Abstract
Introduction
The cerebrospinal fluid (CSF) biomarkers amyloid-β (Aβ), tau and phosphorylated tau (p-tau181) are now used for the diagnosis of Alzheimer’s disease (AD). Aβ40 is the most abundant Aβ peptide isoform in the CSF, and the Aβ 42/40 ratio has been proposed to better reflect brain amyloid production. However, its additional value in the clinical setting remains uncertain.
Methods
A total of 367 subjects with cognitive disorders who underwent a lumbar puncture were prospectively included at three French memory centers (Paris-North, Lille and Montpellier; the PLM Study). The frequency of positive, negative and indeterminate CSF profiles were assessed by various methods, and their adequacies with the diagnosis of clinicians were tested using net reclassification improvement (NRI) analyses.
Results
On the basis of local optimum cutoffs for Aβ42 and p-tau181, 22% of the explored patients had indeterminate CSF profiles. The systematic use of Aβ 42/40 ratio instead of Aβ42 levels alone decreased the number of indeterminate profiles (17%; P = 0.03), but it failed to improve the classification of subjects (NRI = −2.1%; P = 0.64). In contrast, the use of Aβ 42/40 ratio instead of Aβ42 levels alone in patients with a discrepancy between p-tau181 and Aβ42 led to a reduction by half of the number of indeterminate profiles (10%; P < 0.001) and was further in agreement with clinician diagnosis (NRI = 10.5%; P = 0.003).
Conclusions
In patients with a discrepancy between CSF p-tau181 and CSF Aβ42, the assessment of Aβ 42/40 ratio led to a reliable biological conclusion in over 50% of cases that agreed with a clinician’s diagnosis.
Similar content being viewed by others
Introduction
Dementia is a growing public health concern in aging populations. The number of people affected worldwide is set to reach 66 million by 2030 [1]. Alzheimer’s disease (AD) is the most frequent cause of dementia in the elderly. Clinical diagnosis is based on the presence of clinical symptoms, marked by a gradual onset of dementia in the presence of cognitive decline, when other putative disorders have been excluded [2]. Unfortunately, the accuracy of AD diagnosis based solely on clinical observation is associated with poor specificity. In most studies comparing clinical diagnosis with neuropathological findings, researchers have reported specificity lower than 70% [3]. Development of specific disease-modifying drugs and early diagnosis require an improvement in the accuracy of AD diagnosis.
The use of biomarkers has strengthened the link between clinical dementia and AD pathophysiology [2]. Currently, cerebrospinal fluid (CSF) biomarkers are commonly used in specialized memory clinics [4]. A characteristic feature of AD progression is a reduction in amyloid-β (Aβ) protein (that is, low CSF Aβ42 level) and an increase of neuronal degeneration biomarkers (that is, increase of CSF total tau and phosphorylated tau (p-tau181) levels) in CSF of subjects with AD [5]. The decrease in CSF Aβ42 levels appears to be an early phenomenon in AD progression and is evident over two decades prior to the first clinical sign [6]. Unfortunately, because CSF Aβ42 levels can also be low in non-AD patients, this biomarker alone is of limited use in a clinical setting [7,8]. The limited use of CSF biomarkers can lead to indeterminate results, revealing abnormal tau protein values and normal Aβ peptide levels or the inverse [2]. Furthermore, CSF biomarker results are also characterized by a large intersite variability [7] that requires the use of internally validated cutoff levels for each laboratory [9].
Aβ40 is the most abundant Aβ peptide isoform in the CSF. Compared with CSF Aβ42 levels alone, Aβ 42/40 ratio is suggested to account for the constitutive interindividual differences in total CSF Aβ peptide load between high- and low-amyloid-producing individuals [10]. The Aβ 42/40 ratio could also play an important role in Alzheimer’s disease pathogenesis [11]. However, the added value of the CSF Aβ40 level assessment remains controversial [12-15]. Recently, in a monocentric study, researchers reported that CSF Aβ 42/40 ratio may be of particular use in patients with ambiguous CSF results [16]. Therefore, the goal of our present study was to assess CSF Aβ 42/40 ratios and CSF Aβ42 levels alone to discriminate AD from non-AD patients in a large, prospective, multicentric population of patients. We hypothesized that the use of Aβ 42/40 ratio would reduce the frequency of inconclusive CSF results and would lead to a valid AD diagnosis.
