Abstract
Background
The aim of this individual participant data meta-analysis (IPDMA) is to evaluate the effects of dietary and lifestyle interventions among pregnant women who are overweight or obese on later maternal and early childhood outcomes at ages 3–5 years.
Methods/design
We will build on the established International Weight Management in Pregnancy (i-WIP) IPD Collaborative Network, having identified researchers who have conducted randomised dietary and lifestyle interventions among pregnant women who are overweight or obese, and where ongoing childhood follow-up of participants has been or is being undertaken. The primary maternal outcome is a diagnosis of maternal metabolic syndrome. The primary childhood outcome is BMI above 90%.
We have identified 7 relevant trials, involving 5425 women who were overweight or obese during pregnancy, with approximately 3544 women and children with follow-up assessments available for inclusion in the meta-analysis.
Discussion
The proposed IPDMA provides an opportunity to evaluate the effect of dietary and lifestyle interventions among pregnant women who are overweight or obese on later maternal and early childhood health outcomes, including risk of obesity. This knowledge is essential to effectively translate research findings into clinical practice and public health policy.
Systematic review registration
This IPD has been prospectively registered (PROSPERO), ID number CRD42016047165.
Similar content being viewed by others
Background
Globally, 1.46 billion adults [1], and 170 million children under the age of 18 years [2], are estimated to be overweight or obese. Obesity is occurring at an increasingly early age, affecting more than 43 million children aged 0–5 years world-wide [3], leading the World Health Organization to describe childhood obesity as “one of the most serious public health challenges of the 21st century [4]”. With obesity occurring earlier in life, the aggregate exposure and risk of deleterious health consequences also increases [5].
A variety of factors have been identified as increasing an individual’s risk of increased adiposity and obesity in childhood. In particular, both high maternal BMI and excessive gestational weight gain during pregnancy have been consistently identified as significant independent pre-natal factors [6–9]. Recognized postnatal factors operating in early infancy include feeding (exposure to breast feeding, formula feeding, and introduction of solids), activity (including sedentary behaviours), and sleep duration, although the associations between parental and postnatal factors are complex, and the extent to which they may be modified by intrauterine events is unclear [10].
Maternal overweight and obesity represents a significant health issue for women during pregnancy and childbirth, with estimates suggesting that over 50% of women enter pregnancy with a BMI in excess of 25 kg/m2 [11]. While there are well-documented risks associated with obesity during pregnancy for both the woman and her infant [12, 13], there is an increasing recognition of the association between maternal obesity and subsequent obesity in her offspring, developing in early infancy [14] and extending into later childhood [15–17]. Independent of maternal obesity, high gestational weight gain (GWG) is also associated with an increased risk of pre-school obesity [17–19].
Excessive GWG is recognized as a significant risk factor for maternal postpartum weight retention and the subsequent development of obesity [20–22], contributing to an increase in inter-pregnancy BMI, and an increased risk of adverse outcomes in a subsequent pregnancy [22–24]. Excessive GWG is also consistently associated with a greatly increased risk of a woman subsequently developing diabetes in later life [25, 26], when compared with women whose weight gain was within the IoM recommendations. A similar increase in risk of cardiovascular disease in later life has also been reported among women with excessive pregnancy weight gain [27–30].
The major complications associated with obesity during pregnancy and childbirth for women and their infants are well defined, and a comprehensive systematic review led by Thangaratinam and colleagues [31] has identified numerous studies assessing dietary and lifestyle interventions in pregnancy. However, the effect of these pregnancy interventions on later maternal and early childhood health is yet to be evaluated. The International Weight Management in Pregnancy (i-WIP) Collaborative group is near completion of an individual participant data meta-analysis (IPDMA), funded by the UK NIHR, evaluating the effect of dietary and lifestyle interventions during pregnancy on short-term pregnancy and birth outcomes [32]. We propose to extend this existing collaboration to evaluate the effect of dietary and lifestyle interventions among pregnant women who are overweight or obese on later maternal and early childhood health outcomes, establishing the International Weight Management in Pregnancy Collaboration: 3-year follow-up (i-WIP-3).
While systematic review and traditional methods of meta-analysis generate robust evidence regarding healthcare interventions [33], recent calls have advocated that level-1 evidence be attributed to IPDMA [34, 35]. Despite this, IPDMA remains under-utilised as a methodological tool, limiting the quality and robustness of clinical care guidelines and their recommendations [35]. Use of IPDMA methodology greatly increases statistical power to generate unequivocal pooled risk estimates and to identify key maternal characteristics and critical components of the intervention contributing to maternal and childhood health. Combining and analyzing the extensive volume of randomised controlled trial (RCT) data available world-wide avoids the expense, duplication of effort, and inevitable time delays of undertaking further very large-scale trial(s) with pre-specified longer-term primary outcomes relating to maternal and child cardio-metabolic health.
