Abstract
Background
Colorectal cancer (CRC) appear to arise from precursor lesions in a well-characterized adenoma-carcinoma sequence. Significant efforts have been invested to develop biomarkers that identify early adenocarcinomas and adenomas with high-grade dysplasia, since these are believed to harbor a particularly high risk for malignant transition and thus require resection. Promoter methylation of SEPT9 and SHOX2 has been suggested as a biomarker for various solid malignant tumors. Hence, the present study aimed to test their biomarker potential in CRC and precursor lesions.
Results
Assessment of promoter methylation of SEPT9 distinguished adenomas and CRC from controls as well as advanced from non-advanced adenomas (all p < 0.001). Correspondingly, SHOX2 methylation levels in adenomas and colorectal carcinomas were significantly higher compared to those in normal control tissues (p < 0.001). Histologic transition from adenomas to CRC was paralleled by amplification of the SEPT9 gene locus.
Conclusions
SEPT9/SHOX2 methylation assays may help to distinguish colorectal cancer and adenomas from normal and inflammatory colonic tissue, as well as advanced from non-advanced adenomas. Further studies need to validate these findings before introduction in clinical routine.
Similar content being viewed by others
Background
Colorectal cancer (CRC) is one of the most common and intensively studied cancer entities worldwide [1]. Although its molecular pattern is to a certain extent heterogeneous, more than 80 % of sporadic CRC appear to arise from precursor lesions [2]. The “adenoma-carcinoma sequence” [3] reflects this transition with a genetic characteristic, e.g., mutations in TP53, KRAS, and APC, [4] and histopathologic alterations [5, 6]. The evolving knowledge about precancerous lesions of CRC, the oftentimes slow progression towards malignant transformation, and a tremendously better prognosis for early detected and treated CRCs make this cancer entity particularly attractive for screening strategies [7]. Owing to multimodal therapy regimes, improved surgical techniques, and screening programs, incidence of CRC has steadily decreased over the last decades [8, 9]. Despite this significant success, population’s enrollment in recommended screening programs is difficult [10] and significant efforts have been invested in the development of non-invasive diagnostic tests. Nonetheless, colonoscopy remains the non-replaceable gold standard in every CRC screening program [11, 12].
Epigenetic changes to genomic tumor DNA are biostable and often cancer-specific alterations that are therefore issue of numerous ongoing research projects worldwide [13]. Our and other groups established differential methylation-specific qPCR assays of the stature homeobox 2 (SHOX2) and septin 9 (SEPT9) in various cancer entities with possible biomarker properties for early detection and response prediction strategies [14]. For example, our team previously used a combined assay to measure SHOX2 and SEPT9 promoter methylation for the discrimination between benign and malignant pleural effusions [15]. Promoter methylation of SEPT9, a gene encoding for a GTP-binding protein with various functions in formation and control of the cytoskeleton, proved to be present in >90 % of CRC specimens (mean methylation level 26 %, range 0–89 %) [16–18]. Furthermore, SEPT9 DNA methylation in blood plasma was successfully validated in a large prospective trial including ~8000 asymptomatic subjects, undergoing routine colonoscopy (ClinicalTrials.gov Identifier: NCT00855348) [19]. Consequently, SEPT9-based diagnostic tests for colorectal cancer screening are available to patients in Europe and the USA as CE-marked In Vitro Diagnostics (CE-IVDs) and Laboratory Developed Tests (LDTs). Very recently, the American Food and Drug Administration (FDA) approved the commercial SEPT9 methylation assay, “Epi proColon®,” as a blood-based in vitro diagnostic (IVD) test for screening of CRC. However, the SEPT9 methylation pattern of adenomas has only been studied in a small amount of studies [20–24]. It is known today that certain types of adenomas harbor an increased risk for malignant transformation [25] and that adenomatous subtypes carry different epigenetic profiles [26]. Up-to-date detailed information about the SEPT9 methylation status in different types of adenomatous polyps is still fragmentary.
SHOX2 harbors two large CpG islands, located at the 3′ and the 5′ end of the gene, and is involved in limb formation and cardiac development [27, 28]. So far, the SHOX2 DNA methylation status has mainly been evaluated for its value in the detection of lung cancer with reasonable success [29–34]. More than 90 % of histologically confirmed lung cancer patients showed a hypermethylation of this gene locus in comparison to normal tissue [35]. Additionally, the SHOX2 methylation status showed promising results in other cancer types [15, 36]. In order to probe the apparently broad utility of SHOX2 as a biomarker in CRC, this target was included in the present study.
Results
Stepwise increase of SEPT9 methylation from non-cancerous to cancerous tissue
In the Triplex assay, SEPT9 promoter methylation levels showed a gradual increase from the control group (4.4 % ± 9.9), over non-advanced (N-AA, 72.7 % ± 63.3) and advanced adenomas (AA, 150.2 % ± 110.05), to CRC (294.8 % ± 219.2, Fig. 1a). The Triplex SEPT9 methylation assay was able to differentiate between CRCs vs. controls (p < 0.001), CRCs vs. adenomas (p = 0.001) and CRC vs. AA (p < 0.001), CRC vs. N-AA (p < 0.001). Additionally, AA showed a hypermethylation compared to N-AA (p < 0.001) or control (p < 0.001).
SEPT9 methylation quantified with Triplex and QM assays, respectively, comparing the different subgroups (control vs. non-advanced vs. advanced adenomas vs. CRC). Comparison of different SEPT9 methylation levels obtained from the a Triplex assay (control n = 62, N-AA n = 24, AA n = 48, CRC n = 25) and b QM assay (control n = 63, N-AA n = 24, AA n = 48, CRC n = 28). **p < 0.001 marks significant differences in methylation levels between the indicated subgroups, and *p < 0.05 marks significant differences in methylation levels between the indicated subgroups. N-AA non-advanced adenomas, AA advanced adenomas
Receiver operating characteristic (ROC) analyses showed that SEPT9 hypermethylation was able to distinguish between CRC vs. control (AUC = 0.96, 95 % CI = 0.90–1.00, p < 0.001) and adenomas vs. control (AUC = 0.97, 95 % CI = 0.93–1.00, both p < 0.001; Fig. 2a, b).
