Therefore, study findings can be used at the local governance level to potentially implement policies and programs designed to improve population health and living conditions to reduce geographic disparities in health. Although not all social determinants of health could be obtained for this study, such as literacy, healthcare access, adverse childhood experiences, and others, the list of examined determinants represents a wide breadth of topics and measures, many of which are potentially modifiable. The study results could be used by policymakers, researchers, and the general public, to become informed about RI communities, as well as used as a template for analysis of social determinants of population health in other states and regions, as well. Furthermore, this study, like other studies [6, 8,9,10,11,12, 16,17,18,19,20,21,22,23,24,25,26,27,28,29, 40] also demonstrates that social determinants explain a substantial amount of the variability in population health across geographies.
Conclusions
Addressing the root causes of social determinants such as poverty, education, crime, and inequality that promote or deteriorate population health, is integral to improving population health and reducing critical health disparities [58]. This exploratory study highlights the geographic disparities in population health occurring in RI, and supports the preponderance of evidence suggesting that social determinants are associated with population health across the lifespan. Understanding and addressing key upstream drivers of population health and living conditions, especially those that are potentially modifiable through evidence-based policies, programs, and interventions, are critical to promoting health across all demographic groups.
Availability of data and materials
The data used in this study, the Behavioral Risk Factor Surveillance System, is publicly available on the CDC website (www.cdc.gov/brfss). The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- LE0:
-
Life expectancy at birth (age 0)
- LE65:
-
Life expectancy at age 65
- ASMR:
-
Age-standardized mortality rate (per 100,000)
- CDC:
-
Centers for Disease Control and Prevention
- RI:
-
Rhode Island
References
Eberhardt MS, Pamuk ER. The importance of place of residence: examining health in rural and nonrural areas. Am J Public Health. 2004;94(10):1682–6.
Krieger N. Putting health inequities on the map: social epidemiology meets medical/health geography––an ecosocial perspective. GeoJournal. 2009;74(2):87–97.
Edward J, Biddle DJ. Using geographic information systems (GIS) to examine barriers to healthcare access for Hispanic and Latino immigrants in the US south. J Racial Ethn Health Disparities. 2017;4(2):297–307.
Erwin PC, Fitzhugh EC, Brown KC, Looney S, Forde T. Health disparities in rural areas: the interaction of race, socioeconomic status, and geography. J Health Care Poor Underserved. 2010;21(3):931–45.
Koschinsky J. The case for spatial analysis in evaluation to reduce health inequities. Evaluation and Program Planning. 2013;36(1):172–6.
Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramanian SV, Carson R. Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter? The public health disparities geocoding project. Am J Epidemiol. 2002;156(5):471–82.
Gordon-Larsen P, Nelson MC, Page P, Popkin BM. Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics. 2006;117(2):417–24.
Baicker K, Chandra A, Skinner J. Geographic variation in health care and the problem of measuring racial disparities. Perspect Biol Med. 2005;48(1):42–S53.
Stiel L, Soret S, Montgomery S. Geographic patterns of change over time in mammography: differences between black and White US Medicare enrollees. Cancer Epidemiol. 2017;46:57–65.
Walker KE, Crotty SM. Classifying high-prevalence neighborhoods for cardiovascular disease in Texas. Appl Geogr. 2015;57:22–31.
Anderson RT, Yang TC, Matthews SA, Camacho F, Kern T, Mackley HB, Kimmick G, Louis C, Lengerich E, Yao N. Breast cancer screening, area deprivation, and later-stage breast cancer in Appalachia: does geography matter? Health Serv Res. 2014;49(2):546–67.
Jackson MC, Davis WW, Waldron W, McNeel TS, Pfeiffer R, Breen N. Impact of geography on mammography use in California. Cancer Causes Control. 2009;20(8):1339.
Woolf SH, Braveman P. Where health disparities begin: the role of social and economic determinants—and why current policies may make matters worse. Health Aff. 2011;30(10):1852–9.
Jia P, Shi X, Xierali IM. Teaming up census and patient data to delineate fine-scale hospital service areas and identify geographic disparities in hospital accessibility. Environ Monit Assess. 2019;191(2):303.
Braveman PA, Egerter SA, Woolf SH, Marks JS. When do we know enough to recommend action on the social determinants of health? Am J Prev Med. 2011;40(1):S58–66.
Beck AF, Sandel MT, Ryan PH, Kahn RS. Mapping neighborhood health geomarkers to clinical care decisions to promote equity in child health. Health Aff. 2017;36(6):999–1005.
Benach J, Yasui Y, Borrell C, Sáez M, Pasarin MI. Material deprivation and leading causes of death by gender: evidence from a nationwide small area study. J Epidemiol Community Health. 2001;55(4):239–45.
Diez Roux AV. Investigating neighborhood and area effects on health. Am J Public Health. 2001;91(11):1783–9.