Methods
Subjects
According to national recommendations, CSF analyses are routinely used during testing of patients with cognitive disorders in French memory centers [4,17]. Patients were recruited between 1 September 2012 and 1 September 2013 from three French clinical and research memory centers specializing in the care of patients with cognitive disorders. These three centers are based in Paris, Lille and Montpellier (the PLM Study) [18-20]. All patients who were prospectively included in the study had cognitive disorders and received a lumbar puncture. Patients with unknown clinical diagnoses were excluded. Patients with mild cognitive impairment (MCI) represented a heterogeneous group, including patients with and without AD-related brain lesions, and thus were excluded from this study.
All patients had a thorough examination, including clinical and neuropsychological evaluations, biological measurements and brain imaging. Patients with AD were included according to the criteria for probable AD as defined by the National Institute on Aging-Alzheimer’s Association [2]. On the basis of all available elements, which included the results for CSF biomarkers, patients were classified into two groups: AD and non-AD. Complex or unclear cases were discussed, and diagnoses were made by a multidisciplinary team of neurologists, geriatricians and neuropsychologists. Non-AD subjects included subjects with cognitive disorders other than AD (see Additional file 1), such as frontotemporal dementia, Lewy body disease, Parkinson’s disease, Creutzfeldt-Jakob disease and non-degenerative dementia (that is vascular dementia, alcohol-related dementia, normal pressure hydrocephalus, infectious disease and psychiatric disorders) [7].
This research study was approved by the local ethics committees of each hospital (see Additional file 2). All patients agreed to CSF collection, assessments and analyses by providing a written informed consent.
Cerebrospinal fluid analysis
Lumbar punctures were performed on fasting patients within 1 month following their clinical diagnosis, usually between 9:00 am and 12:00 pm. In an effort to reduce the intersite variability in CSF readings previously reported [7], all three centers used a common 10-ml polypropylene tube to collect the CSF (catalog number 62.610.201; Sarstedt, Nümbrecht, Germany) [21]. Each CSF sample was transferred at 4°C to the corresponding local laboratory within 4 hours after collection and was then centrifuged at 1,000 g for 10 minutes at 4°C. A small amount of CSF was used to perform routine analyses, including total cell count, bacteriological examination and total protein and glucose levels. The CSF was aliquoted in 0.5-ml polypropylene tubes and stored at −80°C to await further analysis. CSF Aβ40, Aβ42, total tau and p-tau181 were measured in each local laboratory using a commercially available sandwich enzyme-linked immunosorbent assay (INNOTEST; Fujirebio Europe NV, Gent, Belgium) according to the manufacturer’s instructions. Concentrations of total tau greater than 1,200 pg/ml were well above the detection limit and thus were not recalculated after dilution because of the constraints in the procedure. The biological teams involved in CSF analyses were blinded to the clinical diagnoses.
Cerebrospinal fluid cutoff determination and interpretation
CSF cutoffs used in the analyses were determined on the basis of the population included in the present study. We computed both overall and local cutoff receiver operating characteristic (ROC) curves using STATA software (v10, StataCorp, College Station, TX, USA). ROC curves were built for each biomarker by plotting sensitivity and 1 − specificity to discriminate AD from non-AD patients. Optimum cutoff values were determined using two methods: the highest Youden index (that is, sensitivity + specificity − 1) and lowest distance between ROC plot and point (0.1). We checked that both approaches led to similar findings, and the presented results correspond to the highest Youden index. STATA code used for the determination of optimum cutoff is detailed in the Additional file 3.