In total, 59/166 (35 %) specimens showed a SEPT9 methylation level ≥100 % (highest methylation level of 789 %) and again a stepwise increment was noted from control to CRC. In the CRC group, 19/25 (76 %) showed a methylation level ≥100 %, whereas 39/75 (52 %) adenomas and 0/62 controls had a methylation level ≥100 %.
The QM assay also showed an increase in the SEPT9 methylation level from the control group (2.4 % ± 3.2), over adenomas (55.8 % ± 29.3), to CRC (60.9 % ±26.9). N-AA (36.7 ± 26.6 and AA 67.5 ± 24.6) also showed an increase in the SEPT9 methylation level (p < 0.001, Fig. 1b). Although the QM assay showed different methylation levels between CRC vs. controls (p < 0.001), CRC vs. N-AA (p = 0.002), and AA vs. controls (p < 0.001), this assay was not able to differentiate between CRC vs. AA (p = 0.29) and CRC vs. adenomas (p = 0.43).
ROC analyses showed that SEPT9 hypermethylation was able to distinguish between CRC vs. control (AUC = 0.95, 95 % CI = 0.88–1.00, p < 0.001) and adenomas vs. control (QM: AUC = 0.96, 95 % CI = 0.93–0.99, p < 0.001; Fig. 2a, b).
SHOX2 methylation shows a gradual increase from non-cancerous tissues to CRC
As shown for the SEPT9 gene locus, SHOX2 showed a gradual step-up in the methylation level from control (1.3 % ± 1.5), over N-AA (26.3 % ± 29.6) and AA (46.7 % ± 44.9), to CRC (65.7 % ± 35.4), in the Triplex assay. Adenomas showed a SHOX2 methylation level of 40.2 % ± 40.6 without separation in N-AA and AA. SHOX2 methylation level was able to discriminate CRC vs. control (p < 0.001), CRC vs. N-AA (p = 0.01), N-AA vs. AA (p = 0.025), AA vs. control (p < 0.001), and N-AA vs. control (p < 0.001). Nonetheless, this assay was not able to distinguish between CRC vs. AA (p = 0.44) and CRC vs. adenoma (p = 0.12, Fig. 3).
SHOX2 methylation quantified with Triplex and QM assays, respectively, comparing the different subgroups (control vs. adenomas vs. CRC). Comparison of different SHOX2 methylation levels obtained from the a Triplex assay (control n = 62, adenomas n = 75, CRC n = 25) and the b QM assay (control n = 63, adenomas n = 75, CRC n = 28) for the three subgroups. **p < 0.001 marks significant differences in methylation levels between the indicated subgroups, and *p < 0.05 marks significant differences in methylation levels between the indicated subgroups
ROC analyses showed that SHOX2 hypermethylation was able to discriminate between CRC vs. controls (AUC = 0.91, 95 % CI = 0.81–1.00, p < 0.001) and adenomas vs. controls (AUC = 0.88, 95 % CI = 0.82–0.94, p < 0.001, Fig. 2c, d). However, SHOX2 methylation assay failed in the differentiation between CRC and adenoma (AUC = 0.60, 95 % CI = 0.48–0.74, p = 0.095).
In total, 11/166 (7 %) specimens showed a SHOX2 methylation level in the Triplex assay ≥100 % (highest methylation level of 179 %). There was no difference between the groups with 3/27 (11 %) in the CRC group, 8/75 (11 %) in the adenoma group, and 0/63 in the control group.
The QM assay also showed an increase of the SHOX2 methylation level from controls (1.5 % ± 2.3), over N-AA (44.3 % ± 36.3) and AA (59.5 % ± 37.2), to CRC (65.7 % ± 35.4). Adenomas showed a SHOX2 methylation level of 55.3 % ± 36.9 without separation in N-AA and AA. SHOX2 methylation level was able to discriminate CRC vs. control (p < 0.001), CRC vs. N-AA (p = 0.036), AA vs. control (p < 0.001), and N-AA vs. control (p < 0.001). Nonetheless, this assay was not able to separate CRC from N-AA, AA, or adenomas (all p > 0.05) or AA from N-AA (p > 0.05, Fig. 3).
ROC analyses showed that SHOX2 hypermethylation was able to discriminate between CRC vs. controls (AUC = 0.88, 95 % CI = 0.77–0.99, p < 0.001) and adenomas vs. controls (AUC = 0.90, 95 % CI = 0.85–0.95, p < 0.001, Fig. 2c, d). However, SHOX2 methylation assay failed in the differentiation between CRC and adenoma (AUC = 0.56, 95 % CI = 0.43–0.69, p = 0.33).
SEPT9 and SHOX2 methylation status in advanced adenomas
For three patients with colorectal adenoma, no information regarding size and grade of dysplasia could be retrieved, narrowing the amount of individuals in this analysis to 72.
In correlation to the stepwise increase of SEPT9 and SHOX2 methylation level, the adenoma group was evaluated for other characteristics with known potential for supporting a malignant transition.
In the Triplex assay, size ≥10 mm was significantly correlated with the methylation level of SEPT9 (ρ = 0.40, p < 0.001), but showed no difference in the methylation level of SHOX2 (ρ = 0.21, p = 0.083). Interestingly, those adenomas larger than ≥10 mm in size (n = 48) showed more frequently SEPT9 methylation levels ≥100 % than adenomas ≤10 mm (n = 24) (33/48 (68 %) vs. 6/24 (25 %), p < 0.001). No difference between small and large adenomas was found regarding SHOX2 methylation levels ≥100 % (p = 0.19). Correspondingly, the highest grade of epithelial dysplasia (D1-3) [37] is correlated with significantly higher methylation of SEPT9 (ρ = 0.24, p = 0.047), but not of SHOX2 (ρ = −0.06, p = 0.58).