Aims
Using IPDMA, we will determine the effects of antenatal dietary and lifestyle interventions in pregnancy for women who are overweight or obese on longer-term health outcomes for the women and their children at 3-5 years of age; this will also be assessed in particular groups at greater risk to inform potential targeting of the intervention.
With the available raw participant level data, we will address the effect of antenatal dietary and lifestyle interventions on longer-term health outcomes, overall, and according to maternal subgroups. The primary subgroup analysis is early pregnancy body mass index (BMI) category (25.0–29.9 vs ≥30.0 kg/m2). Secondary subgroup analyses will also be carried out on subgroups defined by the following characteristics:
-
1)
Ethnicity (Caucasian vs Asian vs African);
-
2)
Socioeconomic status (high vs low social disadvantage) at time of randomisation during pregnancy;
-
3)
Parity (0 vs ≥1) at time of randomisation during pregnancy; and
-
4)
Gestational weight gain (as a continuous variable, and according to adherence to the Institute of Medicine (IoM) gestational weight gain recommendations) [36].
Methods
Study design
We will conduct an IPDMA, utilising an approach that follows existing guidelines and that complies with the PRISMA-IPD statement and recent reporting guidelines for IPD meta-analysis (Additional file 1) [37].
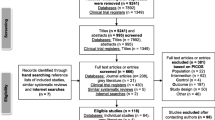
Inclusion criteria for the studies and search strategy
Individual patient data from RCTs in which women with a singleton, live gestation between 10+0–20+0 weeks, and of BMI ≥ 25.0 kg/m2 at the time of the first antenatal visit, were randomised to receive a diet and/or lifestyle intervention or continued standard antenatal care, and in which longer-term maternal and child follow-up has been undertaken. The current studies were identified by a systematic literature search within the i-WIP collaboration [32]. We will update our previously described literature search, without language restrictions, in order to identify any new potential relevant trials with planned or published follow-up at the commencement of the project and 1 year prior to its completion to minimise the potential to miss relevant trials [32].
To date, we have identified seven such randomised trials, with collaborators providing in principal agreement to access de-identified individual participant data for women and their children. The characteristics of each trial are presented in Table 1. We are aware of two studies currently recruiting to the primary pregnancy intervention, with an intention to conduct longer-term maternal and child follow-up [38, 39].
Types of participants
Women with a singleton, live gestation between 10+0–20+0 weeks and of BMI ≥ 25.0 kg/m2 at the time of their first antenatal visit, and in which subsequent maternal and child follow-up has been planned or undertaken at 3–5 years of age.
Types of interventions
Antenatal dietary and/or lifestyle interventions compared with continued standard antenatal care.
Data collection and management
Each trial will contribute de-identified patient level data for each participant randomised. This will be stored in a secure, centralised database with access available only to authorised members of the i-WIP-3 data management group. The database will build on that currently used in the i-WIP collaboration. Specifically, data already housed has been coded for anonymity and relates to the women randomised (date of birth, center identification); baseline descriptive information (age, parity, ethnicity, BMI, smoking status, socioeconomic status, expected date of confinement); allocated treatment intervention; and pregnancy and birth outcome variables.
All data provided from individual trials will be checked to ensure internal consistency as well as consistency with published reports and to assess missing data, using published data, trial protocols, and data collection sheets. Similarly, the randomisation process for each trial will be checked, including the chronological randomisation sequence, stratification variables, and allocation assignment to consider the distribution of prognostic factors across treatment groups. Where inconsistencies are identified, they will be discussed with the individual investigators and will be resolved through consensus. In the initial stages, each trial will be analysed separately, and the output generated cross-checked against published data and verified by the individual investigator before being incorporated into the combined database.
Variables available through the i-WIP collaboration
Trial level information has already been collected and exists within the database. This includes the number of women randomised; methods of random allocation; stratification variables; methods of allocation concealment; blinding of outcome assessment; nature of the intervention (including the content of the intervention, and the number and format in which the sessions were provided); nature of standard antenatal care provided.
Maternal participant level information has already been collected and exists within the database. This includes a unique participant code to ensure anonymity; maternal age; body mass index; parity; ethnicity; smoking status; and socioeconomic status.
Maternal pregnancy and birth outcome variables occurring after the time of randomisation have been collected and exist within the database. This includes pregnancy outcomes (including gestational diabetes, pre-eclampsia, and hypertension, pre-term birth, gestational weight gain); and birth outcomes (including induction of labour, mode of birth, estimated blood loss). Maternal dietary and physical activity reports are also available.
Neonatal participant level information has already been collected and exists within the database. A unique neonatal identification code will be linked to the maternal identification code to ensure anonymity. Outcome variables include gestational age at birth, birth weight, small and large for gestational age, perinatal death, shoulder dystocia, birth trauma, and admission to the neonatal intensive care unit (NICU).
Variables to be collected through the i-WIP-3 Collaboration
Extended maternal participant level information will be collected and entered into an expanded database housing the above information. Outcome variables will include height, weight, BMI, skinfold thickness measurements, calculated percentage body fat and fat-free mass, dietary and physical activity patterns, blood pressure, quality of life and emotional wellbeing, and general health (Table 2).