Grow HM, Cook AJ, Arterburn DE, Saelens BE, Drewnowski A, Lozano P. Child obesity associated with social disadvantage of children’s neighborhoods. Soc Sci Med. 2010;71(3):584–91.
Kruger DJ, Reischl TM, Gee GC. Neighborhood social conditions mediate the association between physical deterioration and mental health. Am J Community Psychol. 2007;40(3–4):261–71.
Kulkarni SC, Levin-Rector A, Ezzati M, Murray CJ. Falling behind: life expectancy in US counties from 2000 to 2007 in an international context. Popul Health Metrics. 2011;9(1):16.
Lippert AM, Evans CR, Razak F, Subramanian SV. Associations of continuity and change in early neighborhood poverty with adult cardiometabolic biomarkers in the United States: results from the National Longitudinal Study of adolescent to adult health, 1995–2008. Am J Epidemiol. 2017;185(9):765–76.
Marmot M, Bell R. Social determinants and dental health. Adv Dent Res. 2011;23(2):201–6.
Mathers CD, Murray CJ, Salomon JA, Sadana R, Tandon A, Lopez AD, Ustün B, Chatterji S. Healthy life expectancy: comparison of OECD countries in 2001. Aust N Z J Public Health. 2003;27(1):5–11.
Olshansky SJ, Antonucci T, Berkman L, Binstock RH, Boersch-Supan A, Cacioppo JT, Carnes BA, Carstensen LL, Fried LP, Goldman DP, Jackson J. Differences in life expectancy due to race and educational differences are widening, and many may not catch up. Health Aff. 2012;31(8):1803–13.
Dwyer-Lindgren L, Stubbs RW, Bertozzi-Villa A, Morozoff C, Callender C, Finegold SB, Shirude S, Flaxman AD, Laurent A, Kern E, Duchin JS. Variation in life expectancy and mortality by cause among neighbourhoods in King County, WA, USA, 1990–2014: a census tract-level analysis for the global burden of disease study 2015. Lancet Public Health. 2017;2(9):e400–10.
Talbot TO, Done DH, Babcock GD. Calculating census tract-based life expectancy in New York state: a generalizable approach. Popul Health Metrics. 2018;16(1):1.
Clark CR, Williams DR. Understanding county-level, cause-specific mortality: the great value—and limitations—of small area data. JAMA. 2016;316(22):2363–5.
Hunt BR, Tran G, Whitman S. Life expectancy varies in local communities in Chicago: racial and spatial disparities and correlates. J Racial Ethn Health Disparities. 2015;2(4):425–33.
Ren C, Johnson R, Cohen SA, Zimmerman E, Phillips A, Haley A, Woolf S. Small-Area Life Expectancy: A comparison of methods, relationship to neighborhood sociodemographic factors, and outlier analysis. Popul Assoc Ann Meet. 2014; Available at: http://paa2014.princeton.edu/papers/142191.
Aron SB, McCrowell J, Moon A, Yamano R, Roark DA, Simmons M, Tatanashvili Z, Drake B. Analyzing the relationship between poverty and child maltreatment: investigating the relative performance of four levels of geographic aggregation. Soc Work Res. 2010;34(3):169–79.
Cohen SA, Greaney ML, Klassen AC. A “Swiss paradox” in the United States? Level of spatial aggregation changes the association between income inequality and morbidity for older Americans. Int J Health Geogr. 2019;18(1):1–2.
Arias E, Escobedo LA, Kennedy J, Fu C, Cisewski J. U.S. Small-area Life Expectancy Estimates Project: Methodology and Results Summary Cdc-pdf [PDF – 8 MB]. National Center for Health Statistics. Vital Health Stat. 2018;2(181).
Toson B, Baker A. Life expectancy at birth: methodological options for small populations. London: Office for National Statistics; 2003.
Silcocks PB, Jenner DA, Reza R. Life expectancy as a summary of mortality in a population: statistical considerations and suitability for use by health authorities. J Epidemiol Community Health. 2001;55(1):38–43.
Rhode Island Geographic Information System. Rhode Island Division of Planning. University of Rhode Island. Website: http://www.rigis.org/. Accessed May 30, 2020.
Fouweather T, Gillies C, Wohland P, Van Oyen H, Nusselder W, Robine JM, Cambois E, Jagger C. JA: EHLEIS team. Comparison of socio-economic indicators explaining inequalities in healthy life years at age 50 in Europe: 2005 and 2010. The European Journal of Public Health. 2015;25(6):978–83.
Higgins JP, Thompson SG. Controlling the risk of spurious findings from meta-regression. Stat Med. 2004;23(11):1663–82.
Hewson PJ. Epidemiology of child pedestrian casualty rates: can we assume spatial independence? Accid Anal Prev. 2005;37(4):651–9.
Assari S. Life expectancy gain due to employment status depends on race, gender, education, and their intersections. J Racial Ethn Health Disparities. 2018;5(2):375–86.