In the QM methylation assay, size ≥10 mm was correlated with the methylation level of SEPT9 (ρ = 0.48, p < 0.001) and SHOX2 (ρ = 0.24, p = 0.047). The highest grade of epithelial dysplasia (D1-3) [37] showed a trend of higher methylation of SEPT9 (ρ = 0.23, p = 0.056), but not of SHOX2 (ρ = −0.06, p = 0.60). Adenomas with a size ≥10 mm had a higher SEPT9 methylation level (67.5 vs. 36.7 %, p < 0.001) compared to small adenomas, but no difference was found in SHOX2 (59.5 vs. 44.3 %, p = 0.10).
SEPT9 and SHOX2 methylation levels in adenoma subtypes
Regarding the methylation status of the SEPT9 gene locus, (tubulo-)villous adenomas showed the highest methylation levels of all adenomas, irrespective of assay type. Consequently, villous adenomas showed a significant hypermethylation of SEPT9 (Triplex assay) in comparison to serrated adenomas (164.9 vs. 70.3 %, p = 0.022, Fig. 4). All other types of adenomas showed no difference in methylation using the Triplex assay. According to results from the Triplex assay, QM assay analysis also showed a significant hypomethylation of serrated adenomas compared to villous adenomas (QM 34.2 vs. 63.7 %, p = 0.003; Triplex 70.3 vs. 164.9 %, p = 0.022) and tubulovillous adenomas (QM 34.2 vs. 74.2 %, p < 0.001; Triplex 70.3 vs. 152.0 %, p = 0.051). Additionally, tubulovillous in comparison to tubular adenomas showed a different SEPT9 methylation level (QM 74.2 vs. 49.8 %, p = 0.029) (Fig. 4).
SEPT9 methylation quantified with QM and Triplex assays, respectively, comparing different adenoma subtypes. Comparison of different SEPT9 methylation levels in the a Triplex and b QM assays for the four adenomatous subgroups (tubular n = 16, tubulovillous n = 21, villous n = 18, serrated n = 20). **p < 0.001 marks significant differences in methylation levels between the indicated subgroups, and *p < 0.05 marks significant differences in methylation levels between the indicated subgroups
In contrast to SEPT9, methylation levels of the SHOX2 gene locus revealed no difference between the various types of adenomas in both methylation assays (QM: villous vs. tubulovillous, villous vs. serrated, and villous vs. tubular, all p > 0.5; tubulovillous vs. tubular, p = 0.26 and serrated vs. tubular, p = 0.082) (Triplex: villous vs. tubulovillous, villous vs. serrated, villous vs. tubular, and serrated vs. tubular, all p > 0.5; tubulovillous vs. tubular, p = 0.20) (Fig. 5).
SHOX2 methylation quantified with QM and Triplex assays, respectively, comparing different adenoma subtypes. Comparison of different SHOX2 methylation levels obtained from the a Triplex and b QM assays for the four adenomatous subgroups (tubular n = 16, tubulovillous n = 21, villous n = 18, serrated n = 20). No significance level p < 0.05 has been reached in these assays
Microsatellite instability
No correlation between any type of microsatellite instability (MSI) (MLH1, PMS2, MSH2, and MSH6), amplification of SEPT9 and SHOX2, and clinical parameters were found (all p > 0.5).
Discussion
Large screening programs have decreased the incidence of CRC [8, 9], but low compliance rates especially regarding preventive colonoscopy hamper a maximum success of modern primary prevention strategies [11]. The principle of “tailored screening” may improve screening effectiveness by stratification into risk tiers [38]. Therefore, entirely non-invasive early detection tests for CRC are urgently needed.
Epigenetic alternations of the SEPT9 gene locus were previously described in minor series of tissue from colorectal adenomas [20–23] or blood samples [24, 39]. The presented comprehensive data confirmed previous findings and highlight the relevance of SEPT9 methylation in these lesions. Moreover, it was revealed that the assessment of promoter methylation of SEPT9 as well as SHOX2 may actually help distinguish CRC and adenomas from normal epithelium without dysplasia. These results are in line with Tänzer et al. who found a higher frequency of SEPT9 and ALX4 DNA methylations in plasma of AA compared to healthy controls [23]. On top of that, the methylation status of SEPT9 as quantified with our Triplex assay was able to distinguish between adenomas vs. CRC and AA vs. N-AA. Despite their statistical significance, the methylation level of both genes within the subgroup showed a scattered and partly overlapping distribution, elevating the risk of false positive or negative results. These observations are in line with the finding that epigenetic changes resemble an early event in the carcinogenesis of CRC [40, 41]. In accordance, genome-wide comprehensive methylation analysis of adenomas and CRC tissue revealed accumulation of epigenetic alternations in the progression from early adenomas towards invasive adenocarcinomas [42, 43]. Although, advanced adenomas are believed to harbor an increased potential for malignant transformation (see [44] and [25]), a direct proof of malignant transformation of advanced adenomas or of a certain histologic subtype remains somewhat elusive.
Interestingly, a stepwise increase of the SEPT9 methylation level from controls over not-advanced adenomas to advanced adenomas and invasive adenocarcinoma could be observed. This may explain false positive test results of the Epi proColon® test indicating methylated DNA segments in the SEPT9 region in the absence of an invasive CRC. SEPT9 may therefore potentially be used as an ancillary marker in the identification of advanced adenomas in case of difficulties with histologic diagnosis of a colorectal biopsy (i.e., due to cautery artifacts). Additionally, the presented data support a future inclusion of SEPT9 and SHOX2 in methylation biomarker panels to support the diagnosis of CRC, though both markers have to be validated in a large prospective trial. By combining these and other markers, overlapping results especially between AA and CRC may be minimized.