Childhood participant level information will be collected and entered into an expanded database housing the above information. A unique childhood identification code will be linked to the neonatal and maternal identification codes to ensure anonymity. Outcome variables will include height, weight, BMI, skinfold thickness measurements, calculated percentage body fat and fat-free mass, dietary and physical activity patterns, blood pressure, neurodevelopmental outcome domains, and general health (Table 3).
Establishment of outcome measures
To determine primary and secondary maternal and child outcomes, we conducted a Delphi survey. An initial list of outcomes was incorporated into a previous Delphi survey conducted by the i-WIP group, with a specific focus on outcomes relevant to women and their children [40]. We undertook a two-stage Delphi survey (February to April 2016) using a methodology consistent with current recommendations [41], in order to prioritise maternal and childhood outcomes of relevance to clinical practice. The panel involved members of the i-WIP collaborative steering committee, members from the planned IPD investigators, and other identified multi-disciplinary experts in the field.
An online survey tool was used and a link sent to individual members of the panel, who were asked to score each listed maternal and childhood outcome in terms of clinical relevance for patient care. A nine-point Likert scale was used to evaluate the importance, with a score of 9 considered critical, while a score of 1 was considered of limited importance to patient care. In the first round of the survey, participants were asked to suggest other relevant outcomes that may not have been included. These additional outcomes were included in the second round of the survey. For each outcome, a median and interquartile range (IQR) was calculated. This information was then provided to panelists in the second round of the survey. For each survey round, an e-mail reminder was sent if no response had been received within 2 weeks, with a second reminder sent after 4 weeks.
A total of 21 of 41 individuals completed both the first and second rounds of the survey. The median and IQR for maternal and childhood outcomes are shown in Tables 4 and 5.
Primary outcome measures
The primary maternal outcome is a diagnosis of maternal metabolic syndrome. The primary childhood outcome is BMI above 90%. Secondary outcome measures are presented in Tables 2 and 3.
Data management and statistical analyses
Data checking
The IPDMA project coordinator will check all new maternal and child follow-up data provided from the individual trials to ensure internal consistency and consistency with published reports and to assess missing data, using published data, trial protocols, and data collection sheets. Similarly, the randomisation process for each trial will be checked, including the chronological randomisation sequence, stratification variables, and allocation assignment to consider the distribution of prognostic factors across treatment groups. Where inconsistencies are identified, they will be discussed with the individual investigators and resolved through consensus. Initially, each trial will be analysed separately, and the output generated will be cross-checked against published data and verified by the individual investigator before being incorporated into the IPDMA database.
Data transformation
Data from each trial will be combined in a common data set, after the above. Each patient will retain a unique trial identifier. The combined data set will be used to define the new variables required to address the hypotheses of the proposal.
Statistical analyses
A detailed statistical analysis plan will be prepared and agreed upon by members of the i-WIP-3 collaboration, prior to the conduct of any analyses. All randomised participants with available outcome data will be included in the analyses, on an intention-to-treat basis, according to the treatment group to which the woman was allocated at the time of randomisation (dietary and/or lifestyle intervention vs standard care). Imputation methods will be used to account for missing data.
The statistical analyses of this IPDMA will utilize methods described in the Cochrane Collaboration Handbook [42] and as outlined for the i-WIP IPDMA [32]. Firstly, we will summarise the overall effect of each intervention in relation to each outcome. Meta-analyses of the effectiveness of antenatal interventions in pregnancy will be performed for the primary and secondary maternal and child outcomes. We will include all patients randomised and will adopt intention-to-treat principles.
All trials will be reanalysed separately, and the investigators asked to confirm their individual results, with resolution of any discrepancies. We will then perform a one-step IPDMA to generate a pooled intervention effect. A two-step IPDMA will also be conducted as a secondary analysis for comparison with the one-step results, unless convergence issues with the one-step analysis require the use of the two-step approach. A one-step approach accounts for clustering of participants within studies and analyses IPD from all trials simultaneously. A two-step approach first estimates the intervention effect from the IPD in each study separately and then pools them using a conventional meta-analysis of the intervention effect estimates obtained. While one and two-step meta-analyses typically yield similar results, both will be undertaken to ensure robust conclusions [43, 44].
We anticipate that there will be evidence of heterogeneity in our IPDMA and will therefore use a random effects approach to account for between study heterogeneity in intervention effect. Heterogeneity will be summarised using the I-squared statistic (which describes the proportion of total variability due to between study heterogeneity) and the estimated between-study variance (‘tau-squared’).
For continuous outcomes, we will use mean differences, which will be standardized where possible if outcome scales differ substantially, with adjustment for baseline values using analysis of covariance [45]. For binary outcomes, we will calculate relative risks and incorporate modelling where required (for example, logistic regression to adjust for clustering). We will assume that the random effects contributing to heterogeneity at the individual trial level will be normally distributed, although it is unlikely that violation of this assumption will affect the results of the analysis [46].