CSF results were defined as negative (that is, CSF p-tau181 below cutoff and CSF Aβ42 above cutoff) or positive (that is, CSF p-tau181 above cutoff and CSF Aβ42 below cutoff). An indeterminate CSF profile was defined by the association of one positive biomarker and one negative biomarker.
We chose to evaluate tau pathology based on CSF p-tau181 levels alone because p-tau181 and total tau levels were highly correlated in our sample (Pearson’s correlation coefficient = 0.87). Furthermore, p-tau181 has previously been reported to be more discriminant than total tau [22]. Analyses based on total tau led to findings and conclusions similar to those obtained with p-tau181.
Statistical analysis
The subjects’ characteristics are presented overall, by diagnosis (AD vs. non-AD) and by CSF collection centers. The various groups (diagnoses, centers) were compared using analysis of variance for continuous variables and χ2 test for categorical variables.
We computed ROC curves to evaluate the capacity of each CSF biomarker to discriminate AD from non-AD subjects. Analyses were performed in the overall study population and then stratified by centers. Optimum cutoffs for each biomarker were defined using the highest Youden index to discriminate in the best possible manner AD from non-AD subjects, thus maximizing sensitivity and specificity of the analyses based on ROC curve analyses. Then we used local optimum cutoffs for further analysis because intersite differences were present.
To evaluate the interest of ratio Aβ 42/40 versus CSF Aβ42 alone, we compared three methods to interpret CSF results:
-
1.
Method 1: interpretation based on CSF p-tau181 and on CSF Aβ42
-
2.
Method 2: interpretation based on CSF p-tau181 and on Aβ 42/40 ratio
-
3.
Method 3: a decisional algorithm based, in a first step, on CSF p-tau181 and on CSF Aβ42. Then, in case of discrepancy between p-tau181 and Aβ42, we used, in a second step, the Aβ 42/40 ratio in place of Aβ1–42
For all three methods, we first determined the percentage of AD, non-AD and indeterminate biological CSF profiles. Proportions of indeterminate profiles according to the methods were compared using the McNemar test. Then we used a net reclassification improvement (NRI) method to compare method 2 to method 1, and method 3 to method 1, among AD patients and non-AD patients (based on clinical diagnosis). Briefly, NRI is a statistical tool used to assess improvement in model performance offered by a new method of classification compared with a reference method [23,24]. The NRI compares the frequency of appropriate reclassification to inappropriate reclassification with the use of a new model of classification. The NRI is based on reclassification tables constructed separately for participants with or without the interest event (that is, diagnosis of AD or non-AD) and quantifies the correct movement in categories, up for events and down for non-events. Upward movement (up) is a change into a higher category, and downward movement (down) is a change into a lower category based on the new algorithm. The NRI is calculated as follows:
NRI = P (up | event) ‐ P (down | event) + P (down | non ‐ event) ‐ P (up | non ‐ event) [23]
The null hypothesis for NRI = 0 was tested using Z-statistics following McNemar asymptotic test for correlated proportions [22]. We provide an Excel file (Microsoft, Redmond, WA, USA) that allows the assessment of NRI with its standard error and its P-value [24].
All resulting P-values were two-tailed, and P ≤ 0.05 was considered statistically significant. Statistical analyses were performed using STATA version 10 and SAS version 9.2 (SAS Institute, Cary, NC, USA).
Results
In this study, we enrolled a total of 367 participants who received a lumbar puncture between 1 September 2012 and 1 September 2013. The study was conducted at three study centers (Paris, n = 82 subjects; Lille, n = 124 subjects; Montpellier, n = 161 subjects). The subjects’ characteristics are summarized in Table 1. Compared with non-AD subjects, participants with AD were older, were more likely to be female and had lower Mini Mental State Examination scores. Furthermore, subjects with AD had higher CSF tau and p-tau181 levels, lower CSF Aβ42 levels and lower CSF Aβ 42/40 ratios. CSF Aβ40 levels tended to be higher in patients with AD compared with non-AD patients (P = 0.06), but this relationship was attenuated after adjustment for age and sex (P = 0.19).