Surprisingly, >50 % of SEPT9 Triplex methylation levels in CRC and adenomas showed a value exceeding 100 %, technically reasoned by a distant location of the reference gene (ACTB at chromosome 7) and the analyzed gene loci (SEPT9 gene at chromosome 17 and SHOX2 at chromosome 3q) [15]. Hence, higher methylation values in comparison to QM assay may be due to focal amplification of the SEPT9 gene locus and/or a deletion of the reference gene (ACTB). A SEPT9 amplification later during carcinogenesis is supported by the observation that especially advanced adenomas and carcinomas showed a level >100 % in the Triplex assay. These findings are in congruence with the results from Ben-David et al. who found that genes, which have been up-regulated in early adenomas, showed a tendency for amplification in later stages of colorectal carcinogenesis [45]. Taken together, one may carefully speculate that promoter hypermethylation of SEPT9 triggers a focal amplification that may foster a malignant transition from adenoma to invasive carcinoma. This mirrors the assumption of Saha et al. and Bardelli et al. that gene amplification is attributed to play a role in stage transition of CRC [46, 47]. Concordantly, SEPT9 amplification has only been identified in advanced breast cancer patients [48] and in vitro [49], while early localized tumors showed no SEPT9 amplification. Additionally, the same group was able to identify a worse survival in endometrial adenocarcinoma, which shows a copy number variation (CNV) of SEPT9 [50]. In contrast to this hypothesis, SEPT9 amplification was only found in 0.4 % of CRC in a cohort of 257 CRC patients and in 2/615 CRC cases of the TCGA data repository (0.3 %) [4]. If the above assumptions are proven true, SEPT9 may be an excellent plasmatic biomarker. Because, due to DNA amplification, the total number of tumor DNA alleles in plasma including their specific epigenetic SEPT9 alteration may be easier to detect among background DNA. This phenomenon has already been evidenced for SHOX2 in squamous cell lung cancer [34]. Another possible explanation for this phenomenon was hypothesized to be a MSI, which is known for causing hyper-mutated and epigenetically altered genomes [4]. However, no correlation between MSI and amplifications of SEPT9 and SHOX2 or clinical parameters were found in the present study.
Overall, SEPT9 methylation showed a better performance than SHOX2 in distinguishing the different study groups. This finding is in line with results about the potential of plasmatic free-circulating tumor DNA and tissue SEPT9 methylation [17–19, 51–53], although sensitivity (52–94 %) and specificity (88–95 %) vary greatly between the studies [17, 18, 51, 54]. This variability may be attributed to different testing methods or common pre-existing conditions like high age, gender, and comorbidities and have to be interpreted with caution [53, 55].
The present study has several limitations. For example, only a small series was included and analyzed in a retrospective fashion hampering statistical power and lowering the evidence level. Furthermore, methylation assays have only a limited suitability to detect CNV, and more sensitive assays (e.g., FISH, CGH, or next-generation sequencing) have to validate the data.
Conclusions
In conclusion, SEPT9 or SHOX2 methylation may be auxiliary biomarkers for the differentiation of CRC and advanced adenomas to non-advanced adenomas and normal tissue. Ideally, both markers should be integrated into a marker panel for CRC screening and validated in a large prospective trial. The investigations suggest that CNV of SEPT9 may contribute to a malignant transition from adenomas into advanced adenomas and adenocarcinomas. Further studies with CNV sensible assays are needed to elucidate the distinct role of these gene loci in the carcinogenesis of CRC and their potential as biomarker.
Methods
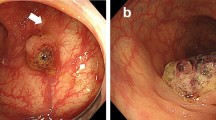
Patient samples
The study was approved by the Institutional Review Board (IRB) of the University Hospital of Bonn (Number: 222/13). Formalin-fixed, paraffin-embedded (FFPE) tissue specimens from 166 patients, treated or diagnosed at the University Hospital of Bonn academic hospitals between 2002 and 2013, were included. The study group included various non-invasive epithelial lesions including tubular adenomas, tubulovillous adenomas, villous adenomas, and serrated adenomas. Furthermore, sporadic colorectal cancer were included. Patients with a history of familial adenomatous polyposis (FAP), Lynch syndrome, or other second primary malignancy were not included. Additionally, patients with Crohn’s disease showing high-grade dysplasia in the resected specimen or in any biopsy taken at time of admission were excluded from the study. All specimens were histologically diagnosed by an experienced pathologist blinded to the patient’s history. Histologic classification was performed according to the most recent recommendations by the World Health Organization [56] and the latest TNM classification [57]. Advanced adenomas were defined as adenomatous polyps with a size ≥10 mm, ≥25 % of villous features, or a high-grade dysplasia [58–61].
Patient characteristics
The study cohort comprised tissue specimens from 166 patients (102 ♂, 64 ♀) with a mean age of 67 years (range 38–91). Age and gender were distributed equally in the following groups (all p > 0.5). The CRC group embodied 28 patients (18 ♂, 10 ♀) with a mean age of 69 years (range 42–90). This group included 7 stage I, 7 stage IIa, 3 stage IIb, 3 stage IIIa, 1 stage IIIb, 4 stage IIIc, and 3 stage IV CRCs. The adenoma group contained 75 individuals (45 ♂, 30 ♀) with a mean age of 68 years (range 38–89). Sixteen of the adenomas were described as tubular, 21 as tubulovillous, 18 as villous, and 20 as serrated adenomas. Twenty-four of 75 adenomas (32 %) measured <1 cm, and 48/75 (64 %) had a size >1 cm, while 3 datasets were missing (4 %). The mean size of adenomas was 2 cm, the median 1.5 cm (range 0.3–8 cm). Fifty-three adenomas of 75 (70.7 %) showed a low or moderate grade of dysplasia, 19/75 (25.3 %) showed high-grade dysplasia, while 3 datasets were missing (4 %). The control group comprised of 63 patients (39 ♂, 24 ♀) with a mean age of 66 years (range 39–91). This group contained 34 normal adjunct tissue specimens (NAT), 23 specimens diagnosed with Crohn’s disease and admitted for surgical colon resection because of obstruction, abscesses, or fistula and 6 specimens with colonic diverticulosis.