Montez JK, Hayward MD. Cumulative childhood adversity, educational attainment, and active life expectancy among US adults. Demography. 2014;51(2):413–35.
Meara ER, Richards S, Cutler DM. The gap gets bigger: changes in mortality and life expectancy, by education, 1981–2000. Health Aff. 2008;27(2):350–60.
Gundersen C, Ziliak JP. Food insecurity and health outcomes. Health Aff. 2015;34(11):1830–9.
Chetty R, Stepner M, Abraham S, Lin S, Scuderi B, Turner N, Bergeron A, Cutler D. The association between income and life expectancy in the United States, 2001-2014. JAMA. 2016;315(16):1750–66.
Dwyer-Lindgren L, Bertozzi-Villa A, Stubbs RW, Morozoff C, Mackenbach JP, van Lenthe FJ, Mokdad AH, Murray CJ. Inequalities in life expectancy among US counties, 1980 to 2014: temporal trends and key drivers. JAMA Intern Med. 2017;177(7):1003–11.
Williams DR, Priest N, Anderson NB. Understanding associations among race, socioeconomic status, and health: patterns and prospects. Health Psychol. 2016;35(4):407.
Cohen DA, Mason K, Bedimo A, Scribner R, Basolo V, Farley TA. Neighborhood physical conditions and health. Am J Public Health. 2003;93(3):467–71.
Redelings M, Lieb L, Sorvillo F. Years off your life? The effects of homicide on life expectancy by neighborhood and race/ethnicity in Los Angeles County. J Urban Health. 2010;87(4):670–6.
Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2016;30.
Subramanian SV, Acevedo-Garcia D, Osypuk TL. Racial residential segregation and geographic heterogeneity in black/white disparity in poor self-rated health in the US: a multilevel statistical analysis. Soc Sci Med. 2005;60(8):1667–79.
White K, Haas JS, Williams DR. Elucidating the role of place in health care disparities: the example of racial/ethnic residential segregation. Health Serv Res. 2012;47(3pt2):1278–99.
Mayne SL, Hicken MT, Merkin SS, Seeman TE, Kershaw KN, Do DP, Hajat A, Roux AV. Neighbourhood racial/ethnic residential segregation and cardiometabolic risk: the multiethnic study of atherosclerosis. J Epidemiol Community Health. 2019;73(1):26–33.
Jonker MF, van Lenthe FJ, Donkers B, Congdon PD, Burdorf A, Mackenbach JP. The impact of nursing homes on small-area life expectancies. Health Place. 2013;19:25–32.
Verropoulou G, Tsimbos C. Estimating mortality levels and patterns among natives, immigrants, and selected ethnic groups in Greece: 2010–2012. Int Migr Rev. 2017;51(3):600–31.
MacDonald H. The American community survey: warmer (more current), but fuzzier (less precise) than the decennial census. J Am Plan Assoc. 2006;72(4):491–503.
Eayres D, Williams ES. Evaluation of methodologies for small area life expectancy estimation. J Epidemiol Community Health. 2004;58(3):243–9.
Jonker MF, Van Lenthe FJ, Congdon PD, Donkers B, Burdorf A, Mackenbach JP. Comparison of Bayesian random-effects and traditional life expectancy estimations in small-area applications. Am J Epidemiol. 2012;176(10):929–37.
Zimmerman EB, Woolf SH, Blackburn SM, Kimmel AD, Barnes AJ, Bono RS. The case for considering education and health. Urban Educ. 2018;53(6):744–73.
Acknowledgements
We gratefully acknowledge the funding source for the Rhode Island Life Expectancy Project, the University of Rhode Island Council for Research. We also thank Catherine Lenox of the University of Rhode Island for her help with the project and Heather O’Neil and her team at Pixels for Humans for their support with the project and for developing the associated project website.
Funding
The University of Rhode Island Council for Research provided funding for this project, including the development of the accompanying website, summer salary support, and support for a research assistant to help with data compilation and analysis.
Author information
Authors and Affiliations
Contributions
SAC conceived the study and provided oversight of all study activities, including data compilation and analysis and preparation of the manuscript. JRB provided critical support in data collection and analysis, and wrote parts of this manuscript. MLG assisted with the preparation of the manuscript by providing critical edits of the text and analysis. SAC, JRB, and MLG approved the manuscript submitted for potential publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study received approval from the University of Rhode Island Institutional Review Board on July 10, 2018 (IRB # 1249971–2).
Consent for publication
Not applicable. All data analyses are secondary. All survey participants have provided their consent to be in the survey (CDC).
Competing interests
MLG is an Associate Editor on BMC Public Health. The other authors have no competing interests to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cohen, S.A., Broccoli, J.R. & Greaney, M.L. Community-based social determinants of three measures of mortality in Rhode Island cities and towns. Arch Public Health 78, 56 (2020). https://doi.org/10.1186/s13690-020-00438-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13690-020-00438-7