The percentages of patients with AD across centers ranged from 31% to 59% (Table 2). There were no significant differences in age or sex between AD and non-AD patients across the three sites. In patients with AD, the Aβ 42/40 ratio was the only comparable biomarker between the three sites, with a mean value ranging from 4.4% to 4.9% (P = 0.39).
The results of ROC curve analysis comparing AD with non-AD patients and optimum cutoffs are presented in Table 3. Area under the receiver operating characteristic curve (AUC) values for the various biomarkers can be used to discriminate between AD and non-AD patients. Across all three centers, tau (AUC range, 0.77 to 0.96) and p-tau181 levels (AUC range, 0.84 to 0.95) were more useful than Aβ42 levels (AUC range, 0.74 to 0.82) for AD diagnosis. Aβ 42/40 ratio outperformed Aβ42 in only one of the three centers, but not in the overall population (AUC = 0.81). Optimum cutoffs for CSF Aβ42 and for Aβ 42/40 ratio ranged from 737 pg/ml to 836 pg/ml and from 0.050 to 0.082, respectively.
Figure 1 illustrates the results of CSF biomarkers in the overall population according to CSF Aβ42 and CSF p-tau181 and per the global cutoffs based on the previous ROC curve analysis (overall population study). A total of 284 patients (77%) had determinate and definitive results using CSF Aβ1–42 and CSF p-tau181 levels (non-AD profile or AD-type profile), and 83 participants (23%) had indeterminate CSF results.
Scatterplot of cerebrospinal fluid amyloid-β42 and phosphorylated tau values in the overall study population. Black dots represent non-ambiguous cerebrospinal fluid (CSF) results (non-Alzheimer’s disease (non-AD) in the upper left quadrant, AD in the lower right quadrant). Gray dots represent indeterminate CSF results. Cutoffs for amyloid-β42 (Aβ42) and phosphorylated tau (p-tau181) were calculated in the overall population. Among the 367 patients, 83 (23%) had indeterminate CSF results.
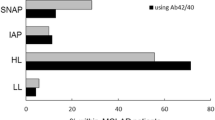
Figure 2 illustrates the biological interpretation of CSF results according to three methods. (1) Interpretation based on CSF p-tau181 and CSF Aβ42 cutoffs (method 1) leads to 82 patients (22.3%) with indeterminate results. (2) Using CSF p-tau181 and Aβ 42/40 ratio (method 2) could reduce the number of indeterminate profiles to 64 patients (17.4%; P = 0.03 compared with method 1). (3) Use of CSF p-tau181 and CSF Aβ42, and then Aβ 42/40 ratio in case of discrepancy (method 3), attenuated the number of indeterminate results to 38 patients (10.4%; P < 0.001 compared with method 1).
Biological interpretation of cerebrospinal fluid results according to different methods. Method 1: Cerebrospinal fluid (CSF) phosphorylated tau (p-tau181) and CSF amyloid-β42 (Aβ42). Method 2: CSF p-tau181 and Aβ 42/40 ratio. Method 3: First measure p-tau181 and CSF Aβ42, then use of Aβ 42/40 ratio instead of Aβ42 in case of discrepancy. Proportions of indeterminate profiles according to the methods were compared using the McNemar test.
Figure 3 presents reclassification tables, comparing method 1 with methods 2 and 3 in patients with AD and non-AD patients. The systematic use of Aβ 42/40 ratio did not improve the classification of patients and tended even to be slightly worse than CSF Aβ42 alone with a NRI equal to −2.1% (standard error (SE) = 0.05, P = 0.64). By contrast, the use of Aβ 42/40 ratio only in patients with discordant results between p-tau181 and Aβ42 (method 3) improved the classification of patients, with a NRI at 10.5% (SE = 0.04, P = 0.003) compared with method 1.