Valid Triplex assay measurements were obtained from 25 CRCs; 75 adenomas, including 16 tubular, 21 tubulovillous, 18 villous, and 20 serrated adenomas; and 62 controls.
Valid QM assay measurements were obtained from 28 CRC, 75 adenoma (16 tubular, 21 tubulovillous, 18 villous, and 20 serrated adenomas), and 63 control specimens.
TCGA data
Data plots for CNV were conducted using cBioPortal (http://www.cbioportal.org/index.do) [62, 63] and the gene-centric GISTIC analyses provided at http://www.broadinstitute.org/tcga/home [64]. These results are in whole based upon data generated by the TCGA Research Network (http://cancergenome.nih.gov/).
DNA extraction and methylation analysis
DNA extraction was performed using the Bisulfite All-In-One Kit (innuCONVERT, Analytik Jena, Germany). The detailed protocol is described elsewhere [65, 66]. Locus-specific analyses of DNA methylation patterns were performed using two different PCR methods of methylation analyses for each specimen: (1) Triplex methylation-specific qPCR (Triplex qMSP) [15] and (2) quantitative methylation PCR (QM PCR) [67].
SHOX2/SEPT9/ACTB Triplex assay
As previously described, a methylation-specific Triplex qPCR assay was used [15]. It quantifies the number of methylated SHOX2 and SEPT9 alleles, referred to total DNA copy numbers. The total DNA copy number was quantified using a qPCR assay targeting the β-actin (ACTB) gene locus comprising no CpG sites [15]. A calibrator sample (bisulfite-converted artificially methylated DNA) was used in order to allow for an accurate quantification as previously described [15].
QM assay
A modified quantitative methylation real-time PCR, called QM PCR assay [67], was used. It allows a simultaneous amplification of methylated and unmethylated alleles in a single tube. The composition of the PCR buffer has been described earlier [34]. Primers (SHOX2-forward: cctcctaccttctaaccc, SHOX2-reverse: gttttttggatagttaggtaat, SEPT9-forward: aaataatcccatccaacta, SEPT9-reverse: gttgtttattagttattatgt) and probes (SHOX2-methylated: 6-FAM-ctcgtacgaccccgatcg-BBQ650, SHOX2-unmethylated: HEX-tactcatacaaccccaatcaaaca-BHQ1, SEPT9-methylated: 6-FAM-ttaaccgcgaaatccgac-BHQ1, SEPT9-unmethylated: HEX-acattaaccacaaaatccaac-BHQ1) were applied in a final concentration of 0.6 μM each. PCR was performed with an AB 7500 Fast Real-Time PCR System (Life Technologies Corporation, Carlsbad, CA, USA) using the following temperature profile: 15 min at 95 °C of initial denaturation followed by 45 cycles with 15 s, 95 °C and 60 s, 60 °C. As a calibrator sample for the QM PCR assay, a 50 % mixture of bisulfite-converted artificially methylated DNA (CpGenome™ Universal Methylated DNA; Merck Millipore, Darmstadt, Germany) and unmethylated DNA (NW Andrology & Cryobank Inc., Spokane, WA, USA) was used.
Calculation of methylation levels
The calibrator and all the samples were analyzed in triplicate (Triplex assay) and in duplicate (QM assay), respectively. The mean average of the CT values was calculated and used for further analysis. Previously described adapted ∆∆CT methods were applied to determine a relative methylation value from the QM assay [68] and the Triplex assay [15] measurements. Invalid PCR results indicated by high cycle threshold (CT) values (CT ACTB > 33 (Triplex assay); CTmethylated allele > 33 and CTunmethylated allele > 33 (QM assay)) were omitted from the analysis.
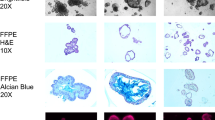
Immunohistochemical staining for MSI
Tumors with MSI are known for their hyper-mutated genome and epigenetic alternations [4]. To analyze SHOX2/SEPT9 in association with MSI, immunohistochemical staining (IHC) was used to estimate the protein expression levels of the four major mismatch repair enzymes (MLH1, PMS2, MSH2, and MSH6). For this purpose, tissue microarrays (TMA) were assembled from formalin-fixed, paraffin-embedded tissue. For each case (adenoma, carcinoma, control group), representative areas were marked on the hematoxylin-eosin-stained section. Subsequently, at least 1-mm cores were punched and arrayed in a paraffin block. IHC stainings were performed with a Ventana Benchmark-automated staining system (Ventana Medical Systems, Tucson, AZ, USA), following the manufactures’ protocol. The following antibodies from BD Pharmingen were used: MLH-1 #550838 clon G168-15 (1:50), MSH-2 #556349 mouse anti-human, MSH6 BD Pharmingen #610918 mouse anti-human, and PMS2 BD Pharmingen #556415 mouse monoclonal. The slides were then counterstained with hematoxylin, dehydrated, and mounted. Presence of mismatch repair enzymes was then evaluated by an experienced pathologist.
Availability of data and materials
The TCGA dataset supporting the conclusions of this article is available in the TCGA data repository (http://cancergenome.nih.gov/). The dataset supporting the conclusions of this article is included within the article and its figures.