The subgroups to be considered as causes of heterogeneity and potential modifiers of the effect of the intervention include maternal BMI category, ethnicity, socioeconomic status, parity, and maternal gestational weight gain. We will generate summary intervention effects in each subgroup using the same random-effects meta-analysis approach as described above. Subgroup analyses, if not carefully planned, can lead to misleading results, and we will therefore exercise caution in the interpretation of subgroup results, with adjustment for multiple testing.
To explore the possibility of chance effects contributing to the findings of our subgroup analyses, we will incorporate treatment-covariate interaction terms in the analysis. This will ensure that we estimate the pooled within-trial interaction of interest separately from the across-trial (meta-regression) interaction, as recommended because the former is the desired information as it is based solely on patient-level information [47, 48].
A secondary analysis will evaluate the association between maternal gestational weight gain and maternal and child outcomes in overweight and obese women. We will fit a suitable regression model to account for clustering of participants within individual trials and quantify how each 1-unit increase in weight gain changes the risk of each outcome. As the relationship may be non-linear, we will use fractional polynomial terms [49]. Modelling will use linear regression for continuous variables and logistic regression for binary variables, and will also account for clustering of participants within trials, as well as their allocated treatment intervention during pregnancy.
Study quality assessment and evaluation of nonresponse bias
We will consider all recorded variables, even those not reported in the published studies. The quality of each trial will be assessed [50, 51] to evaluate the integrity of the randomisation and follow-up procedure. We will evaluate the risk of bias in individual studies by considering six items used in the Cochrane risk of bias tool: sequence generation, allocation concealment, blinding, incomplete outcome data, selective outcome reporting, and other potential sources of bias.
If individual patient data are not received from all identified studies, the potential for bias due to nonresponse will be assessed by descriptive comparison of participating and non-participating studies, in terms of study characteristics (sample size, where and when conducted, etc.), patient population, and main effect estimate (where possible). Comparison of results from the two-stage meta-analysis with those of the one-stage analysis will also be used to assess the potential for nonresponse bias.
Sample size
There are a total of 3544 women and children with data available at the 3-year follow-up across the 7 trials; the smallest study has a sample size of 134. Power and coverage (alpha/type I error) for the main child outcome (BMI > 90%) and for the main subgroup analysis (interaction between treatment and maternal early pregnancy BMI category) were investigated across 1000 simulated datasets using the ipdpower command in Stata [52]. The simulated datasets incorporated study-specific fixed intercepts (base log-odds), fixed effects for maternal BMI category and treatment-by-BMI interaction, and random effects for treatment.
For the main childhood outcome (BMI > 90%), assuming a reduction in incidence from 21.0% in the control group to 16.7% in the treatment group (corresponding to a treatment effect OR of approximately 0.75), and stipulating a high degree of between-study heterogeneity for the random treatment effect (SD on the log-odds scale corresponding to 1/3 of the average effect), there was 85% power (95% CI 82.6–87.2%) to detect the treatment effect. Coverage was acceptable at 92% (95% CI 90.1–93.6).
For the main subgroup analysis, assuming that the treatment effect in the higher BMI category is approximately 1.5 times that in the lower BMI category (OR of 1.5); that the control group OR for the higher BMI category compared to the lower BMI category is approximately 1.6, and that about 70% of women have early pregnancy BMI in the higher category (≥30.0), there is greater than 80% power to detect the interaction effect (82.2%, with 95% CI 79.6–84.5%), with good coverage of 96.4% (95% CI 95.0–97.5%).
Management considerations
The i-WIP-3 Collaboration will have a steering group consisting of the current named authors, which includes a representative from each of the individual randomised trials contributing individual patient data, in addition to the project coordinator and statistician. The steering committee will meet initially to discuss and finalise the definitions and outcomes to be assessed and the statistical processes proposed. Where possible, one face-to-face collaborator meeting will be scheduled each year, at which key decisions, including the project design, analysis plan, and interpretation of findings will be discussed.
The operational requirements of the project will be performed by the project coordinator and statistician, in conjunction with the individual trial managers and statisticians and will be overseen by the chair of the steering committee.
Publication considerations
Each member of the steering committee will be provided with the results of the analysis, and a meeting will be held to discuss and interpret the findings. The current named authors will be responsible for the preparation of manuscripts, which will then be circulated to each member of the committee for further discussion prior to submission for publication. Where possible, each member of the steering committee will be named as an author on any publications arising from the analysis and on behalf of the i-WIP-3 collaboration as a whole, with acknowledgement of all participating collaborators within the manuscript.
Discussion
There is an increasing recognition of the association between maternal obesity, high infant birth weight, and the subsequent development of childhood obesity. In a large population cohort from the United States, the overall incidence of infant birth weight above 4 kg was approximately 12% [53]. However, approximately 1 in 5 children who were obese at ages 5–6 years had birth weight above 4 kg, increasing to almost one third of obese individuals at age 14 years [53]. Therefore, antenatal interventions which are successful in reducing the risk of maternal gestational weight and adiposity gain and/or high birth weight infants represent a public health strategy of considerable significance to tackle the global issue of increasing obesity and adverse health in children and in adults [54].