Reclassification tables of different methods of cerebrospinal fluid interpretation among patients with Alzheimer’s disease and non-Alzheimer’s disease patients. Method 1 (reference): cerebrospinal fluid (CSF) phosphorylated tau (p-tau181) and CSF amyloid-β42 (Aβ42). Method 2: CSF p-tau181 and Aβ 42/40 ratio. Method 3: First measure p-tau181 and CSF Aβ 42, then use Aβ 42/40 ratio instead of Aβ42 in case of discrepancy. Cells in green indicate an improvement compared with method 1, and cells in red indicate a worsening.
Discussion
In this clinically based, multicenter study, we evaluated the systematic assessment of CSF Aβ40 as part of a battery of CSF biomarkers measured in patients with cognitive disorders. We made the following observations:
-
The Aβ 42/40 ratio was the only biomarker that was consistent between centers in AD and non-AD patients. We may therefore hypothesize that this ratio is less sensitive to preanalytical and analytical conditions.
-
The systematic use of Aβ 42/40 ratio instead of Aβ42 decreased the number of indeterminate CSF profiles but failed to improve the classification of patients based on clinical diagnosis (NRI = −2.1%, P = 0.64).
-
A strategy based on the use of Aβ 42/40 ratio instead of Aβ42 in patients with initially discrepant results between p-tau181 and Aβ42 led to a reduction of the number of indeterminate CSF profiles (10% vs. 22%) and improved the classification of patients (NRI = 10.5%, P = 0.003).
Consequently, the assessment of Aβ 42/40 ratio could be helpful and can be recommended as a second step when the initial CSF profile remains indeterminate.
Researchers in several previous studies have investigated the use of Aβ 42/40 ratio to differentiate patients with AD from patients with other cognitive disorders, and the reported results are heterogeneous. In a previous study, researchers found that Aβ 42/40 ratio outperformed Aβ42 alone in differentiating AD from non-AD patients, but the diagnostic performance of the combination of CSF tau and CSF Aβ42 was not improved by the use of Aβ 42/40 ratio instead of Aβ42 alone [15]. In another study, using a subset of autopsy-confirmed diagnoses, investigators found no overall difference in AUC between Aβ 42/40 ratio and Aβ42 alone to differentiate AD from non-AD patients. Those authors showed that the use of Aβ 42/40 ratio improved diagnostic accuracy in patients with intermediate levels of phosphorylated tau [12]. In other previous studies, researchers also found that the assessment of CSF Aβ40 may help to discriminate between AD patients and patients with frontotemporal lobar degeneration [25] or dementia with Lewy bodies [26] and Parkinson’s disease with dementia [27]. In contrast, the authors of another previous report found that the diagnostic accuracy of CSF Aβ42 was not different from the Aβ 42/40 ratio to discriminate AD patients from control subjects [14]. Controversial data have also been reported in patients with MCI, with some studies revealing that the Aβ 42/40 ratio may be useful to predict dementia conversion [28], whereas another did not [13].
Our findings confirm and strengthen the results of a recent study in which researchers reported that the use of the Aβ 42/40 ratio may contribute to decreases in the proportion of indeterminate CSF profiles in the clinical setting [16].
The proportion of patients with AD varied greatly at the three centers, reflecting the differences in recruitment and practices of memory clinics. Despite significant intercenter differences in reporting CSF Aβ40 and CSF Aβ42 levels, the mean Aβ 42/40 ratios were comparable across the three centers, ranging from 0.044 to 0.049 in patients with AD. We therefore hypothesize that the use of the CSF amyloid ratio could contribute to decreased preanalytical and analytical sources of variability among centers. Interestingly, we found that optimal cutoff for the ratio in the overall study population was equal to 0.055, which was comparable to the 0.057 cutoff recently reported by another team in a monocentric study [12].
Very few data are available concerning indeterminate profiles of CSF biomarkers. In our study population, on the basis of routine clinical practice, this situation was not rare, being observed in 22% of the patients even after optimization procedures using local optimum cutoffs. We have shown that Aβ 42/40 ratio instead of Aβ42 leads to a clear biological conclusion in more than 50% of these indeterminate cases. Reclassification analyses also showed that this approach is more congruent with the diagnosis by clinicians.