Data evaluation and statistical analysis
Values are expressed as mean or median, unless otherwise stated. Differences between groups were tested using t test, Mann-Whitney U test, or ANOVA, where appropriate. Correlation between values was tested using Spearman’s rank correlation. The Bonferroni correction was used in case of multiple pairwise comparisons. Receiver operating characteristic (ROC) curves were calculated to observe the ability of the methylation level of SHOX2 and SEPT9 gene loci to differentiate between the subgroups. Areas under the curve (AUCs) were reported. p values of <0.05 were considered to be statistically significant. Statistical analyses were performed with SPSS (IBM, Armonk, NY, USA, version 23) and GraphPad Prism 4 (GraphPad Software Inc., San Diego, CA, USA).
References
Ferlay J, Shin H-R, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–917.
Jass JR. Classification of colorectal cancer based on correlation of clinical, morphological and molecular features. Histopathology. 2007;50:113–30.
Cho KR, Vogelstein B. Genetic alterations in the adenoma—carcinoma sequence. Cancer. 1992;70:1727–31.
Cancer Genome Atlas Network. Comprehensive molecular characterization of human colon and rectal cancer. Nature. 2012;487:330–7.
Fearon ER. Molecular genetics of colorectal cancer. Annu Rev Pathol. 2011;6:479–507.
Brenner H, Kloor M, Pox CP. Colorectal cancer. Lancet. 2014;383:1490–502.
Siegel R, DeSantis C, Virgo K, Stein K, Mariotto A, Smith T, et al. Cancer treatment and survivorship statistics, 2012. CA Cancer J Clin. 2012;62:220–41.
Murphy CC, Harlan LC, Lund JL, Lynch CF, Geiger AM. Patterns of colorectal cancer care in the United States: 1990–2010. J Natl Cancer Inst. 2015;107(10):djv198. doi:10.1093/jnci/djv198.
Arnold M, Sierra MS, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global patterns and trends in colorectal cancer incidence and mortality. Gut. 2016; doi:10.1136/gutjnl-2015-310912. [Epubahead of print].
Shapiro JA, Seeff LC, Thompson TD, Nadel MR, Klabunde CN, Vernon SW. Colorectal cancer test use from the 2005 National Health Interview Survey. Cancer Epidemiol Biomarkers Prev. 2008;17:1623–30.
Joseph DA, Meester RGS, Zauber AG, Manninen DL, Winges L, Dong FB, et al. Colorectal cancer screening: estimated future colonoscopy need and current volume and capacity. Cancer. 2016;122(16)2479–86.
Strum WB. Colorectal adenomas. N Engl J Med. 2016;374:1065–75.
Vogelstein B, Vogelstein B, Papadopoulos N, Papadopoulos N, Velculescu VE, Velculescu VE, et al. Cancer genome landscapes. Science. 2013;339:1546–58.
Mikeska T, Bock C, Do H, Dobrovic A. DNA methylation biomarkers in cancer: progress towards clinical implementation. Expert Rev Mol Diagn. 2012;12:473–87.
Dietrich D, Jung M, Puetzer S, Leisse A, Holmes EE, Meller S, et al. Diagnostic and prognostic value of SHOX2 and SEPT9 DNA methylation and cytology in benign, paramalignant and malignant pleural effusions. PLoS One. 2013;8:e84225.
Lofton-Day C, Model F, Devos T, Tetzner R, Distler J, Schuster M, et al. DNA methylation biomarkers for blood-based colorectal cancer screening. Clin Chem [Internet]. 2008;54:414–23. Available from: http://eutils.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&id=18089654&retmode=ref&cmd=prlinks.
Grützmann R, Molnar B, Pilarsky C, Habermann JK, Schlag PM, Saeger HD, et al. Sensitive detection of colorectal cancer in peripheral blood by septin 9 DNA methylation assay. PLoS ONE [Internet]. 2008;3:e3759. Available from: http://eutils.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&id=19018278&retmode=ref&cmd=prlinks.
Warren JD, Xiong W, Bunker AM, Vaughn CP, Furtado LV, Roberts WL, et al. Septin 9 methylated DNA is a sensitive and specific blood test for colorectal cancer. BMC Med. 2011;9:133.
Church TR, Wandell M, Lofton-Day C, Mongin SJ, Burger M, Payne SR, et al. Prospective evaluation of methylated SEPT9 in plasma for detection of asymptomatic colorectal cancer. Gut. 2014;63:317–25.
Toth K, Galamb O, Spisak S, Wichmann B, Sipos F, Valcz G, et al. The influence of methylated septin 9 gene on RNA and protein level in colorectal cancer. Pathol Oncol Res. 2011;17:503–9.
Wasserkort R, Kalmar A, Valcz G, Spisak S, Krispin M, Toth K, et al. Aberrant septin 9 DNA methylation in colorectal cancer is restricted to a single CpG island. BMC Cancer. 2013;13:398.
Toth K, Wasserkort R, Sipos F, Kalmar A, Wichmann B, Leiszter K, et al. Detection of methylated septin 9 in tissue and plasma of colorectal patients with neoplasia and the relationship to the amount of circulating cell-free DNA. PLoS One. 2014;9:e115415.
Tänzer M, Balluff B, Distler J, Hale K, Leodolter A, Röcken C, et al. Performance of epigenetic markers SEPT9 and ALX4 in plasma for detection of colorectal precancerous lesions. PLoS One. 2010;5:e9061.
Potter NT, Hurban P, White MN, Whitlock KD, Lofton-Day CE, Tetzner R, et al. Validation of a real-time PCR-based qualitative assay for the detection of methylated SEPT9 DNA in human plasma. Clin Chem. 2014;60:1183–91.
Sadanandam A, Lyssiotis CA, Homicsko K, Collisson EA, Gibb WJ, Wullschleger S, et al. A colorectal cancer classification system that associates cellular phenotype and responses to therapy. Nat Med. 2013;19:619–25.