Our proposed IPDMA provides a unique opportunity to evaluate the effect of dietary and lifestyle interventions among pregnant women who are overweight or obese on later maternal and early childhood health outcomes, including risk of obesity. Importantly, we will build on the successful existing i-WIP project, which has standardized the baseline characteristics of women recruited to randomised trials, interventions, and short-term pregnancy and birth outcomes. While each of the identified randomised trials are sufficiently similar in design and outcomes to allow meaningful meta-analysis to occur, the intensity of the intervention provided and social demographics of included participants is diverse with the IPD proposed enabling identification of effect modifiers through pre-specified subgroup analyses.
Furthermore, this can be achieved in a relatively efficient manner and with sufficient statistical power, avoiding the expense, duplication of effort, and inevitable time delays in undertaking another large-scale pregnancy intervention trial with a pre-specified primary outcome of later maternal or early childhood obesity. This knowledge is essential to effectively translate research findings into clinical practice and public health policy, and to maximise the return on publicly funded research investments globally.
Abbreviations
- BMI:
-
Body mass index
- GWG:
-
Gestational weight gain
- IPD:
-
Individual participant data
- IPDMA:
-
Individual participant data meta-analysis
- IQR:
-
Interquartile range
- i-WIP:
-
International Weight Management in Pregnancy
- NICU:
-
Neonatal intensive care unit
- OR:
-
Odds ratio
- RCT:
-
Randomised controlled trial
- UK-NIHR:
-
United Kingdom-National Institute for Health Research
References
Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, Paciorek CJ, Singh GM, Gutierrez HR, Lu Y, Bahalim AN, et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9 · 1 million participants. Lancet. 2011;377(9765):557–67.
Lobstein T, Baur L, Uauy R, Force fIIOT. Obesity in children and young people: a crisis in public health. Obes Rev. 2004;5 Suppl 1:4–104.
de Onis M, Blossner M, Borghi E. Global prevalence and trends of overweight and obesity among preschool children. Am J Clin Nutr. 2010;92:1257–64.
World Health Organization (WHO). Global strategy on diet, physical activity and health: childhood overweight and obesity, vol. Geneva; 2011.http://www.who.int/dietphysicalactivity/childhood/en/. Accessed 9 Sept 2016.
Hannon TS, Rao G, Arsianian SA. Childhood obesity and type 2 diabetes mellitus. Pediatrics. 2005;116(2):473–80.
Godfrey KM, Inskip HM, Hanson MA. The long-term effects of prenatal development on growth and metabolism. Semin Reprod Med. 2011;29(3):257–65.
Wells JC, Haroun D, Levene D, Darch T, Williams JE, Fewtrell MS. Prenatal and postnatal programming of body composition in obese children and adolescents: evidence from anthropometry, DXA and the 4-component model. Int J Obes. 2011;35(4):534–40.
Winter JD, Langenberg P, Krugman SD. Newborn adiposity by body mass index predicts childhood overweight. Clin Pediatr. 2010;49(9):866–70.
Baird J, Fisher D, Lucas P, Kleijnen J, Roberts H, Law C. Being big or growing fast: systematic review of size and growth in infancy and later obesity. BMJ. 2005;331(7522):929.
Poston L. Maternal obesity, gestational weight gain and diet as determinants of offspring long term health. Best Pract Res Clin Endocrinol Metab. 2012;26(5):627–39.
Chan A, Scott J, Nguyen A-M, Sage L. Pregnancy outcome in South Australia 2006. In. Edited by Pregnancy Outcome Unit SADoH. Adelaide: Government of South Australia; 2008.
Callaway LK, Prins JB, Chang AM, McIntyre HD. The prevalence and impact of overweight and obesity in an Australian obstetric population. MJA. 2006;184(2):56–9.
Dodd JM, Grivell RM, Nguyen A-M, Chan A, Robinson JS. Maternal and perinatal health outcomes by body mass index category. ANZJOG. 2011;51(2):136–40.
Tikellis G, Ponsonby AL, Wells JC, Pezic A, Cochrane J, Dwyer T. Maternal and infant factors associated with neonatal adiposity: results from the Tasmanian Infant Health Survey (TIHS). Int J Obes. 2012;36(4):496–504.
Fraser A, Tilling K, Macdonald-Wallis C, Sattar N, Brion MJ, Benfield L, Ness A, Deanfield J, Hingorani A, Nelson SM, et al. Association of maternal weight gain in pregnancy with offspring obesity and metabolic and vascular traits in childhood. Circulation. 2010;121:2557–64.
Kitsantas P, Gaffney KF. Risk profiles for overweight/obesity among preschoolers. Early Hum Dev. 2010;86:563–8.