This study has several strengths, including its large size, its multicentric and prospective design, and the use of a common CSF polypropylene tubing at each of the three centers to standardize CSF evaluation. In addition, we used a NRI method that compares different strategies of biomarker analyses and is more precise than traditional analyses based on ROC curves. The main limitation of the results is the lack of neuropathological validations. Also, clinicians were not blinded to CSF results prior to clinical diagnosis, which may generate a circular reasoning bias in our findings. The absence of a centralized measurement for CSF biomarkers is another limitation, owing to the persistence of an intersite variability despite the use of a common tubing to collect CSF. Furthermore, the non-AD group was heterogeneous and included patients with cognitive disorders, of both psychiatric and neurologic origins. However, our study was aimed at reflecting the standard practice at memory clinics. The wide variety of patients with a number of diseases reflects the broad spectrum of cognitive complaints referred to memory centers. Finally, this study excluded patients with MCI. Inclusion of these patients in future studies will help to determine the links between the amyloid ratio and the rate of conversion from MCI to AD.
Conclusions
Using a large prospective multicenter cohort of patients with cognitive disorders, we did not find an added value for the systematic assessment of the CSF Aβ 42/40 ratio. However, in cases of discrepancy between CSF p-tau and CSF Aβ42, the use of Aβ 42/40 ratio allowed reaching a biological conclusion in more than 50% of indeterminate results and improved the biological congruence with clinical diagnoses.
Abbreviations
- AD:
-
Alzheimer’s disease
- Aβ:
-
Amyloid-β protein
- Aβ40:
-
40–amino acid isoform of amyloid-β protein
- Aβ42:
-
42–amino acid isoform of amyloid-β protein
- AUC:
-
Area under the receiver operating characteristic curve
- CSF:
-
Cerebrospinal fluid
- MCI:
-
Mild cognitive impairment
- MMSE:
-
Mini Mental State Examination
- NRI:
-
Net reclassification improvement
- p-tau181:
-
tau phosphorylated at threonine 181
- ROC:
-
Receiver operating characteristic
- SD:
-
Standard deviation
- SE:
-
Standard error
References
Prince M, Bryce R, Albanese E, Wimo A, Ribeiro W, Ferri CP. The global prevalence of dementia: a systematic review and metaanalysis. Alzheimers Dement. 2013;9:63–75.e2.
McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack Jr CR, Kawas CH, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:263–9.
Beach TG, Monsell SE, Phillips LE, Kukull W. Accuracy of the clinical diagnosis of Alzheimer disease at National Institute on Aging Alzheimer Disease Centers, 2005–2010. J Neuropathol Exp Neurol. 2012;71:266–73.
Mouton-Liger F, Wallon D, Troussière AC, Yatimi R, Dumurgier J, Magnin E, et al. Impact of cerebro-spinal fluid biomarkers of Alzheimer’s disease in clinical practice: a multicentric study. J Neurol. 2014;261:144–51.
Rosén C, Hansson O, Blennow K, Zetterberg H. Fluid biomarkers in Alzheimer’s disease - current concepts. Mol Neurodegener. 2013;8:20.
Bateman RJ, Xiong C, Benzinger TL, Fagan AM, Goate A, Fox NC, et al. Clinical and biomarker changes in dominantly inherited Alzheimer’s disease. N Engl J Med. 2012;367:795–804.
Dumurgier J, Vercruysse O, Paquet C, Bombois S, Chaulet C, Laplanche JL, et al. Intersite variability of CSF Alzheimer’s disease biomarkers in clinical setting. Alzheimers Dement. 2013;9:406–13.
Dumurgier J, Laplanche JL, Mouton-Liger F, Lapalus P, Indart S, Prévot M, et al. The screening of Alzheimer’s patients with CSF biomarkers, modulates the distribution of APOE genotype: impact on clinical trials. J Neurol. 2014;261:1187–95.