Luo Y, Wong C-J, Kaz AM, Dzieciatkowski S, Carter KT, Morris SM, et al. Differences in DNA methylation signatures reveal multiple pathways of progression from adenoma to colorectal cancer. Gastroenterology. 2014;147:418–29.e8.
Blaschke RJ, Hahurij ND, Kuijper S, Just S, Wisse LJ, Deissler K, et al. Targeted mutation reveals essential functions of the homeodomain transcription factor Shox2 in sinoatrial and pacemaking development. Circulation. 2007;115:1830–8.
Song L, Yu H, Li Y. Diagnosis of lung cancer by SHOX2 gene methylation assay. Mol Diagn Ther. 2015;19:159–67.
Dietrich D, Kneip C, Raji O, Liloglou T, Seegebarth A, Schlegel T, et al. Performance evaluation of the DNA methylation biomarker SHOX2 for the aid in diagnosis of lung cancer based on the analysis of bronchial aspirates. Int J Oncol. 2012;40:825–32.
Zhao Q-T, Guo T, Wang H-E, Zhang X-P, Zhang H, Wang Z-K, et al. Diagnostic value of SHOX2 DNA methylation in lung cancer: a meta-analysis. Onco Targets Ther. 2015;8:3433–9.
Darwiche K, Zarogoulidis P, Baehner K, Welter S, Tetzner R, Wohlschlaeger J, et al. Assessment of SHOX2 methylation in EBUS-TBNA specimen improves accuracy in lung cancer staging. Ann Oncol. 2013;24:2866–70.
Kneip C, Schmidt B, Seegebarth A, Weickmann S, Fleischhacker M, Liebenberg V, et al. SHOX2 DNA methylation is a biomarker for the diagnosis of lung cancer in plasma. J Thorac Oncol. 2011;6:1632–8.
Dietrich D, Hasinger O, Liebenberg V, Field JK, Kristiansen G, Soltermann A. DNA methylation of the homeobox genes PITX2 and SHOX2 predicts outcome in non-small-cell lung cancer patients. Diagn Mol Pathol. 2012;21:93–104.
Schneider KU, Dietrich D, Fleischhacker M, Leschber G, Merk J, Schäper F, et al. Correlation of SHOX2 gene amplification and DNA methylation in lung cancer tumors. BMC Cancer. 2011;11:102.
Konecny M, Markus J, Waczulikova I, Dolesova L, Kozlova R, Repiska V, et al. The value of SHOX2 methylation test in peripheral blood samples used for the differential diagnosis of lung cancer and other lung disorders. Neoplasma. 2016;63(2):246–53.
Jung M, Pützer S, Gevensleben H, Meller S, Kristiansen G, Dietrich D. Diagnostic and prognostic value of SHOX2 and SEPT9 DNA methylation and cytology in benign, paramalignant, and malignant ascites. Clin Epigenetics. 2016;8:24.
Toll AD, Fabius D, Hyslop T, Pequignot E, DiMarino AJ, Infantolino A, et al. Prognostic significance of high-grade dysplasia in colorectal adenomas. Colorectal Dis. 2011;13:370–3.
Ladabaum U, Patel A, Mannalithara A, Sundaram V, Mitani A, Desai M. Predicting advanced neoplasia at colonoscopy in a diverse population with the National Cancer Institute colorectal cancer risk-assessment tool. Cancer. 2016;122(17):2663–70.
Jin P, Kang Q, Wang X, Yang L, Yu Y, Li N, et al. Performance of a second-generation methylated SEPT9 test in detecting colorectal neoplasm. J Gastroenterol Hepatol. 2015;30:830–3.
Timp W, Feinberg AP. Cancer as a dysregulated epigenome allowing cellular growth advantage at the expense of the host. Nat Rev Cancer. 2013;13:497–510.
Baylin SB, Jones PA. A decade of exploring the cancer epigenome—biological and translational implications. Nat Rev Cancer. 2011;11:726–34.
Yagi K, Takahashi H, Akagi K, Matsusaka K, Seto Y, Aburatani H, et al. Intermediate methylation epigenotype and its correlation to KRAS mutation in conventional colorectal adenoma. Am J Pathol. 2012;180:616–25.
Sakai E, Nakajima A, Kaneda A. Accumulation of aberrant DNA methylation during colorectal cancer development. World J Gastroenterol. 2014;20:978–87.
Grady WM, Carethers JM. Genomic and epigenetic instability in colorectal cancer pathogenesis. Gastroenterology. 2008;135:1079–99.
Ben-David E, Bester AC, Shifman S, Kerem B. Transcriptional dynamics in colorectal carcinogenesis: new insights into the role of c-Myc and miR17 in benign to cancer transformation. Cancer Res. 2014;74:5532–40.
Saha S, Bardelli A, Buckhaults P, Velculescu VE, Rago C, St Croix B, et al. A phosphatase associated with metastasis of colorectal cancer. Science. 2001;294:1343–6.
Bardelli A, Saha S, Sager JA, Romans KE, Xin B, Markowitz SD, et al. PRL-3 expression in metastatic cancers. Clin Cancer Res. 2003;9:5607–15.
Connolly D, Hoang HG, Adler E, Tazearslan C, Simmons N, Bernard VV, et al. Septin 9 amplification and isoform-specific expression in peritumoral and tumor breast tissue. Biol Chem. 2014;395:157–67.
Montagna C, Lyu M-S, Hunter K, Lukes L, Lowther W, Reppert T, et al. The Septin 9 (MSF) gene is amplified and overexpressed in mouse mammary gland adenocarcinomas and human breast cancer cell lines. Cancer Res. 2003;63:2179–87.