Rooney BL, Mathiason MA, Schauberger CW. Predictors of obesity in childhood, adolescence, and adulthood in a birth cohort. Maternal Child Health J. 2010. doi: 10.1007/s10995-010-0689-1.
Oken E, Taveras EM, Kleinman KP, Rich-Edwards JW, Gillman MW. Gestational weight gain and child adiposity at age 3 years. Am J Obstet Gynecol. 2007;196:322–8.
Wrotniak BH, Shults J, Butts S, Stettler N. Gestational weight gain and risk of overweight in the offspring at age 7 y in a multicenter, multiethnic cohort study. Am J Clin Nutr. 2008;87(6):1818–24.
Rooney BL, Schauberger CW. Excess pregnancy weight gain and long-term obesity: one decade later. Obstet Gynecol. 2002;100(2):245–52.
Rooney BL, Schauberger CW, Mathiason MA. Impact of perinatal weight change on long-term obesity and obesity-related illnesses. Obstet Gynecol. 2005;106(6):1349–56.
Amorim AR, Rössner S, Neovius M, Lourenço PM, Linné Y. Does excess pregnancy weight gain constitute a major risk for increasing long-term BMI? Obesity (Silver Spring). 2007;15(5):1278–86.
Kac G, Benício MH, Velásquez-Meléndez G, Valente JG, Struchiner CJ. Gestational weight gain and prepregnancy weight influence postpartum weight retention in a cohort of brazilian women. J Nutr. 2004;134(3):661–6.
Parker JD, Abrams B. Differences in postpartum weight retention between black and white mothers. Obstet Gynecol. 1993;81:768–74.
Retnakaran R, Qi Y, Sermer M, Connelly PW, Hanley AJ, Zinman B. Glucose intolerance in pregnancy and future risk of pre-diabetes or diabetes. Diabetes Care. 2008;31(10):2026–31.
Hedderson MM, Gunderson EP, Ferrara A. Gestational weight gain and risk of gestational diabetes mellitus. Obstet Gynecol. 2010;115(3):597–604.
Shah BR, Retnakaran R, Booth GL. Increased risk of cardiovascular disease in young women following gestational diabetes mellitus. Diabetes Care. 2008;31(8):1668–9.
Jonsdottir LS, Arngrimsson R, Geirsson RT, Sigvaldason H, Sigfusson N. Death rates from ischemic heart disease in women with a history of hypertension in pregnancy. Acta Obstet Gynecol Scand. 1995;74(10):772–6.
Fraser A, Tilling K, Macdonald-Wallis C, Hughes R, Sattar N, Nelson SM, Lawlor DA. Associations of gestational weight gain with maternal body mass index, waist circumference, and blood pressure measured 16 y after pregnancy: the Avon Longitudinal Study of Parents and Children (ALSPAC). Am J Clin Nutr. 2011;93(6):1285–92.
Mamun AA, Kinarivala M, O’Callaghan MJ, Williams GM, Najman JM, Callaway LK. Associations of excess weight gain during pregnancy with long-term maternal overweight and obesity: evidence from 21y postpartum follow-up. Am J Clin Nutr. 2010;91:1336–41.
Thangaratinam S, Rogozinska E, Jolly K, Glinkowski S, Roseboom T, Tomlinson JW, Kunz R, Mol BW, Coomarasamy A, Khan KS. Effects of interventions in pregnancy on maternal weight and obstetric outcomes: meta-analysis of randomised evidence. BMJ. 2012;344:e2088.
Ruifrok AE, Rogozinska E, van Poppel MN, Rayanagoudar G, Kerry S, de Groot CJ, Yeo S, Molyneaux E, McAuliffe FM, Poston L, et al. Study protocol: differential effects of diet and physical activity based interventions in pregnancy on maternal and fetal outcomes--individual patient data (IPD) meta-analysis and health economic evaluation. Syst Rev. 2014;3:131. doi:10.1186/2046-4053-3-131.
Council NHaMR. How to review the evidence: systematic identification and review of the scientific literature. Canberra: Commonwealth of Australia; 2005.
Chalmers I. The Cochrane Collaboration: preparing, maintaining and disseminating systematic reviews of the effects of health care. Ann NY Acad Sci. 1993;703:156–65.
Vale CL, Rydzewska LH, Rovers MM, Emberson JR, Gueyffier F, Stewart LA, Group. ftCIM-aM. Uptake of systematic reviews and meta-analyses based on individual participant data in clinical practice guidelines: descriptive study. BMJ. 2015;350:h1088.
Institute of Medicine (IOM). Weight gain during pregnancy: reexamining the guidelines. Edited by Rasmussen KM, Yaktine AL. Washington D.C.: National Academies Press; 2009.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group. fTP. Preferred reporting items for systematic reviews and meta-analyses: the prisma statement. BMJ. 2009;339:b2535. doi:10.1136/bmj.b2535.