Mattsson N, Andreasson U, Persson S, Carrillo MC, Collins S, Chalbot S, et al. CSF biomarker variability in the Alzheimer’s Association quality control program. Alzheimers Dement. 2013;9:251–61.
Wiltfang J, Esselmann H, Bibl M, Hüll M, Hampel H, Kessler H, et al. Amyloid β peptide ratio 42/40 but not Aβ42 correlates with phospho-Tau in patients with low- and high-CSF Aβ40 load. J Neurochem. 2007;101:1053–9.
Tanzi RE, Bertram L. Twenty years of the Alzheimer’s disease amyloid hypothesis: a genetic perspective. Cell. 2005;120:545–55.
Slaets S, Le Bastard N, Martin JJ, Sleegers K, Van Broeckhoven C, De Deyn PP, et al. Cerebrospinal fluid Aβ1-40 improves differential dementia diagnosis in patients with intermediate P-tau181P levels. J Alzheimers Dis. 2013;36:759–67.
Parnetti L, Chiasserini D, Eusebi P, Giannandrea D, Bellomo G, De Carlo C, et al. Performance of Aβ1-40, Aβ1-42, total tau, and phosphorylated tau as predictors of dementia in a cohort of patients with mild cognitive impairment. J Alzheimers Dis. 2012;29:229–38.
Schoonenboom NS, Mulder C, Van Kamp GJ, Mehta SP, Scheltens P, Blankenstein MA, et al. Amyloid β 38, 40, and 42 species in cerebrospinal fluid: more of the same? Ann Neurol. 2005;58:139–42.
Spies PE, Slats D, Sjögren JM, Kremer BP, Verhey FR, Rikkert MG, et al. The cerebrospinal fluid amyloid β42/40 ratio in the differentiation of Alzheimer’s disease from non-Alzheimer’s dementia. Curr Alzheimer Res. 2010;7:470–6.
Sauvée M, DidierLaurent G, Latarche C, Escanyé MC, Olivier JL, Malaplate-Armand C. Additional use of Aβ42/Aβ40 ratio with cerebrospinal fluid biomarkers P-tau and Aβ42 increases the level of evidence of Alzheimer’s disease pathophysiological process in routine practice. J Alzheimers Dis. 2014;41:377–86.
Troussière AC, Wallon D, Mouton-Liger F, Yatimi R, Robert P, Hugon J, et al. Who needs cerebrospinal biomarkers? A national survey in clinical practice. J Alzheimers Dis. 2014;40:857–61.
Gabelle A, Dumurgier J, Vercruysse O, Paquet C, Bombois S, Laplanche JL, et al. Impact of the 2008–2012 French Alzheimer Plan on the use of cerebrospinal fluid biomarkers in research memory center: the PLM Study. J Alzheimers Dis. 2013;34:297–305.
Dumurgier J, Gabelle A, Vercruysse O, Bombois S, Laplanche JL, Peoc’h K, et al. Exacerbated CSF abnormalities in younger patients with Alzheimer’s disease. Neurobiol Dis. 2013;54:486–91.
Lehmann S, Dumurgier J, Schraen S, Wallon D, Blanc F, Magnin E, et al. A diagnostic scale for Alzheimer’s disease based on cerebrospinal fluid biomarker profiles. Alzheimers Res Ther. 2014;6:38.
Lehmann S, Schraen S, Quadrio I, Paquet C, Bombois S, Delaby C, et al. Impact of harmonization of collection tubes on Alzheimer’s disease diagnosis. Alzheimers Dement. 2014;10(5 Suppl):S390–S394.e2.
Pencina MJ, D’Agostino Sr RB, D’Agostino Jr RB, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. 2008;27:157–72.
Pencina MJ, D’Agostino Sr RB, Steyerberg EW. Extensions of net reclassification improvement calculations to measure usefulness of new biomarkers. Stat Med. 2011;30:11–21.