Zechmeister JR, Goldberg GL, Montagna C. Increased copy number of Septin 9 (SEPT9) in women with high grade endometrial adenocarcinoma (EMCA): is there a potential link to paclitaxel resistance. Cancer Res. 2014. doi:10.1158/1538-7445.
Devos T, Tetzner R, Model F, Weiss G, Schuster M, Distler J, et al. Circulating methylated SEPT9 DNA in plasma is a biomarker for colorectal cancer. Clin Chem [Internet]. 2009;55:1337–46. Available from: http://eutils.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&id=19406918&retmode=ref&cmd=prlinks.
Payne SR. From discovery to the clinic: the novel DNA methylation biomarker (m)SEPT9 for the detection of colorectal cancer in blood. Epigenomics. 2010;2:575–85.
Ørntoft M-BW, Nielsen HJ, Ørntoft TF, Andersen CL, Danish Study Group on Early Detection of Colorectal Cancer. Performance of the colorectal cancer screening marker Sept9 is influenced by age, diabetes and arthritis: a nested case-control study. BMC Cancer. 2015;15:819.
Carmona FJ, Azuara D, Berenguer-Llergo A, Fernandez AF, Biondo S, de Oca J, et al. DNA methylation biomarkers for noninvasive diagnosis of colorectal cancer. Cancer Prev Res (Phila). 2013;6:656–65.
Tapp HS, Commane DM, Bradburn DM, Arasaradnam R, Mathers JC, Johnson IT, et al. Nutritional factors and gender influence age-related DNA methylation in the human rectal mucosa. Aging Cell. 2013;12:148–55.
Bosman FT, World Health Organization, Carneiro F, International Agency for Research on Cancer, Hruban RH. WHO classification of tumours of the digestive system. Lyon: International Agency for Research on Cancer; 2010.
Sobin LH, Gospodarowicz MK, Wittekind C. TNM classification of malignant tumours. Hoboken: John Wiley & Sons; 2011.
Odze RD, Goldblum JR. Odze and Goldblum surgical pathology of the GI tract, liver, biliary tract and pancreas. 3rd ed. Philadelphia: Elsevier/Saunders; 2015. p. 621–42.
Conteduca V, Sansonno D, Russi S, Dammacco F. Precancerous colorectal lesions (review). Int J Oncol. 2013;43:973–84.
Lieberman DA. Clinical practice. Screening for colorectal cancer. N Engl J Med. 2009;361:1179–87.
Levine JS, Ahnen DJ. Clinical practice. Adenomatous polyps of the colon. N Engl J Med. 2006;355:2551–7.
Gao J, Aksoy BA, Dogrusoz U, Dresdner G, Gross B, Sumer SO, et al. Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci Signal. 2013;6:pl1.
Cerami E, Gao J, Dogrusoz U, Gross BE, Sumer SO, Aksoy BA, et al. The cBio cancer genomics portal: an open platform for exploring multidimensional cancer genomics data. Cancer Discov. 2012;2:401–4.
Beroukhim R, Mermel CH, Porter D, Wei G, Raychaudhuri S, Donovan J, et al. The landscape of somatic copy-number alteration across human cancers. Nature. 2010;463:899–905.
Jung M, Uhl B, Kristiansen G, Dietrich D. Bisulfite conversion of DNA from tissues, cell lines, buffy coat, FFPE tissues, microdissected cells, swabs, sputum, aspirates, lavages, effusions, plasma, serum, and urine. Methods Mol Biol (Clifton, N.J.). 2015; [Epub ahead of print].
Dietrich D, Uhl B, Sailer V, Holmes EE, Jung M, Meller S, et al. Improved PCR performance using template DNA from formalin-fixed and paraffin-embedded tissues by overcoming PCR inhibition. PLoS One. 2013;8:e77771.
Zeschnigk M, Böhringer S, Price EA, Onadim Z, Masshöfer L, Lohmann DR. A novel real-time PCR assay for quantitative analysis of methylated alleles (QAMA): analysis of the retinoblastoma locus. Nucleic Acids Res. 2004;32:e125.
Harbeck N, Nimmrich I, Hartmann A, Ross JS, Cufer T, Grützmann R, et al. Multicenter study using paraffin-embedded tumor tissue testing PITX2 DNA methylation as a marker for outcome prediction in tamoxifen-treated, node-negative breast cancer patients. J Clin Oncol. 2008;26:5036–42.
Acknowledgements
Not applicable.
Funding
This work was supported by a BONFOR (“Bonner Forschung”) Research Grant (O-1120051) provided to HM by the University Medical Center, University of Bonn, Bonn, Germany.
Availability of data and materials
The datasets supporting the conclusions of this article are included within the article. Additionally, TCGA datasets may be retrieved from http://cancergenome.nih.gov/.
Authors’ contributions
AS, HM, and DD drafted the manuscript and conceived and coordinated the study. GK, DP, and JCK participated in the design of the study and its supervision and revised the manuscript. AVE, SM, and DG provided and characterized the sample material. AS, VB, AVE, and VB performed the real-time PCR and the DNA preparations. All authors read and approved the final version of the manuscript.
Competing interests
DD has been employed by Epigenomics AG (Berlin, Germany) and is one of its shareholders. The company aims to commercialize DNA methylation markers. The other authors report to have no conflict of interest regarding the topic of the article.
Consent for publication
Not applicable.
Ethical approval
The study was approved by the Institutional Review Board (IRB) of the University Hospital of Bonn (Number: 222/13). All experiments were conducted in accordance with the Helsinki Declaration of 1975.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Semaan, A., van Ellen, A., Meller, S. et al. SEPT9 and SHOX2 DNA methylation status and its utility in the diagnosis of colonic adenomas and colorectal adenocarcinomas. Clin Epigenet 8, 100 (2016). https://doi.org/10.1186/s13148-016-0267-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13148-016-0267-5