Rauh K, Kunath J, Rosenfeld E, Kick L, Ulm K, Hauner H. Healthy living in pregnancy: a cluster-randomized controlled trial to prevent excessive gestational weight gain - rationale and design of the GeliS study. BMC Pregnancy Childbirth. 2014;14:119.
An Optimized Programming of Healthy Children (APPROACH). https://www.clinicaltrials.gov/ct2/show/NCT01894139. Accessed 10 Nov 2016.
Rogozinska E, D’Amico MI, Khan KS, Cecatti JG, Teede H, Yeo S, Vinter CA, Rayanagoudar G, Carballo RB, Perales M, et al. Development of composite outcomes for individual patient data (IPD) meta-analysis on the effects of diet and lifestyle in pregnancy: a Delphi survey. BJOG. 2016;123:190–8.
Boulkedid R, Abdoul H, Loustau M, Sibony O, Alberti C. Using and Reporting the Delphi Method for Selecting Healthcare Quality Indicators: A Systematic Review. PLoS One. 2011;6(6):e20476.
Stewart LA, Tierney JF, Clarke M, Group. obotCIPDM-aM. Reviews of individual patient data. In: Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. Volume Version 5.0.2, edn. Chichester: The Cochrane Collaboration; 2009.
Riley RD, Lambert PC, Abo-Zaid G. Meta-analysis of individual participant data: rationale, conduct, and reporting. BMJ. 2010;340:c221.
Debray TP, Moons KG, Abo-Zaid GM, Koffijberg H, Riley RD. Individual participant data meta-analysis for a binary outcome: one-stage or two- stage? PLoS One. 2013;8:e60650.
Vickers AJ, Altman DG. Statistics notes: analysing controlled trials with baseline and follow up measurements. BMJ. 2001;323:1123–4.
Kontopantelis E, Reeves D. Performance of statistical methods for meta-analysis when true study effects are non-normally distributed: a simulation study. Stat Methods Med Res. 2012;21(4):409–26.
Riley RD, Lambert PC, Staessen JA, Wang J, Gueyffier F, Thijs L, Boutitie F. Meta-analysis of continuous outcomes combining individual patient data and aggregate data. Stat Med. 2008;27:1870–93.
Riley RD, Steyerberg EW. Meta-analysis of a binary outcome using individual participant data and aggregate data. J Res Syn Meth. 2010;1:2–9.
Royston P, Sauerbrei W. A new approach to modelling interactions between treatment and continuous covariates in clinical trials by using fractional polynomials. Stat Med. 2004;23:2509–25.
Guyatt GH, Oxman AD, Kunz R, Vist GE, Falck-Ytter Y, Schunemann HJ, Group GW. What is “quality of evidence” and why is it important to clinicians? BMJ. 2008;336(7651):995–8.
Glasziou P, Chalmers I, Altman DG, Bastian H, Boutron I, Brice A, Jamtvedt G, Farmer A, Ghersi D, Groves T, et al. Taking healthcare interventions from trial to practice. BMJ. 2010;341:c3852.
Kontopantelis E, Springate D, Parisi R, Reeves D. Simulation-based power calculations for mixed effects modeling: ipdpower in Stata. J Stat Softw. 2016;74(12):1–25.
Cunningham SA, Kramer MR, Narayan KM. Incidence of childhood obesity in the United States. N Engl J Med. 2014;370(5):403–11.
Poston L. Healthy eating in pregnancy—always a good idea, now with more supporting evidence. BMJ. 2014;348:g1739.
Dodd JM, Cramp CS, Sui Z, Yelland LN, Deussen AR, Grivell RM, Moran LJ, Crowther CA, Turnbull DA, McPhee AJ, et al. Effects of antenatal lifestyle advice for women who are overweight or obese on maternal diet and physical activity: the LIMIT randomised trial. BMC Med. 2014;12:161. http://www.biomedcentral.com/1741-7015/12/161.
Dodd JM, McPhee AJ, Turnbull DA, Yelland LN, Deussen AR, Grivell RM, Wittert G, Owens JA, Robinson JS, group. ftLrt. The effect of antenatal lifestyle advice for women who are overweight or obese on neonatal health: the LIMIT randomised trial. BMC Med. 2014;12:163. http://www.biomedcentral.com/1741-7015/12/163.
Dodd JM, Turnbull DA, McPhee AJ, Deussen AR, Grivell RM, Yelland LN, Crowther CA, Wittert G, Owens JA, Robinson JS. Antenatal lifestyle advice for women who are overweight or obese: the LIMIT randomised trial. BMJ. 2014;348:g1285.
Poston L, Bell R, Croker H, Flynn AC, Godfrey KM, Goff L, Hayes L, Khazaezadeh N, Nelson SM, Oteng-Ntim E, et al. Effect of a behavioural intervention in obese pregnant women (the UPBEAT study): a multicentre, randomised controlled trial. Lancet Diabetes and Endocrinol. 2015. (http://dx.doi.org/10.1016/S2213-8587(15)00227-2).