Centre Mémoire de Ressources et de Recherche, Paris Nord Ile-de-France. Net Reclassification Improvement (NRI) calculator. Retrieved from http://www.parisnord.org/net-reclassification-improvement-excell-calculator.html. Accessed 24 Mar 2015.
Verwey NA, Kester MI, van der Flier WM, Veerhuis R, Berkhof H, Twaalfhoven H, et al. Additional value of CSF amyloid-β40 levels in the differentiation between FTLD and control subjects. J Alzheimers Dis. 2010;20:445–52.
Bibl M, Mollenhauer B, Esselmann H, Lewczuk P, Trenkwalder C, Brechlin P, et al. CSF diagnosis of Alzheimer’s disease and dementia with Lewy bodies. J Neural Transm. 2006;113:1771–8.
Nutu M, Zetterberg H, Londos E, Minthon L, Nägga K, Blennow K, et al. Evaluation of the cerebrospinal fluid amyloid-β1-42/amyloid-β1-40 ratio measured by α-LISA to distinguish Alzheimer’s disease from other dementia disorders. Dement Geriatr Cogn Disord. 2013;36:99–110.
Hansson O, Zetterberg H, Buchhave P, Andreasson U, Londos E, Minthon L, et al. Prediction of Alzheimer’s disease using the CSF Aβ42/Aβ40 ratio in patients with mild cognitive impairment. Dement Geriatr Cogn Disord. 2007;23:316–20.
Acknowledgments
The authors thank the other members of the teams for their contributions to this study: Dr Florence Lebert, Dr Marie-Anne Mackowiak, Dr Vincent Deramecourt, Dr Adeline Rollin-Sillaire, Dr Pascaline Cassagnaud, Dr Karim Bennys, Dr Christian Geny, Dr Eric Thouvenot, Dr Sarah Benisty, Dr Valérie Ducasse, Dr Claire Kiffel and all the neuropsychologists. The authors warmly thank Professors Joël Ménard, Hervé Maisonneuve, Jean Marie Goehrs and Patrick Trunet for their very helpful advice and for revising the manuscript. The authors also thank Sylvie Ledoux and the Fondation Plan Alzheimer for logistic support.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
JD processed and analyzed the data, prepared the results presentation and drafted various versions of the manuscript. SS participated in the research project (conception, organization, execution) and in manuscript preparation (review and critique). AG participated in the research project (conception, organization, execution) and in manuscript preparation (review and critique). OV participated in the research project (conception, organization, execution) and in manuscript preparation (review and critique). SB participated in the research project (conception, organization, execution) and in manuscript preparation (review and critique). JLL participated in the research project (conception, organization, execution) and in manuscript preparation (review and critique). KP participated in the research project (conception, organization, execution) and in manuscript preparation (review and critique). BS participated in the research project (conception, organization, execution) and in manuscript preparation (review and critique). KVK participated in the research project (interpretation of data, execution) and in manuscript preparation (review and critique). CD participated in the research project (conception, organization, execution) and in manuscript preparation (review and critique). FP participated in the research project (conception, organization, execution) and in manuscript preparation (review and critique). JT participated in the research project (conception, organization, execution) and in manuscript preparation (review and critique). JH participated in the research project (conception, organization, execution) and in manuscript preparation (review and critique) and helped draft the manuscript. CP participated in the research project (conception, organization, execution) and in manuscript preparation (review and critique) and helped draft the manuscript. SL helped with data analysis, participated in the research project (conception, organization, execution) and in manuscript preparation (review and critique). All authors edited and approved the final version of the manuscript.
Additional files
Additional file 1:
List of local ethics committees that approved the research study.
Additional file 2:
STATA code used for determination of local optimum cutoffs.
Additional file 3:
Characteristics of non-AD patients.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Dumurgier, J., Schraen, S., Gabelle, A. et al. Cerebrospinal fluid amyloid-β 42/40 ratio in clinical setting of memory centers: a multicentric study. Alz Res Therapy 7, 30 (2015). https://doi.org/10.1186/s13195-015-0114-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13195-015-0114-5