Walsh JM, McGowan CA, Mahony R, Foley ME, McAuliffe FM. Low glycaemic index diet in pregnancy to prevent macrosomia (ROLO study): randomised control trial. BMJ. 2012;345:e5605.
Vinter CA, Jensen DM, Ovesen P, Beck-Nielsen H, Jørgensen JS. The LiP (Lifestyle in Pregnancy) study: a randomized controlled trial of lifestyle intervention in 360 obese pregnant women. Diabetes Care. 2011;34(12):2502–7.
Vinter CA, Jensen DM, Ovesen P, Beck-Nielsen H, Tanvig M, Lamont RF, Jørgensen JS. Postpartum weight retention and breastfeeding among obese women from the randomized controlled Lifestyle in Pregnancy (LiP) trial. Acta Obstet Gynecol Scand. 2014;93(8):794–801.
Tanvig M, Vinter CA, Jørgensen JS, Wehberg S, Ovesen PG, Beck-Nielsen H, Christesen HT, Jensen DM. Effects of lifestyle intervention in pregnancy and anthropometrics at birth on offspring metabolic profile at 2.8 years: results from the Lifestyle in Pregnancy and Offspring (LiPO) study. J Clin Endocrinol Metab. 2015;100(1):175–83.
Tanvig M, Vinter CA, Jørgensen JS, Wehberg S, Ovesen PG, Lamont RF, Beck-Nielsen H, Christesen HT, Jensen DM. Anthropometrics and body composition by dual energy X-ray in children of obese women: a follow-up of a randomized controlled trial (the Lifestyle in Pregnancy and Offspring [LiPO] study). PLoS One. 2014;9(2):e89590.
Bogaerts AF, Devlieger R, Nuyts E, Witters I, Gyselaers W, Van den Bergh BR: Effects of lifestyle intervention in obese pregnant women on gestational weight gain and mental health: a randomized controlled trial. Int J Obes (Lond). 2012. doi: 10.1038/ijo.2012.162. [Epub ahead of print].
Luoto R, Kinnunen TI, Aittasalo M, Kolu P, Raitanen J, Ojala K, Mansikkamäki K, Lamberg S, Vasankari T, Komulainen T, et al. Primary prevention of gestational diabetes mellitus and large-for-gestational-age newborns by lifestyle counseling: a cluster-randomized controlled trial. PLoS Med. 2011;8(5):e1001036. doi:10.1371/journal.pmed.1001036. Epub 2011 May 17.
Renault KM, Norgaard K, Nilas L, Carlsen EM, Cortes D, Pryds O, Secher NJ. The Treatment of Obese Pregnant Women (TOP) study: a randomized controlled trial of the effect of physical activity intervention assessed by pedometer with or without dietary intervention in obese pregnant women. Am J Obstet Gynecol. 2014;210(2):134 e131–139.
Acknowledgements
Not applicable.
Funding
No funding has been awarded for this proposed IPDMA.
JM Dodd is supported through a NHMRC Practitioner Fellowship (ID 627005).
RM Grivell is supported through a NHMRC Early Career Fellowship (ID 1073514).
Intramural funding provided by the Discipline of Obstetrics and Gynaecology, and the Robinson Research Institute, The University of Adelaide.
Availability of data and materials
The datasets analysed during the current study are available from the respective corresponding author on reasonable request.
Authors’ contributions
JMD, RMG, and JAO designed the study and search strategy extending from work through the i-WIP consortium. ST, EW, and BMW reviewed and provided expertise in methods for this review. RGM and JD designed and administered the Delphi Survey and together with CV, MT, DMJ, ABo, RD, RL, FM, KR, EC, NG, LP, ABr, ST, EW, BWM, and AD agreed on interpretation and selection of study outcomes. LG and JL designed the statistical analyses. All authors reviewed and provided comment on the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
The authors of individual studies included in this IPDMA consent to publication of these data. Written informed consent was obtained from all study participants for publication of reports pertaining to study participation.
Ethics approval and consent to participate
This IPDMA does not require ethics approval. All included studies were reviewed and approved by their respective human research ethics committees. The IPDMA will utilize de-identified data and report outcomes specified in individual studies.
Each participant in the individual trials comprising the i-WIP-3 collaboration has provided written informed consent to participate. The data are being used for the purposes for which they were originally collected and are made available by the lead investigators of each trial, who have agreed to a Memorandum of Understanding. The lead investigator of each individual trial remains the custodian of their original data.
Author information
Authors and Affiliations
Corresponding author
Additional file
Additional file 1:
PRISMA-P 2015 Checklist. (DOCX 30 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Dodd, J.M., Grivell, R.M., Louise, J. et al. The effects of dietary and lifestyle interventions among pregnant women who are overweight or obese on longer-term maternal and early childhood outcomes: protocol for an individual participant data (IPD) meta-analysis. Syst Rev 6, 51 (2017). https://doi.org/10.1186/s13643-017-0442-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13643-017-0442-6